Back

Poster Session C - Monday Afternoon
Category: Biliary/Pancreas
C0053 - Isolated Intramural Gastric Metastasis of Pancreatic Ductal Adenocarcinoma (PDAC) Detected on Surveillance Esophagogastroduodenoscopy (EGD) Before Endoscopic Ultrasound (EUS) Guided Biopsy
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Arjun Chatterjee, MD
Cleveland Clinic Foundation
Cleveland, OH
Presenting Author(s)
Award: Presidential Poster Award
Arjun Chatterjee, MD1, Andrew Ford, MD1, Amandeep Singh, MD1, Prabhleen Chahal, MD2
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic, Cleveland, OH
Introduction: PDAC is an aggressive malignancy that requires prompt diagnosis and treatment to provide the patient with the best chance of long-term survival. Patients who have an imaging-confirmed solitary pancreatic mass generally undergo a EUS-guided biopsy for histological confirmation of the diagnosis. We describe a rare case of solitary intramural gastric metastases discovered on surveillance EGD prior to EUS-guided biopsy.
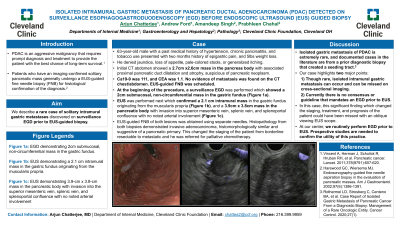
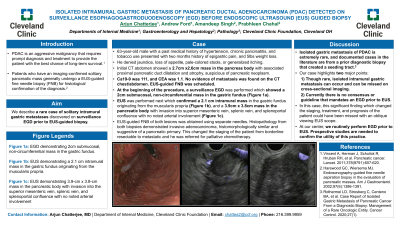
Case Description/Methods: 63-year-old male with a past medical history of hypertension, chronic pancreatitis, and tobacco use presented with two months history of epigastric pain, and 5lbs weight loss. He denied jaundice, loss of appetite, pale-colored stools, or generalized itching. Initial CT abdomen showed a 2.7cm x2.6cm mass in the pancreas body with associated proximal pancreatic duct dilatation and atrophy, suspicious of pancreatic neoplasm. Ca19-9 was 111, and CEA was 1.1. No evidence of metastasis was found on the CT chest/abdomen. EUS-guided biopsy of the mass was scheduled. At the beginning of the procedure, a surveillance EGD was performed which showed a 2cm submucosal, non-circumferential mass in the gastric fundus (Figure 1a). EUS was performed next which confirmed a 2.1 cm intramural mass in the gastric fundus originating from the muscularis propria (Figure 1b), and a 3.9cm x 3.8cm mass in the pancreatic body with invasion into superior mesenteric vein, splenic vein, and splenoportal confluence with no noted arterial involvement (Figure 1c). EUS-guided fine needle biopsy of both lesions was obtained using separate needles. Histopathology from both biopsies demonstrated invasive adenocarcinoma, histomorphologically similar and suggestive of a pancreatic primary. This changed the staging of the patient from borderline resectable to metastatic and he was referred for palliative chemotherapy.
Discussion: Isolated gastric metastasis of PDAC is extremely rare, and documented cases in the literature are from a prior diagnostic biopsy that created a seeding tract. Our case highlights two major points: 1) Though rare, isolated intramural gastric metastasis can occur and can be missed on cross-sectional imaging. 2) Currently there is no consensus or guideline that mandates an EGD prior to EUS. In this case, this significant finding which changed the staging, treatment, and prognosis of the patient could have been missed with an oblique viewing EUS scope. At our center, we routinely perform EGD prior to EUS. Prospective studies are needed to confirm the utility of this practice.

Disclosures:
Arjun Chatterjee, MD1, Andrew Ford, MD1, Amandeep Singh, MD1, Prabhleen Chahal, MD2. C0053 - Isolated Intramural Gastric Metastasis of Pancreatic Ductal Adenocarcinoma (PDAC) Detected on Surveillance Esophagogastroduodenoscopy (EGD) Before Endoscopic Ultrasound (EUS) Guided Biopsy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Arjun Chatterjee, MD1, Andrew Ford, MD1, Amandeep Singh, MD1, Prabhleen Chahal, MD2
1Cleveland Clinic Foundation, Cleveland, OH; 2Cleveland Clinic, Cleveland, OH
Introduction: PDAC is an aggressive malignancy that requires prompt diagnosis and treatment to provide the patient with the best chance of long-term survival. Patients who have an imaging-confirmed solitary pancreatic mass generally undergo a EUS-guided biopsy for histological confirmation of the diagnosis. We describe a rare case of solitary intramural gastric metastases discovered on surveillance EGD prior to EUS-guided biopsy.
Case Description/Methods: 63-year-old male with a past medical history of hypertension, chronic pancreatitis, and tobacco use presented with two months history of epigastric pain, and 5lbs weight loss. He denied jaundice, loss of appetite, pale-colored stools, or generalized itching. Initial CT abdomen showed a 2.7cm x2.6cm mass in the pancreas body with associated proximal pancreatic duct dilatation and atrophy, suspicious of pancreatic neoplasm. Ca19-9 was 111, and CEA was 1.1. No evidence of metastasis was found on the CT chest/abdomen. EUS-guided biopsy of the mass was scheduled. At the beginning of the procedure, a surveillance EGD was performed which showed a 2cm submucosal, non-circumferential mass in the gastric fundus (Figure 1a). EUS was performed next which confirmed a 2.1 cm intramural mass in the gastric fundus originating from the muscularis propria (Figure 1b), and a 3.9cm x 3.8cm mass in the pancreatic body with invasion into superior mesenteric vein, splenic vein, and splenoportal confluence with no noted arterial involvement (Figure 1c). EUS-guided fine needle biopsy of both lesions was obtained using separate needles. Histopathology from both biopsies demonstrated invasive adenocarcinoma, histomorphologically similar and suggestive of a pancreatic primary. This changed the staging of the patient from borderline resectable to metastatic and he was referred for palliative chemotherapy.
Discussion: Isolated gastric metastasis of PDAC is extremely rare, and documented cases in the literature are from a prior diagnostic biopsy that created a seeding tract. Our case highlights two major points: 1) Though rare, isolated intramural gastric metastasis can occur and can be missed on cross-sectional imaging. 2) Currently there is no consensus or guideline that mandates an EGD prior to EUS. In this case, this significant finding which changed the staging, treatment, and prognosis of the patient could have been missed with an oblique viewing EUS scope. At our center, we routinely perform EGD prior to EUS. Prospective studies are needed to confirm the utility of this practice.

Figure: Figure 1 a: EGD demonstrating 2cm submucosal, non-circumferential mass in the gastric fundus.
Figure 1 b: EUS demonstrating a 2.1 cm intramural mass in the gastric fundus originating from the muscularis propria.
Figure 1 c: EUS demonstrating 3.9-cm x 3.8-cm mass in the pancreatic body with invasion into the superior mesenteric vein, splenic vein, and splenoportal confluence with no noted arterial involvement
Figure 1 b: EUS demonstrating a 2.1 cm intramural mass in the gastric fundus originating from the muscularis propria.
Figure 1 c: EUS demonstrating 3.9-cm x 3.8-cm mass in the pancreatic body with invasion into the superior mesenteric vein, splenic vein, and splenoportal confluence with no noted arterial involvement
Disclosures:
Arjun Chatterjee indicated no relevant financial relationships.
Andrew Ford indicated no relevant financial relationships.
Amandeep Singh indicated no relevant financial relationships.
Prabhleen Chahal: Boston Scientific – Consultant. Medtronic – Consultant.
Arjun Chatterjee, MD1, Andrew Ford, MD1, Amandeep Singh, MD1, Prabhleen Chahal, MD2. C0053 - Isolated Intramural Gastric Metastasis of Pancreatic Ductal Adenocarcinoma (PDAC) Detected on Surveillance Esophagogastroduodenoscopy (EGD) Before Endoscopic Ultrasound (EUS) Guided Biopsy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

