Back

Poster Session C - Monday Afternoon
Category: Small Intestine
C0671 - Disseminated Histoplasmosis Causing Peritoneal Implants in Patient Receiving Tumor Necrosis Factor-Alpha Inhibitor
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Sarah Grebennikov, DO
OhioHealth Riverside Methodist Hospital
Columbus, OH
Presenting Author(s)
Sarah Grebennikov, DO1, Cierra Smith, DO1, David Y. Lo, MD, FACG2, Jay Anderson, DO1
1OhioHealth Riverside Methodist Hospital, Columbus, OH; 2Ohio Gastroenterology Group, Inc, and The Ohio State University College of Medicine, Columbus, OH
Introduction: Histoplasmosis is an endemic mycosis commonly found in the Ohio River valley and presents with various clinical presentations ranging from asymptomatic to disseminated disease. Most patients present with pulmonary symptoms, while the immunocompromised subset can have multiple organ involvement with varying symptomology. An increasing number of patients are being treated with tumor necrosis factor (TNF)-alpha inhibitors, which dampens immune response and puts these patients at risk of opportunistic infections. We report a rare presentation of disseminated peritoneal histoplasmosis initially mimicking peritoneal carcinomatosis in a patient with rheumatoid arthritis on a TNF-alpha inhibitor.
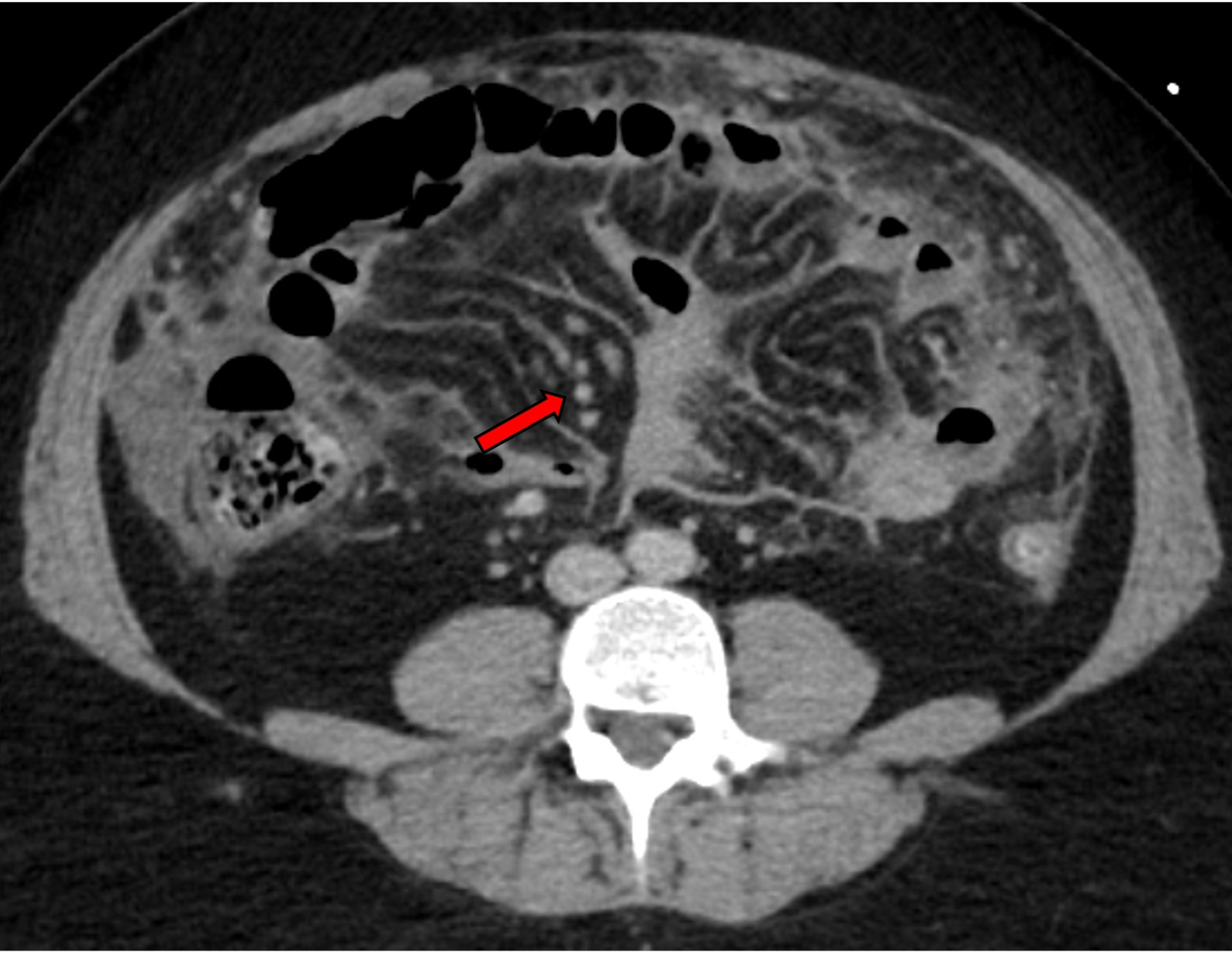
Case Description/Methods: A 43-year-old female with known history of rheumatoid arthritis (RA) on leflunomide, infliximab, and recent steroid course presented to the ED for abdominal pain and shortness of breath. On admission, the patient was febrile, tachycardic, and required supplemental oxygen. CT chest/abdomen/pelvis demonstrated right-sided pleural effusion, diffuse mesenteric nodules along the anterior abdominal wall concerning for malignancy, and moderate ascites (Figure A). Tumor marker CA 125 was elevated at 341 U/mL and surgical oncology was consulted for diagnostic laparoscopy with drainage of ascites, which was initially concerning for peritoneal carcinomatosis. Surprisingly, the biopsy revealed chronic inflammation, granulomas, and fungal yeast cells with morphological features consistent with histoplasmosis. She underwent thoracentesis, and pleural studies were consistent with exudative effusion with lymphocyte predominance, and cultures confirmed histoplasmosis. Initial broad antibiotic therapy for sepsis of unknown origin was transitioned to itraconazole and she was eventually discharged. More than a year after hospitalization, she remains on itraconazole due to persistent histoplasmosis. Her RA treatment was switched to upadacitinib, with some control of her symptoms.
Discussion: Diagnosis of histoplasmosis can be challenging because of its heterogeneous presentation. Disseminated histoplasmosis with peritoneal implants is exceeding rare, and most cases have been reported in ESRD patients on continuous peritoneal dialysis. Other cases of peritoneal histoplasmosis have been reported in immunosuppressed patients, which mimicked pathologies such as malignancy and IBD. It is essential to be vigilant of uncommon presentations of common disease, especially in immunocompromised patients.
Disclosures:
Sarah Grebennikov, DO1, Cierra Smith, DO1, David Y. Lo, MD, FACG2, Jay Anderson, DO1. C0671 - Disseminated Histoplasmosis Causing Peritoneal Implants in Patient Receiving Tumor Necrosis Factor-Alpha Inhibitor, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1OhioHealth Riverside Methodist Hospital, Columbus, OH; 2Ohio Gastroenterology Group, Inc, and The Ohio State University College of Medicine, Columbus, OH
Introduction: Histoplasmosis is an endemic mycosis commonly found in the Ohio River valley and presents with various clinical presentations ranging from asymptomatic to disseminated disease. Most patients present with pulmonary symptoms, while the immunocompromised subset can have multiple organ involvement with varying symptomology. An increasing number of patients are being treated with tumor necrosis factor (TNF)-alpha inhibitors, which dampens immune response and puts these patients at risk of opportunistic infections. We report a rare presentation of disseminated peritoneal histoplasmosis initially mimicking peritoneal carcinomatosis in a patient with rheumatoid arthritis on a TNF-alpha inhibitor.
Case Description/Methods: A 43-year-old female with known history of rheumatoid arthritis (RA) on leflunomide, infliximab, and recent steroid course presented to the ED for abdominal pain and shortness of breath. On admission, the patient was febrile, tachycardic, and required supplemental oxygen. CT chest/abdomen/pelvis demonstrated right-sided pleural effusion, diffuse mesenteric nodules along the anterior abdominal wall concerning for malignancy, and moderate ascites (Figure A). Tumor marker CA 125 was elevated at 341 U/mL and surgical oncology was consulted for diagnostic laparoscopy with drainage of ascites, which was initially concerning for peritoneal carcinomatosis. Surprisingly, the biopsy revealed chronic inflammation, granulomas, and fungal yeast cells with morphological features consistent with histoplasmosis. She underwent thoracentesis, and pleural studies were consistent with exudative effusion with lymphocyte predominance, and cultures confirmed histoplasmosis. Initial broad antibiotic therapy for sepsis of unknown origin was transitioned to itraconazole and she was eventually discharged. More than a year after hospitalization, she remains on itraconazole due to persistent histoplasmosis. Her RA treatment was switched to upadacitinib, with some control of her symptoms.
Discussion: Diagnosis of histoplasmosis can be challenging because of its heterogeneous presentation. Disseminated histoplasmosis with peritoneal implants is exceeding rare, and most cases have been reported in ESRD patients on continuous peritoneal dialysis. Other cases of peritoneal histoplasmosis have been reported in immunosuppressed patients, which mimicked pathologies such as malignancy and IBD. It is essential to be vigilant of uncommon presentations of common disease, especially in immunocompromised patients.
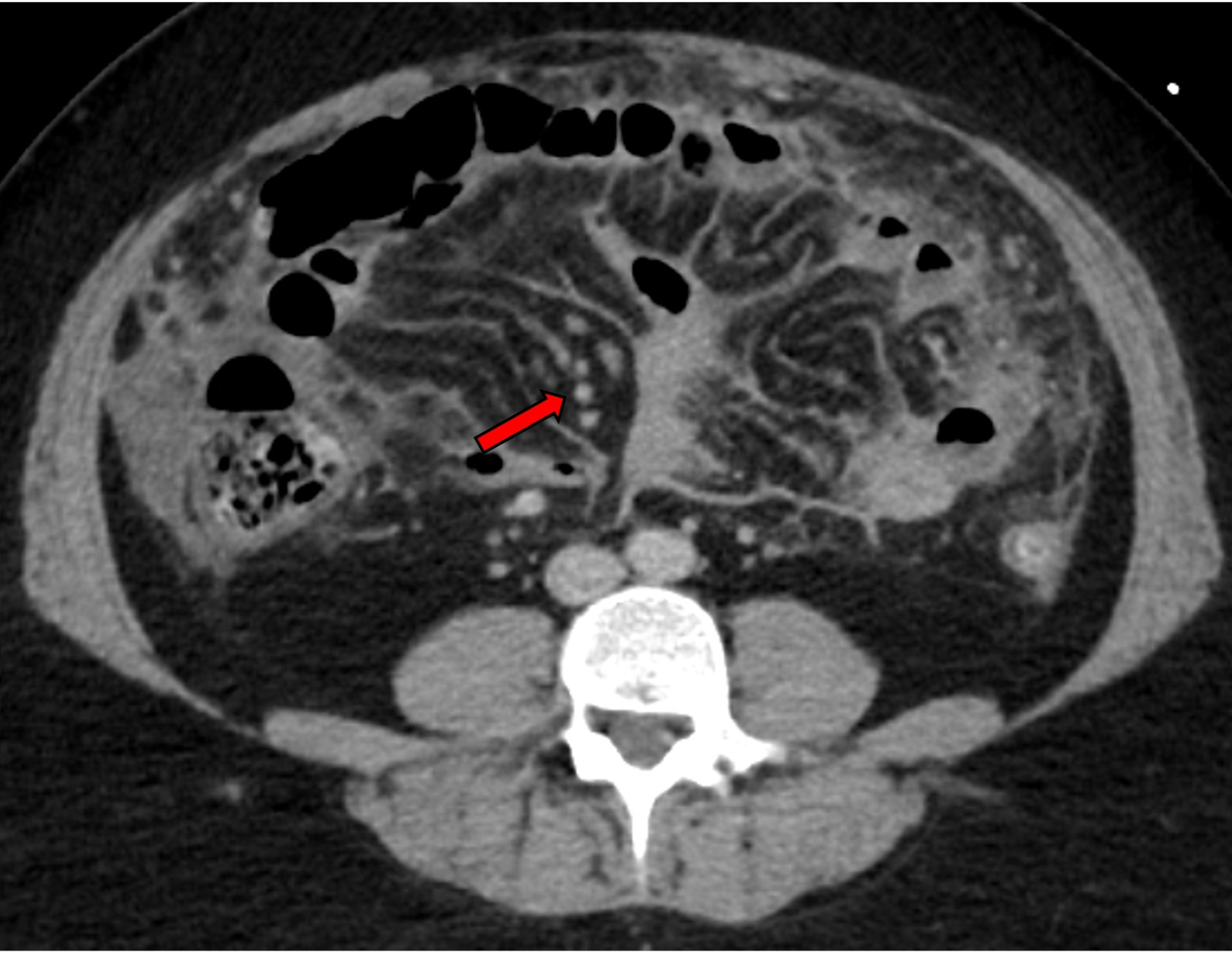
Figure: Figure 1: Diffuse nodularity to the mesentery most prevalent along anterior abdominal wall right paracolic gutter regions concerning for metastatic disease to the mesentery (Arrow). Mild bowel wall thickening seen involving descending colon.
Disclosures:
Sarah Grebennikov indicated no relevant financial relationships.
Cierra Smith indicated no relevant financial relationships.
David Lo indicated no relevant financial relationships.
Jay Anderson indicated no relevant financial relationships.
Sarah Grebennikov, DO1, Cierra Smith, DO1, David Y. Lo, MD, FACG2, Jay Anderson, DO1. C0671 - Disseminated Histoplasmosis Causing Peritoneal Implants in Patient Receiving Tumor Necrosis Factor-Alpha Inhibitor, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
