Back

Poster Session C - Monday Afternoon
Category: Small Intestine
C0676 - A Case of Mycobacterial Infection Causing Necrotizing Granulomas of the Gastrointestinal Tract and Retroperitoneal Lymphadenopathy
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Alexis Bejcek, MD
Baylor Scott and White Medical Center
Temple, TX
Presenting Author(s)
Alexis Bejcek, MD1, Adam Patrick, BS2, Namisha Thapa, DO1, Nada Mohamed, MD1, Christopher Naumann, MD1
1Baylor Scott and White Medical Center, Temple, TX; 2Texas A&M College of Medicine, Temple, TX
Introduction: Various species of Mycobacterium, best known for their role in causing pulmonary tuberculosis, have rarely been described in gastrointestinal disease. Historically, Mycobacterium avium and Mycobacterium paratuberculosis have been found in tissue samples in patients with terminal ileitis, and have previously been described in patients with Crohn’s disease. Our study describes a rare case of mycobacterial infection with intestinal involvement.
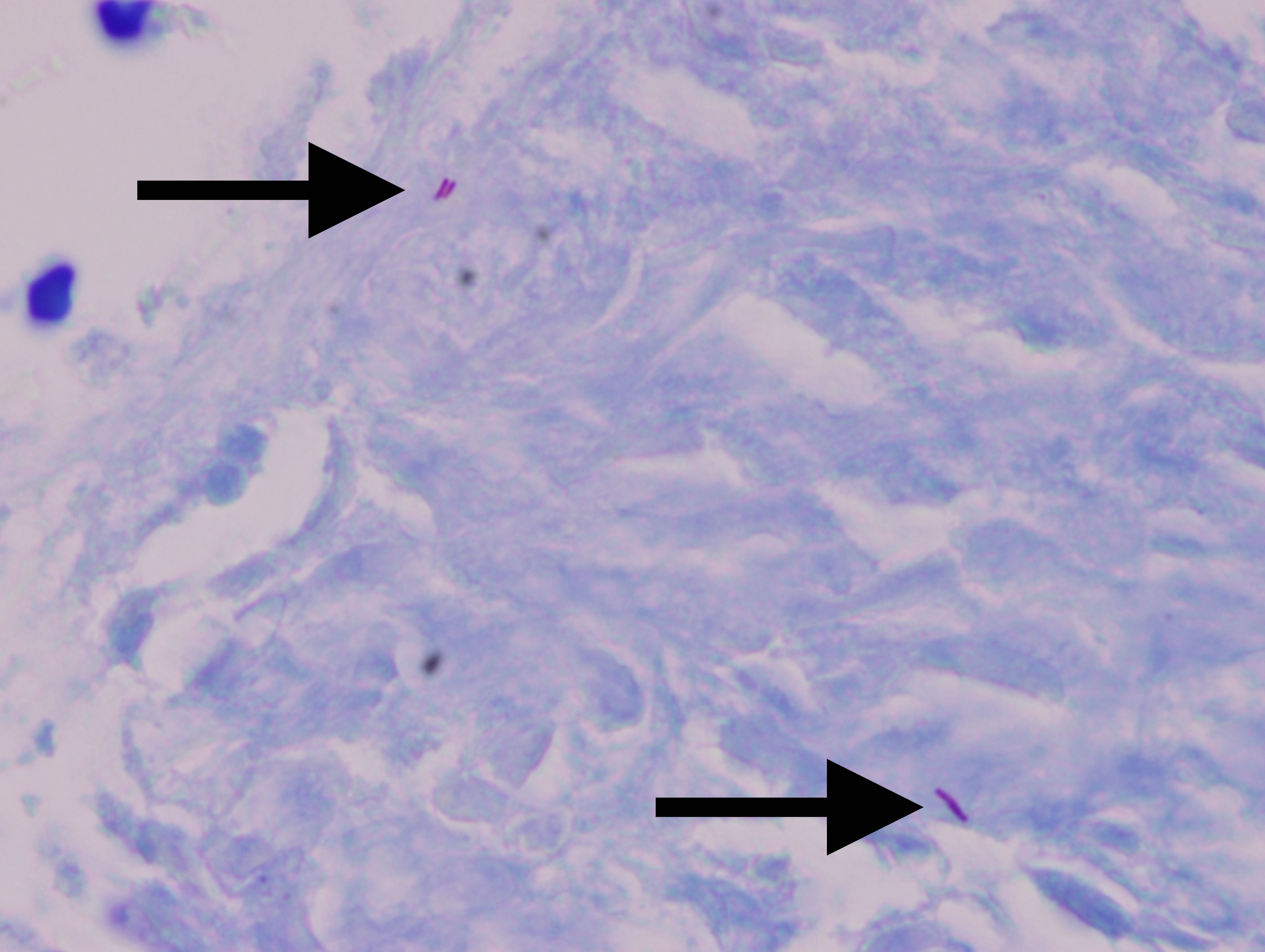
Case Description/Methods: A 44-year-old female with a history of ankylosing spondylitis treated with adalimumab and travel to Mexico 2 years ago endorsed 5 weeks of worsening epigastric pain, unintentional weight loss, diarrhea, and arthralgias during an outpatient visit. Review of computed tomography scans 3 and 10 years prior described prominent retroperitoneal lymph nodes. She was referred to interventional radiology for lymph node biopsy which revealed necrotizing granulomatous lymphadenitis. She was admitted to the hospital and computed tomography was notable for mural thickening and inflammatory stranding of the distal small bowel, particularly the terminal ileum. Esophagogastroduodenoscopy appeared normal. Colonoscopy displayed an edematous ileocecal valve and terminal ileum with ulcers as well as erosions of the cecum and proximal ascending colon. Biopsy of the ileum demonstrated necrotizing granulomatous inflammation and biopsy of the colon was consistent with focal poorly formed granulomatous inflammation. Mycobacterium PCR and staining of the duodenal biopsy was positive for acid-fast bacilli (see figure). The Mycobacterium polymerase chain reaction testing on the same duodenal sample was negative. Serum interferon-gamma release assay was positive. She was started on rifampin, isoniazid, pyrazinamide, and ethambutol to be taken for 2 months with plan to take an additional 7 months of rifampin and isoniazid. She experienced improvement in abdominal pain after initiation of antibiotic therapy.
Discussion: Granulomatous ileitis or other intestinal manifestations of Mycobacterium species are rare, and have been previously described in the Crohn’s disease population. This case of Mycobacterium infection represents an unusual etiology for intestinal inflammation and erosions in a patient with an autoimmune condition but without known Crohn’s disease. This case highlights the importance of including mycobacterial diseases within the differential for gastrointestinal tract lesions.
Disclosures:
Alexis Bejcek, MD1, Adam Patrick, BS2, Namisha Thapa, DO1, Nada Mohamed, MD1, Christopher Naumann, MD1. C0676 - A Case of Mycobacterial Infection Causing Necrotizing Granulomas of the Gastrointestinal Tract and Retroperitoneal Lymphadenopathy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Baylor Scott and White Medical Center, Temple, TX; 2Texas A&M College of Medicine, Temple, TX
Introduction: Various species of Mycobacterium, best known for their role in causing pulmonary tuberculosis, have rarely been described in gastrointestinal disease. Historically, Mycobacterium avium and Mycobacterium paratuberculosis have been found in tissue samples in patients with terminal ileitis, and have previously been described in patients with Crohn’s disease. Our study describes a rare case of mycobacterial infection with intestinal involvement.
Case Description/Methods: A 44-year-old female with a history of ankylosing spondylitis treated with adalimumab and travel to Mexico 2 years ago endorsed 5 weeks of worsening epigastric pain, unintentional weight loss, diarrhea, and arthralgias during an outpatient visit. Review of computed tomography scans 3 and 10 years prior described prominent retroperitoneal lymph nodes. She was referred to interventional radiology for lymph node biopsy which revealed necrotizing granulomatous lymphadenitis. She was admitted to the hospital and computed tomography was notable for mural thickening and inflammatory stranding of the distal small bowel, particularly the terminal ileum. Esophagogastroduodenoscopy appeared normal. Colonoscopy displayed an edematous ileocecal valve and terminal ileum with ulcers as well as erosions of the cecum and proximal ascending colon. Biopsy of the ileum demonstrated necrotizing granulomatous inflammation and biopsy of the colon was consistent with focal poorly formed granulomatous inflammation. Mycobacterium PCR and staining of the duodenal biopsy was positive for acid-fast bacilli (see figure). The Mycobacterium polymerase chain reaction testing on the same duodenal sample was negative. Serum interferon-gamma release assay was positive. She was started on rifampin, isoniazid, pyrazinamide, and ethambutol to be taken for 2 months with plan to take an additional 7 months of rifampin and isoniazid. She experienced improvement in abdominal pain after initiation of antibiotic therapy.
Discussion: Granulomatous ileitis or other intestinal manifestations of Mycobacterium species are rare, and have been previously described in the Crohn’s disease population. This case of Mycobacterium infection represents an unusual etiology for intestinal inflammation and erosions in a patient with an autoimmune condition but without known Crohn’s disease. This case highlights the importance of including mycobacterial diseases within the differential for gastrointestinal tract lesions.
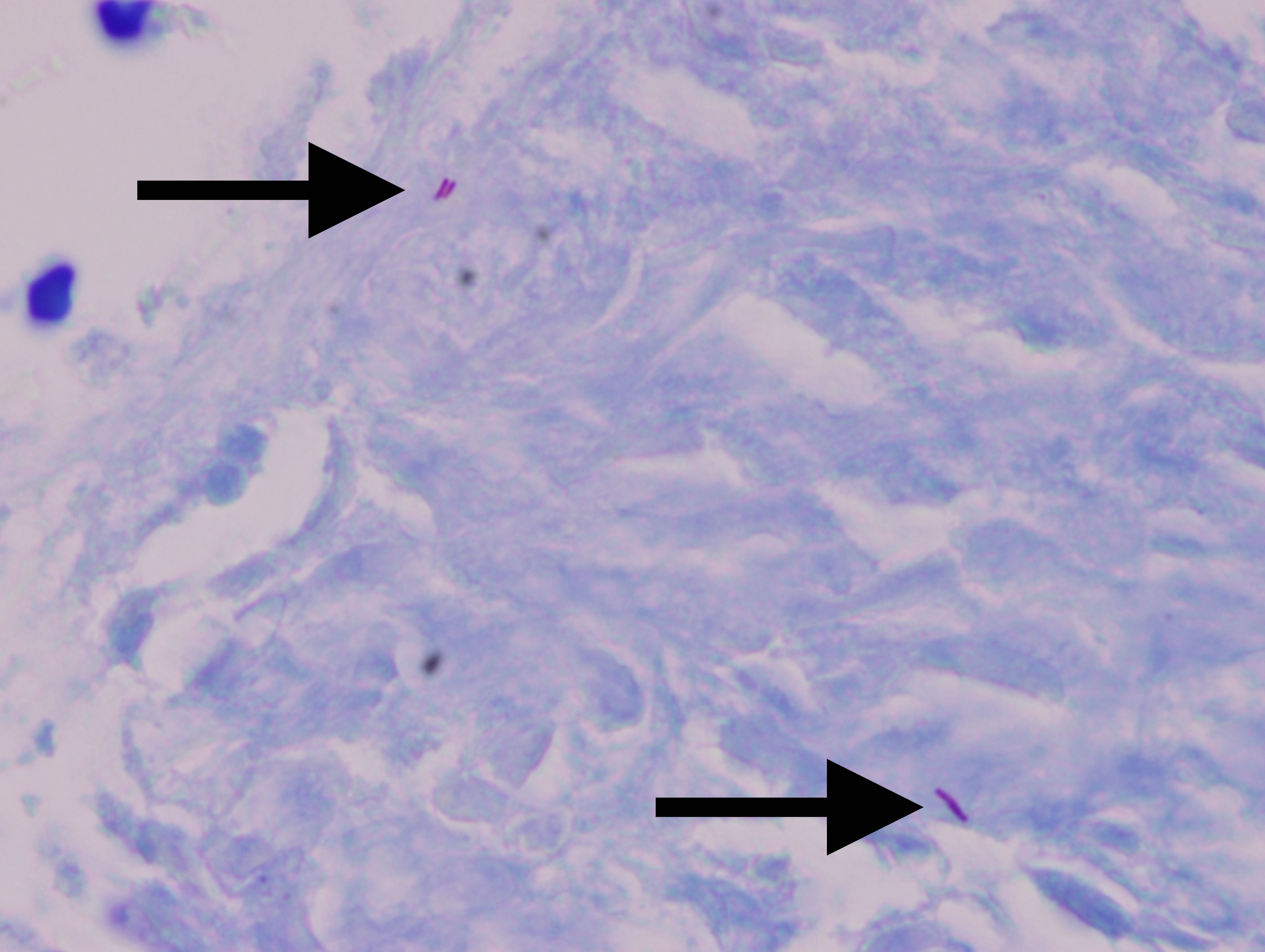
Figure: Acid-fast bacilli on duodenal biopsy
Disclosures:
Alexis Bejcek indicated no relevant financial relationships.
Adam Patrick indicated no relevant financial relationships.
Namisha Thapa indicated no relevant financial relationships.
Nada Mohamed indicated no relevant financial relationships.
Christopher Naumann indicated no relevant financial relationships.
Alexis Bejcek, MD1, Adam Patrick, BS2, Namisha Thapa, DO1, Nada Mohamed, MD1, Christopher Naumann, MD1. C0676 - A Case of Mycobacterial Infection Causing Necrotizing Granulomas of the Gastrointestinal Tract and Retroperitoneal Lymphadenopathy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
