Back

Poster Session C - Monday Afternoon
Category: Colon
C0113 - Plasmacytomas and Polyps: A Perplexing Presentation
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- TM
Thomas J. Mathews, MD
University of Kansas Medical Center
Kansas City, KS
Presenting Author(s)
Thomas J. Mathews, MD, Mark Cunningham, MD, John A. Bonino, MD
University of Kansas Medical Center, Kansas City, KS
Introduction: Plasmacytomas are rare tumors involving plasma cells that arise from either bone or mucosal surfaces throughout the body. These are generally classified as either bone plasmacytomas or extramedullary lesions. Extramedullary lesions can occur in organs or soft tissues and are thought to be a manifestation of hematogenous dissemination. Extramedullary plasmacytomas (EMPs) make up less than 5% of all plasma cell tumors, and when identified are usually located in the respiratory tract. Gastrointestinal involvement has been reported to be extremely rare.
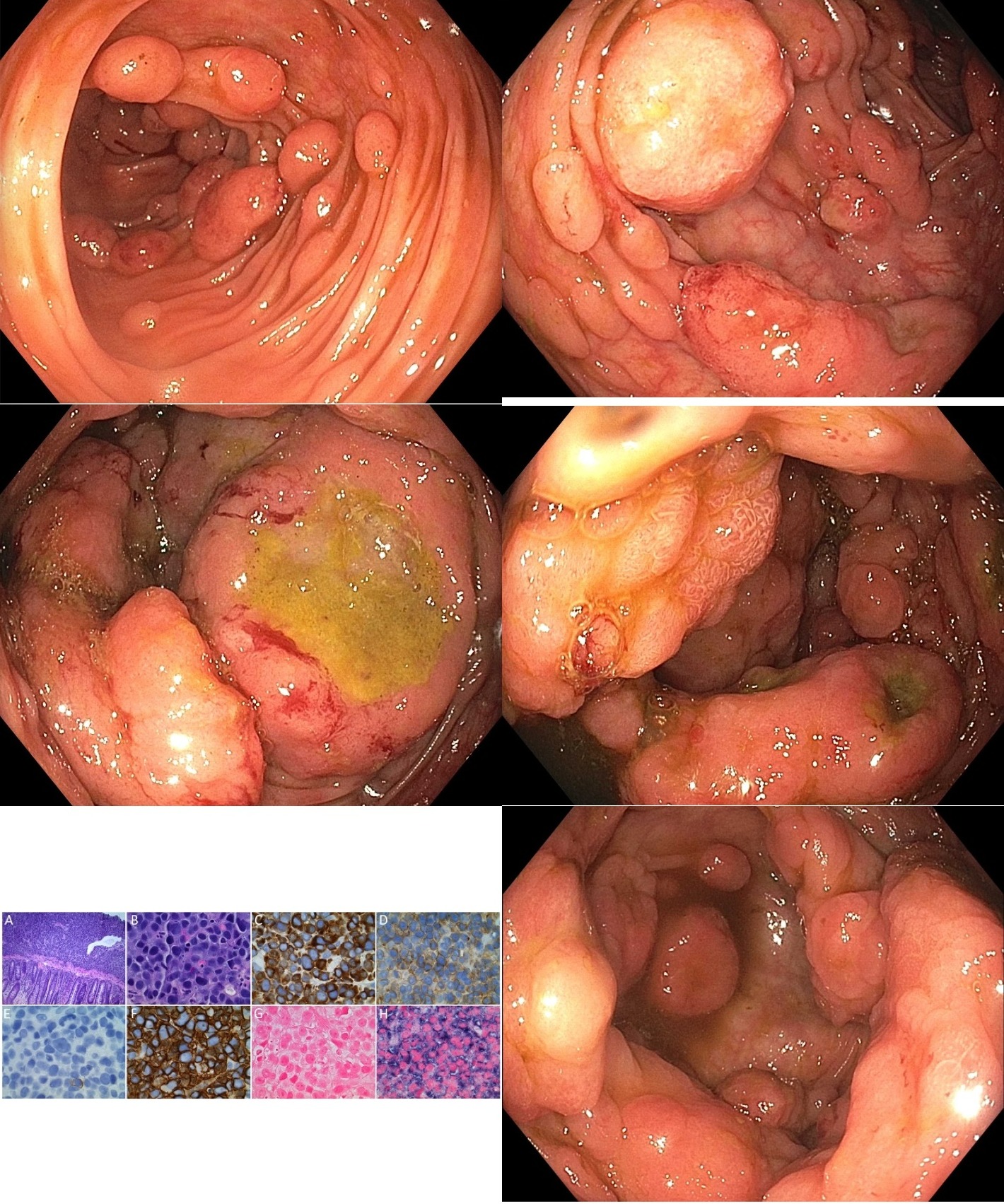
Case Description/Methods: An 80-year-old male with history of acute lymphoid leukemia, multiple myeloma (MM), and pancytopenia (secondary to chemotherapy) was admitted for acute renal failure. The patient reported diarrhea and increasing fatigue over the previous several weeks. Stool evaluation for infectious etiologies was unrevealing. Labs demonstrated significantly increased fLLC of 974 (fKLC 0.08), as well as decreased IgG, IgA, and IgM. Serum protein electrophoresis demonstrated an IgG lambda paraprotein spike, suggestive of MM relapse. A CT scan of the abdomen and pelvis demonstrated irregular thickening of the cecum and ascending colon. A colonoscopy was performed and revealed innumerable large polypoid masses throughout the colon. The mass burden predominated in the cecum and ascending colon. Many of the masses had large ulcerations, up to 2 cm in diameter. Biopsies were obtained confirming plasma cell neoplasia.
Discussion: The incidence of EMPs at the time of diagnosis of MM is 7 to 18% and up to 20% at relapse. EMPs may be more frequent after treatment with novel agents, but this remains to be proven. Mechanisms of extramedullary spread may include decreased adhesion molecule expression and downregulation of chemokine receptors. Current and future studies will focus on the mechanisms of myeloma cell adhesion, myeloma growth at extramedullary sites, and drug sensitivity. Gastrointestinal EMPs have rarely been reported in the medical literature. Colonic involvement has been even more rarely described, with less than a handful of cases described with the diffuse nature and burden of colonic disease as seen in our patient. Our case demonstrates the need for clinicians to consider colonic plasmacytoma as a contributing etiology for patients presenting with chronic diarrhea, a negative infectious workup, and history of either active or past multiple myeloma.
Disclosures:
Thomas J. Mathews, MD, Mark Cunningham, MD, John A. Bonino, MD. C0113 - Plasmacytomas and Polyps: A Perplexing Presentation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Kansas Medical Center, Kansas City, KS
Introduction: Plasmacytomas are rare tumors involving plasma cells that arise from either bone or mucosal surfaces throughout the body. These are generally classified as either bone plasmacytomas or extramedullary lesions. Extramedullary lesions can occur in organs or soft tissues and are thought to be a manifestation of hematogenous dissemination. Extramedullary plasmacytomas (EMPs) make up less than 5% of all plasma cell tumors, and when identified are usually located in the respiratory tract. Gastrointestinal involvement has been reported to be extremely rare.
Case Description/Methods: An 80-year-old male with history of acute lymphoid leukemia, multiple myeloma (MM), and pancytopenia (secondary to chemotherapy) was admitted for acute renal failure. The patient reported diarrhea and increasing fatigue over the previous several weeks. Stool evaluation for infectious etiologies was unrevealing. Labs demonstrated significantly increased fLLC of 974 (fKLC 0.08), as well as decreased IgG, IgA, and IgM. Serum protein electrophoresis demonstrated an IgG lambda paraprotein spike, suggestive of MM relapse. A CT scan of the abdomen and pelvis demonstrated irregular thickening of the cecum and ascending colon. A colonoscopy was performed and revealed innumerable large polypoid masses throughout the colon. The mass burden predominated in the cecum and ascending colon. Many of the masses had large ulcerations, up to 2 cm in diameter. Biopsies were obtained confirming plasma cell neoplasia.
Discussion: The incidence of EMPs at the time of diagnosis of MM is 7 to 18% and up to 20% at relapse. EMPs may be more frequent after treatment with novel agents, but this remains to be proven. Mechanisms of extramedullary spread may include decreased adhesion molecule expression and downregulation of chemokine receptors. Current and future studies will focus on the mechanisms of myeloma cell adhesion, myeloma growth at extramedullary sites, and drug sensitivity. Gastrointestinal EMPs have rarely been reported in the medical literature. Colonic involvement has been even more rarely described, with less than a handful of cases described with the diffuse nature and burden of colonic disease as seen in our patient. Our case demonstrates the need for clinicians to consider colonic plasmacytoma as a contributing etiology for patients presenting with chronic diarrhea, a negative infectious workup, and history of either active or past multiple myeloma.
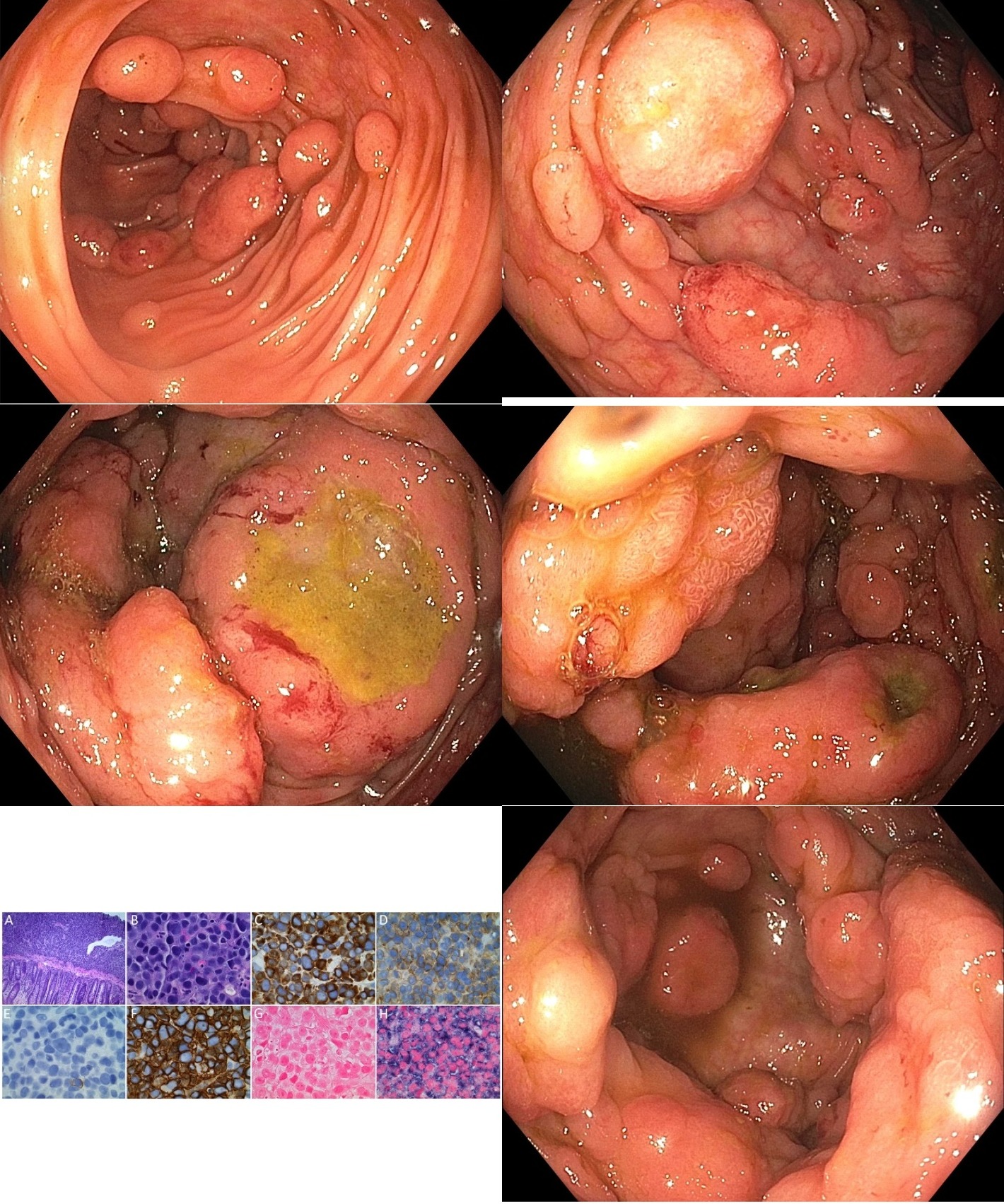
Figure: Histology slides: CD3 – positive multiple myeloma involving the colon in an 80 year old male.
A – B, Atypical large cell proliferation involving the mucosa and submucosa of the right colon. The malignant cells are positive for CD3 (C), CD4 (D), CD138 (F), and lambda light chain (H). The malignant cells are negative for CD20 (E), and kappa light chains (G). (A: H&E stain 100x magnification; B: H&E stain 1000x magnification; C – F; immunohistochemical stains 1000x magnification; G – H: chromogenic in-situ hybridization stains 1000x magnification).
A – B, Atypical large cell proliferation involving the mucosa and submucosa of the right colon. The malignant cells are positive for CD3 (C), CD4 (D), CD138 (F), and lambda light chain (H). The malignant cells are negative for CD20 (E), and kappa light chains (G). (A: H&E stain 100x magnification; B: H&E stain 1000x magnification; C – F; immunohistochemical stains 1000x magnification; G – H: chromogenic in-situ hybridization stains 1000x magnification).
Disclosures:
Thomas Mathews indicated no relevant financial relationships.
Mark Cunningham indicated no relevant financial relationships.
John Bonino indicated no relevant financial relationships.
Thomas J. Mathews, MD, Mark Cunningham, MD, John A. Bonino, MD. C0113 - Plasmacytomas and Polyps: A Perplexing Presentation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
