Back

Poster Session C - Monday Afternoon
Category: Small Intestine
C0657 - Olmesartan-Induced Enteropathy With Associated Anti-Enterocyte Antibody
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- WB
William Bigelow, MD
University of Virginia Health System
Charlottesville, VA
Presenting Author(s)
William Bigelow, MD1, Mark Radlinski, MD2, Dennis Kumral, MD3, Andrew Copland, MD3
1University of Virginia Health System, Charlottesville, VA; 2University of Virginia, Charlottesville, VA; 3University of Virginia Digestive Health Center, Charlottesville, VA
Introduction: Olmesartan-induced enteropathy (OIE) is a well-described drug injury that presents with severe diarrhea and weight loss. The mechanism of injury is poorly understood though believed to involve immune-mediated enteropathy in addition to direct damage of intestinal epithelial cells. We describe a severe presentation of OIE with associated positive anti-enterocyte antibody.
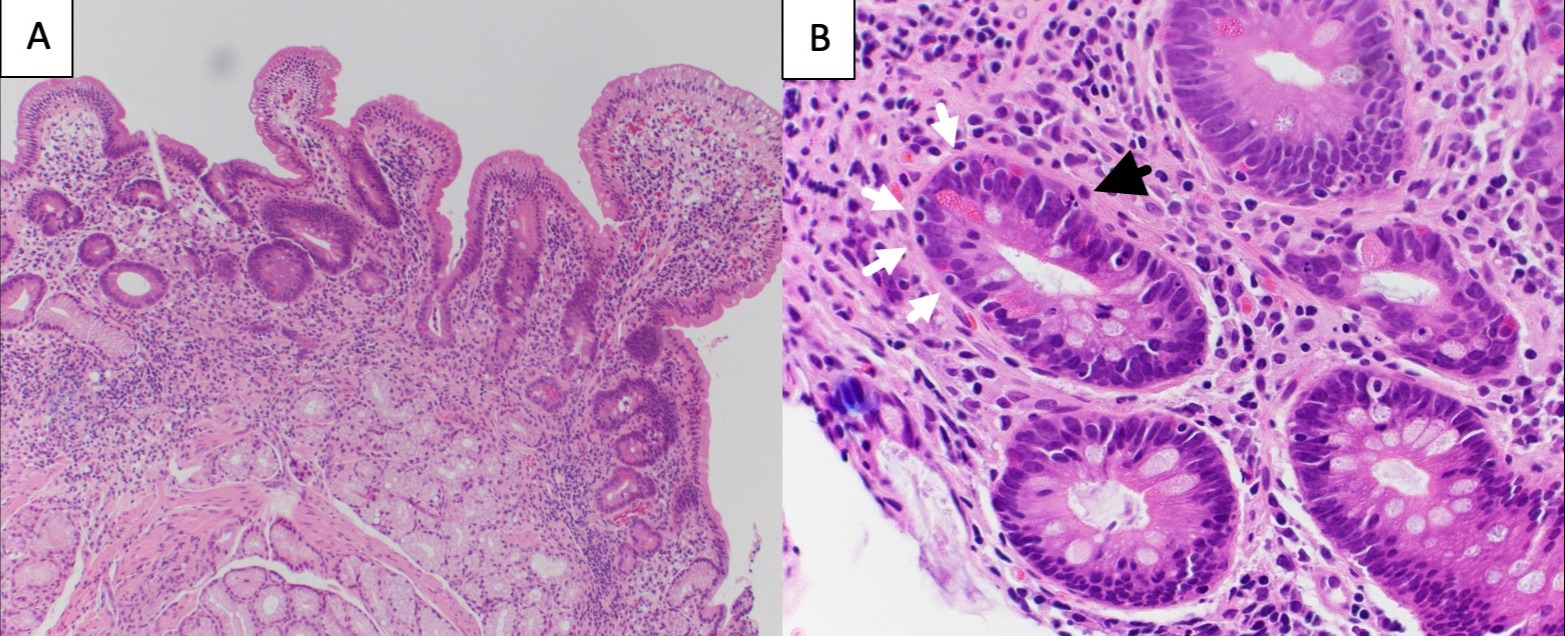
Case Description/Methods: A 74-year-old female presented with a seven month history of weight loss, diarrhea, nausea, and vomiting. Initial evaluation demonstrated a stool osmotic gap of 42 consistent with secretory diarrhea and negative celiac serologies. Cross-sectional imaging revealed extensive inflammation throughout the stomach and duodenum. A subsequent esophagogastroduodenoscopy (EGD) with biopsies revealed esophageal necrosis, active gastritis, and severe mucosal changes of atrophy and scalloping in the duodenum. Olmesartan for hypertension was held and she was started on twice daily IV PPI for the esophageal necrosis. Due to persistent and worsening symptoms over the following four weeks, she underwent a repeat EGD and was given IV steroids. Duodenal biopsy showed chronic duodenitis with villous blunting and scattered apoptotic epithelial cells compatible with Olmesartan-induced injury (Figure 1). Indirect immunofluorescence demonstrated IgG linear staining of apical membranes indicative of circulating anti-enterocyte antibodies. Diarrhea, weight loss, and difficulty with PO intake persisted the following two weeks despite steroid therapy and nutrition support with enteral access for tube feeds. She declined immunosuppressive agents or total parental nutrition and elected to discharge home on a steroid taper. Four months after discharge, she reported complete resolution of her diarrhea while on Budesonide and significant weight gain with both enteral feeds and PO intake.
Discussion: When OIE was first described, 3 of 19 patients were positive for anti-enterocyte antibody indicating potential association. These antibodies may circulate in a hyper-immune state such as the setting of Olmesartan use in certain individuals. The clinical presentation and histology of OIE and autoimmune enteropathy (AIE) are similar, which further supports an immune-related mechanism of injury in OIE. It is unclear if anti-enterocyte antibody presence indicates Olmesartan may cause AIE or is associated with OIE itself. We present this case to draw awareness to this relation and need for further investigation of the mechanism of injury in OIE.
Disclosures:
William Bigelow, MD1, Mark Radlinski, MD2, Dennis Kumral, MD3, Andrew Copland, MD3. C0657 - Olmesartan-Induced Enteropathy With Associated Anti-Enterocyte Antibody, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Virginia Health System, Charlottesville, VA; 2University of Virginia, Charlottesville, VA; 3University of Virginia Digestive Health Center, Charlottesville, VA
Introduction: Olmesartan-induced enteropathy (OIE) is a well-described drug injury that presents with severe diarrhea and weight loss. The mechanism of injury is poorly understood though believed to involve immune-mediated enteropathy in addition to direct damage of intestinal epithelial cells. We describe a severe presentation of OIE with associated positive anti-enterocyte antibody.
Case Description/Methods: A 74-year-old female presented with a seven month history of weight loss, diarrhea, nausea, and vomiting. Initial evaluation demonstrated a stool osmotic gap of 42 consistent with secretory diarrhea and negative celiac serologies. Cross-sectional imaging revealed extensive inflammation throughout the stomach and duodenum. A subsequent esophagogastroduodenoscopy (EGD) with biopsies revealed esophageal necrosis, active gastritis, and severe mucosal changes of atrophy and scalloping in the duodenum. Olmesartan for hypertension was held and she was started on twice daily IV PPI for the esophageal necrosis. Due to persistent and worsening symptoms over the following four weeks, she underwent a repeat EGD and was given IV steroids. Duodenal biopsy showed chronic duodenitis with villous blunting and scattered apoptotic epithelial cells compatible with Olmesartan-induced injury (Figure 1). Indirect immunofluorescence demonstrated IgG linear staining of apical membranes indicative of circulating anti-enterocyte antibodies. Diarrhea, weight loss, and difficulty with PO intake persisted the following two weeks despite steroid therapy and nutrition support with enteral access for tube feeds. She declined immunosuppressive agents or total parental nutrition and elected to discharge home on a steroid taper. Four months after discharge, she reported complete resolution of her diarrhea while on Budesonide and significant weight gain with both enteral feeds and PO intake.
Discussion: When OIE was first described, 3 of 19 patients were positive for anti-enterocyte antibody indicating potential association. These antibodies may circulate in a hyper-immune state such as the setting of Olmesartan use in certain individuals. The clinical presentation and histology of OIE and autoimmune enteropathy (AIE) are similar, which further supports an immune-related mechanism of injury in OIE. It is unclear if anti-enterocyte antibody presence indicates Olmesartan may cause AIE or is associated with OIE itself. We present this case to draw awareness to this relation and need for further investigation of the mechanism of injury in OIE.
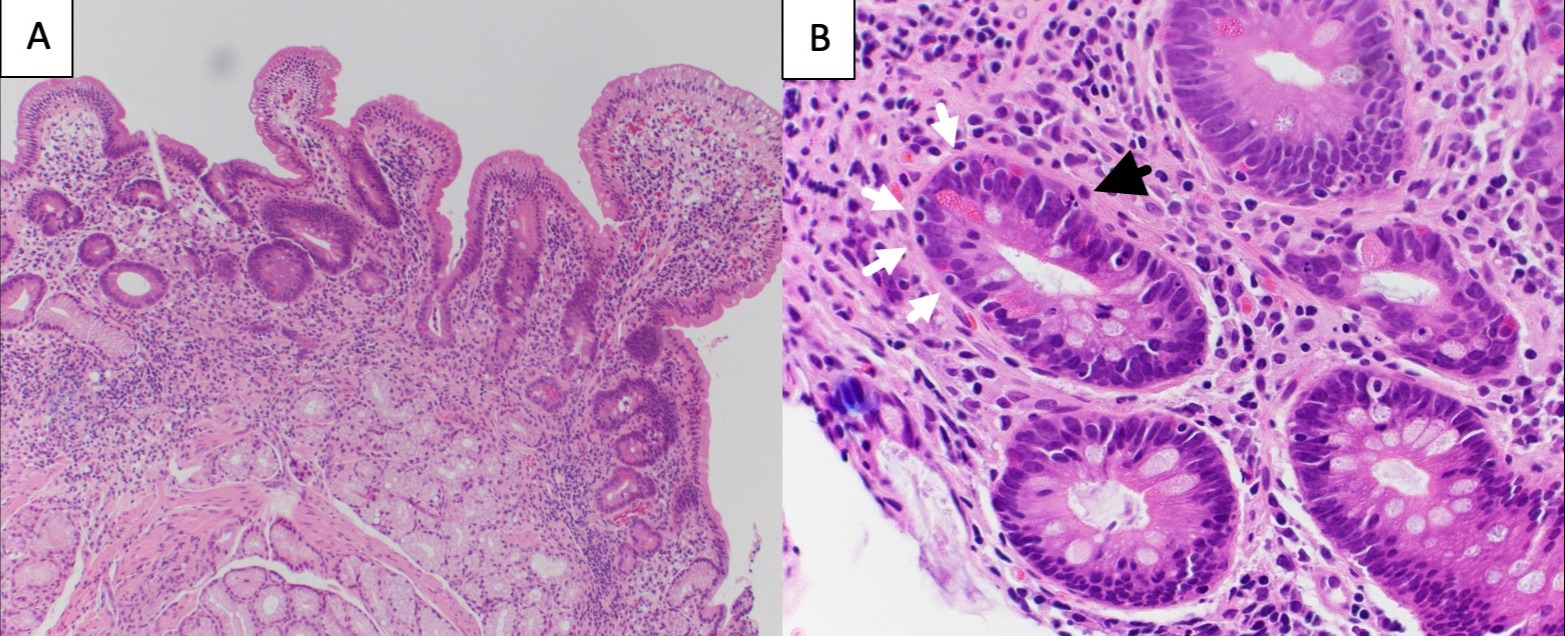
Figure: Figure 1. Panel A - The duodenal mucosa showed mild to moderate villus blunting and widening by an increased chronic inflammatory infiltrate in the lamina propria. (Hematoxylin and eosin stain, 100x original magnification). Panel B - There were scattered epithelial apoptotic bodies in the crypts (black arrow) and focal increase in intraepithelial lymphocytes (white arrows). (Hematoxylin & eosin stain, 400x original magnification).
Disclosures:
William Bigelow indicated no relevant financial relationships.
Mark Radlinski indicated no relevant financial relationships.
Dennis Kumral indicated no relevant financial relationships.
Andrew Copland indicated no relevant financial relationships.
William Bigelow, MD1, Mark Radlinski, MD2, Dennis Kumral, MD3, Andrew Copland, MD3. C0657 - Olmesartan-Induced Enteropathy With Associated Anti-Enterocyte Antibody, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
