Back

Poster Session B - Monday Morning
Category: Stomach
B0703 - Gastropericardial Fistula as a Complication of a Perforated Marginal Ulcer in a Patient With Roux-en-Y Gastric Bypass Surgery
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- RJ
Ravi Jariwala, MD
Ochsner Clinic Foundation
New Orleans, Louisiana
Presenting Author(s)
Ravi Jariwala, MD1, John A. Evans, MD, MSc2
1Ochsner Clinic Foundation, New Orleans, LA; 2Ochsner Medical Center, New Orleans, LA
Introduction: Gastropericardial fistula is a rare occurrence. The most common risk factor for non-traumatic pneumopericardium or gastropericardial fistula is a gastroesophageal surgery such as a Nissen Fundoplication; however, it is also seen with perforation of malignant or benign gastric ulcers (1,2,3). Here we report a gastropericardial fistula presenting with hydropneumopericardium in a patient with a perforation of a marginal ulcer (MU) after laparoscopic Roux en Y gastric bypass (LRYGB) in the setting of excessive NSAID use.
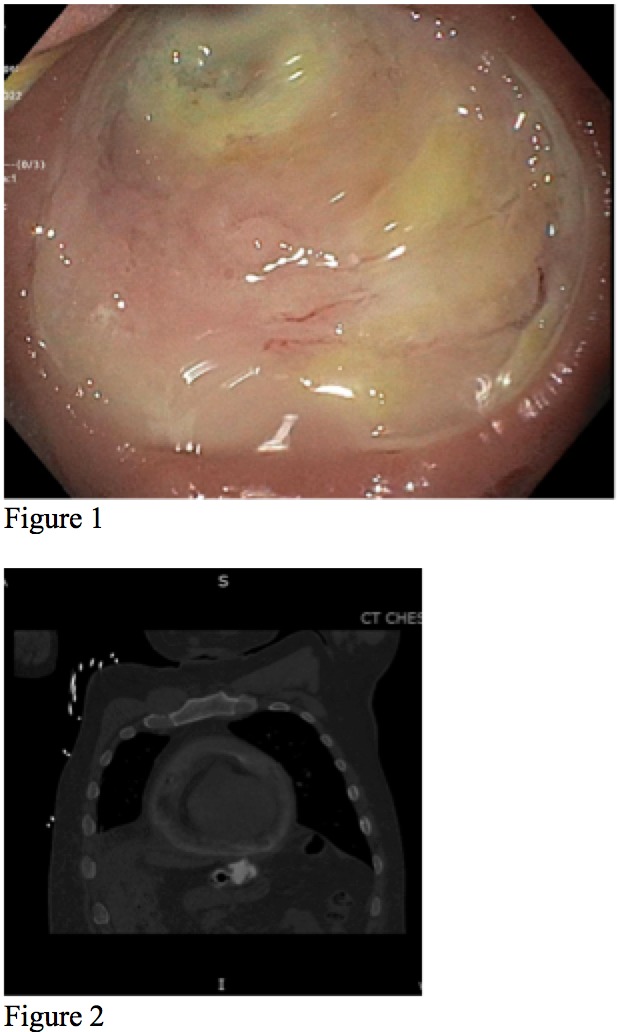
Case Description/Methods: A 48-year-old gentleman 13 years out from an uncomplicated LRYGB had an EGD for abdominal pain after chronic NSAID use and anemia. He was found to have a gastrojejunal (GJ) anastomosis ulcer. Random stomach biopsies were negative for H pylori. Care was taken to avoid biopsy of the ulcer. The patient was prescribed high dose, twice daily PPI with plans for repeat EGD in 8 weeks.
10 days later, he presented to the ED with shortness of breath and chest pain. Vital signs upon arrival were notable for heart rate in the 110s but otherwise unremarkable. Labs were remarkable for leukocytosis 18,000 cells per liter, hemoglobin 10 g/dl, BNP 500 ng/l, and normal troponin. Initial CT chest without contrast demonstrated pericardial effusion with associated pneumomediastinum. The subsequent CT chest with oral contrast had findings of a hydropneumopericardium and large amount of oral contrast within the dependent portion of the pericardial sac. A fistula from the pericardial sac to the GJ anastomosis was seen. An echocardiogram demonstrated a very echodense large circumferential pericardial effusion suspicious for food. The patient went to the operating room and underwent pericardiectomy and reconstruction of the prior gastrojejunostomy.
Discussion: This case demonstrates a rare development of gastropericardial fistula in a LRYGB patient taking NSAIDs causing a MU and subsequent perforation. The mainstays of conservative therapy for MU in RYGB patients include twice daily high dose PPI or H2 antagonist and sucralfate as well as avoidance of NSAIDs (4). A systematic review by Coblijn et al discusses that of 67.9% of patients (N=801) presenting with MU (including those with perforation) after RYGB utilized conservative therapy as mentioned above (5). Alternative options include revisional surgery or radiology assisted drainage, which is typically reserved for recalcitrant ulcers, perforation, fistula development, or dilated pouch (6).
Disclosures:
Ravi Jariwala, MD1, John A. Evans, MD, MSc2. B0703 - Gastropericardial Fistula as a Complication of a Perforated Marginal Ulcer in a Patient With Roux-en-Y Gastric Bypass Surgery, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Ochsner Clinic Foundation, New Orleans, LA; 2Ochsner Medical Center, New Orleans, LA
Introduction: Gastropericardial fistula is a rare occurrence. The most common risk factor for non-traumatic pneumopericardium or gastropericardial fistula is a gastroesophageal surgery such as a Nissen Fundoplication; however, it is also seen with perforation of malignant or benign gastric ulcers (1,2,3). Here we report a gastropericardial fistula presenting with hydropneumopericardium in a patient with a perforation of a marginal ulcer (MU) after laparoscopic Roux en Y gastric bypass (LRYGB) in the setting of excessive NSAID use.
Case Description/Methods: A 48-year-old gentleman 13 years out from an uncomplicated LRYGB had an EGD for abdominal pain after chronic NSAID use and anemia. He was found to have a gastrojejunal (GJ) anastomosis ulcer. Random stomach biopsies were negative for H pylori. Care was taken to avoid biopsy of the ulcer. The patient was prescribed high dose, twice daily PPI with plans for repeat EGD in 8 weeks.
10 days later, he presented to the ED with shortness of breath and chest pain. Vital signs upon arrival were notable for heart rate in the 110s but otherwise unremarkable. Labs were remarkable for leukocytosis 18,000 cells per liter, hemoglobin 10 g/dl, BNP 500 ng/l, and normal troponin. Initial CT chest without contrast demonstrated pericardial effusion with associated pneumomediastinum. The subsequent CT chest with oral contrast had findings of a hydropneumopericardium and large amount of oral contrast within the dependent portion of the pericardial sac. A fistula from the pericardial sac to the GJ anastomosis was seen. An echocardiogram demonstrated a very echodense large circumferential pericardial effusion suspicious for food. The patient went to the operating room and underwent pericardiectomy and reconstruction of the prior gastrojejunostomy.
Discussion: This case demonstrates a rare development of gastropericardial fistula in a LRYGB patient taking NSAIDs causing a MU and subsequent perforation. The mainstays of conservative therapy for MU in RYGB patients include twice daily high dose PPI or H2 antagonist and sucralfate as well as avoidance of NSAIDs (4). A systematic review by Coblijn et al discusses that of 67.9% of patients (N=801) presenting with MU (including those with perforation) after RYGB utilized conservative therapy as mentioned above (5). Alternative options include revisional surgery or radiology assisted drainage, which is typically reserved for recalcitrant ulcers, perforation, fistula development, or dilated pouch (6).
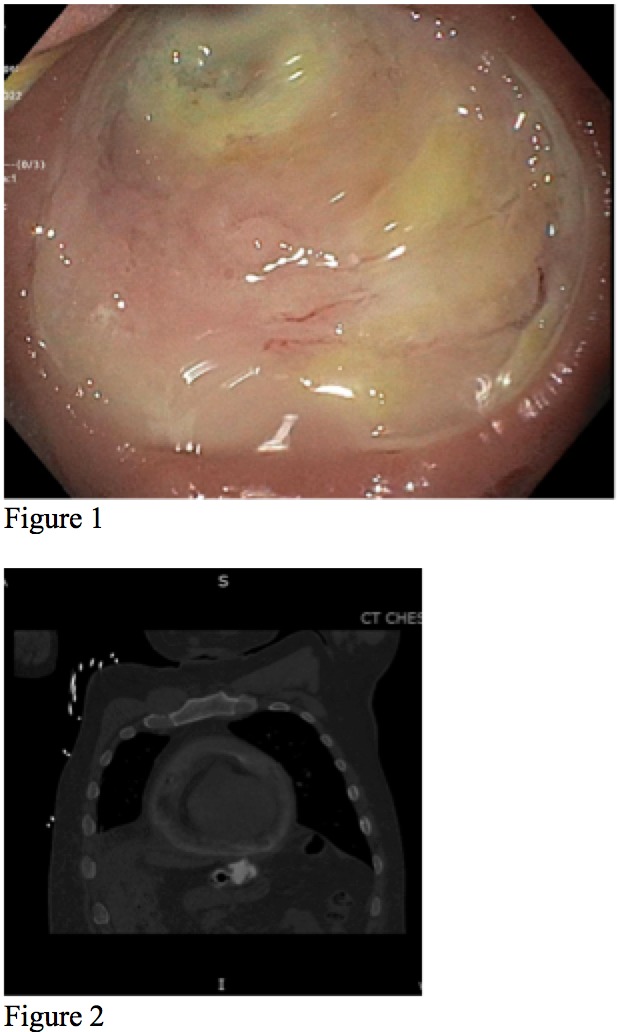
Figure: Figure 1. Endoscopic view of gastrojejunal anastomosis ulceration.
Figure 2. Coronal view of gastropericardial fistula with oral contrast extravasation into pericardium.
Figure 2. Coronal view of gastropericardial fistula with oral contrast extravasation into pericardium.
Disclosures:
Ravi Jariwala indicated no relevant financial relationships.
John Evans indicated no relevant financial relationships.
Ravi Jariwala, MD1, John A. Evans, MD, MSc2. B0703 - Gastropericardial Fistula as a Complication of a Perforated Marginal Ulcer in a Patient With Roux-en-Y Gastric Bypass Surgery, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
