Back

Poster Session B - Monday Morning
Category: Interventional Endoscopy
B0465 - Closing the Gap: First Report of Endoscopic Suture Closure of Malignant Gastric Hemorrhage
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Bryant Megna, MD
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Award: Presidential Poster Award
Bryant Megna, MD1, Michael Andreone, MD1, Nicholas McDonald, MD1, Dharma Sunjaya, MD2, Mohammad Bilal, MD3
1University of Minnesota, Minneapolis, MN; 2Minneapolis Veterans Affairs Health Care System, Minneapolis, MN; 3University of Minnesota and Minneapolis Veterans Affairs Health Care System, Minneapolis, MN
Introduction: Gastrointestinal bleeding secondary to luminal malignancy is typically difficult to manage with conventional endoscopic therapies. Endoscopic suturing devices have become increasing popular for the management of various resection defects, inadvertent perforations, and bariatric endosurgery. Limited recent data suggests that this technology is effective for refractory bleeding from benign peptic ulcer disease. Herein we describe a case of the successful endoscopic closure of a bleeding malignant gastric ulcer using endoscopic suturing.
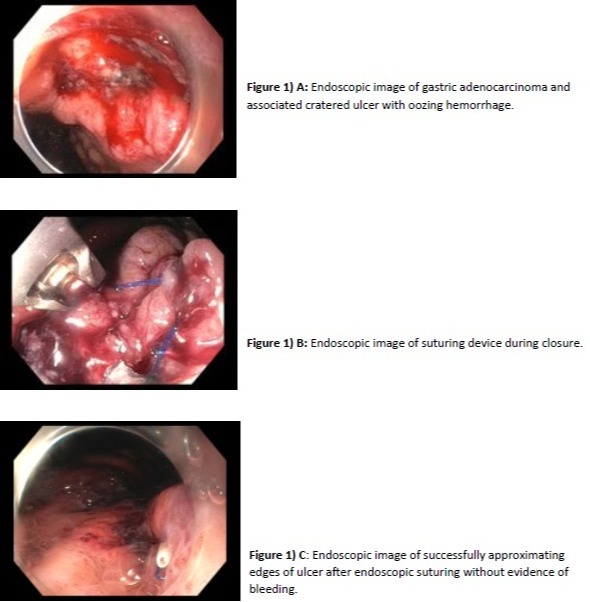
Case Description/Methods: A 60-year-old male with a past history of primary thrombocytopenia, and recent diagnosis of signet ring gastric adenocarcinoma/linitis plastica (T2, N2, M0) on FLOT chemotherapy (5-fluorouracil, leucovorin, oxaliplatin, and docetaxel) presented with hematemesis and acute on chronic anemia. Physician examination was notable for tachycardia and hypotension. Laboratory evaluation was notable for a hemoglobin of 7.8 g/dL from 15.0 g/dL four days prior. The patient was intubated and urgent upper endoscopy in the intensive care unit was performed which showed active oozing and bleeding from a cratered gastric ulcer (previously biopsy proven adenocarcinoma) on the proximal lesser curvature measuring approximately 20 mm in size (A). Diffuse thickening of gastric folds consistent with linitis plastica was also seen. Initial attempts with bipolar cautery and epinephrine injection were unable to achieve hemostasis. An endoscopic suturing system was employed to place a suture in a figure of eight fashion and cinched at end with closure of the ulcer bed (B). The ulcer bed was not visible after suturing and hemostasis was achieved (C). Repeat upper endoscopy after two weeks for nasojejunal feeding tube placement did not show presence of ulcer and any recurrent bleeding. Patient is being clinically optimized to resume chemotherapy.
Discussion: To our knowledge, we describe herein the first case of successful use of endoscopic suturing for closure of a bleeding malignant gastric ulcer. We hypothesize that the thickened gastric folds secondary to the histologic nature of linitis plastica allowed for adequate tissue purchase at the margins of the bleeding gastric ulcer which would typically be precluded in malignant tissue due to its friable nature.
Disclosures:
Bryant Megna, MD1, Michael Andreone, MD1, Nicholas McDonald, MD1, Dharma Sunjaya, MD2, Mohammad Bilal, MD3. B0465 - Closing the Gap: First Report of Endoscopic Suture Closure of Malignant Gastric Hemorrhage, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Bryant Megna, MD1, Michael Andreone, MD1, Nicholas McDonald, MD1, Dharma Sunjaya, MD2, Mohammad Bilal, MD3
1University of Minnesota, Minneapolis, MN; 2Minneapolis Veterans Affairs Health Care System, Minneapolis, MN; 3University of Minnesota and Minneapolis Veterans Affairs Health Care System, Minneapolis, MN
Introduction: Gastrointestinal bleeding secondary to luminal malignancy is typically difficult to manage with conventional endoscopic therapies. Endoscopic suturing devices have become increasing popular for the management of various resection defects, inadvertent perforations, and bariatric endosurgery. Limited recent data suggests that this technology is effective for refractory bleeding from benign peptic ulcer disease. Herein we describe a case of the successful endoscopic closure of a bleeding malignant gastric ulcer using endoscopic suturing.
Case Description/Methods: A 60-year-old male with a past history of primary thrombocytopenia, and recent diagnosis of signet ring gastric adenocarcinoma/linitis plastica (T2, N2, M0) on FLOT chemotherapy (5-fluorouracil, leucovorin, oxaliplatin, and docetaxel) presented with hematemesis and acute on chronic anemia. Physician examination was notable for tachycardia and hypotension. Laboratory evaluation was notable for a hemoglobin of 7.8 g/dL from 15.0 g/dL four days prior. The patient was intubated and urgent upper endoscopy in the intensive care unit was performed which showed active oozing and bleeding from a cratered gastric ulcer (previously biopsy proven adenocarcinoma) on the proximal lesser curvature measuring approximately 20 mm in size (A). Diffuse thickening of gastric folds consistent with linitis plastica was also seen. Initial attempts with bipolar cautery and epinephrine injection were unable to achieve hemostasis. An endoscopic suturing system was employed to place a suture in a figure of eight fashion and cinched at end with closure of the ulcer bed (B). The ulcer bed was not visible after suturing and hemostasis was achieved (C). Repeat upper endoscopy after two weeks for nasojejunal feeding tube placement did not show presence of ulcer and any recurrent bleeding. Patient is being clinically optimized to resume chemotherapy.
Discussion: To our knowledge, we describe herein the first case of successful use of endoscopic suturing for closure of a bleeding malignant gastric ulcer. We hypothesize that the thickened gastric folds secondary to the histologic nature of linitis plastica allowed for adequate tissue purchase at the margins of the bleeding gastric ulcer which would typically be precluded in malignant tissue due to its friable nature.
Figure: 1) A: Endoscopic image of gastric adenocarcinoma and associated cratered ulcer with oozing hemorrhage.
2) B: Endoscopic image of suture device during closure.
3) C: Endoscopic image of successful approximating edges of ulcer after endoscopic suturing without evidence of bleeding.
2) B: Endoscopic image of suture device during closure.
3) C: Endoscopic image of successful approximating edges of ulcer after endoscopic suturing without evidence of bleeding.
Disclosures:
Bryant Megna indicated no relevant financial relationships.
Michael Andreone indicated no relevant financial relationships.
Nicholas McDonald indicated no relevant financial relationships.
Dharma Sunjaya indicated no relevant financial relationships.
Mohammad Bilal indicated no relevant financial relationships.
Bryant Megna, MD1, Michael Andreone, MD1, Nicholas McDonald, MD1, Dharma Sunjaya, MD2, Mohammad Bilal, MD3. B0465 - Closing the Gap: First Report of Endoscopic Suture Closure of Malignant Gastric Hemorrhage, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

