Back

Poster Session C - Monday Afternoon
Category: Stomach
C0721 - Neuroendocrine Tumor Diagnosed While Performing Upper Endoscopy Surveillance of Gastric Intestinal Metaplasia
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio

Aditya Chauhan, MD
The Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
Aditya Chauhan, MD, Vijay Gayam, MD, Praneeth Bandaru, MD, Srilaxmi Gujjula, MD, Jamil Shah, MD, Derrick Cheung, MD, Denzil Etienne, MD, Madhavi Reddy, MD
The Brooklyn Hospital Center, Brooklyn, NY
Introduction: Gastric neuroendocrine tumors (GNET) are rare tumors arising from the enterochromaffin cells of the gastric mucosa, which comprise less than one percent of all gastric neoplasms and around eight percent of all gastrointestinal neuroendocrine tumors. Endoscopic resection is considered the best treatment option for type 1 GNETs. However, due to the rarity of this entity, no specific management guidelines are currently available.
Case Description/Methods:
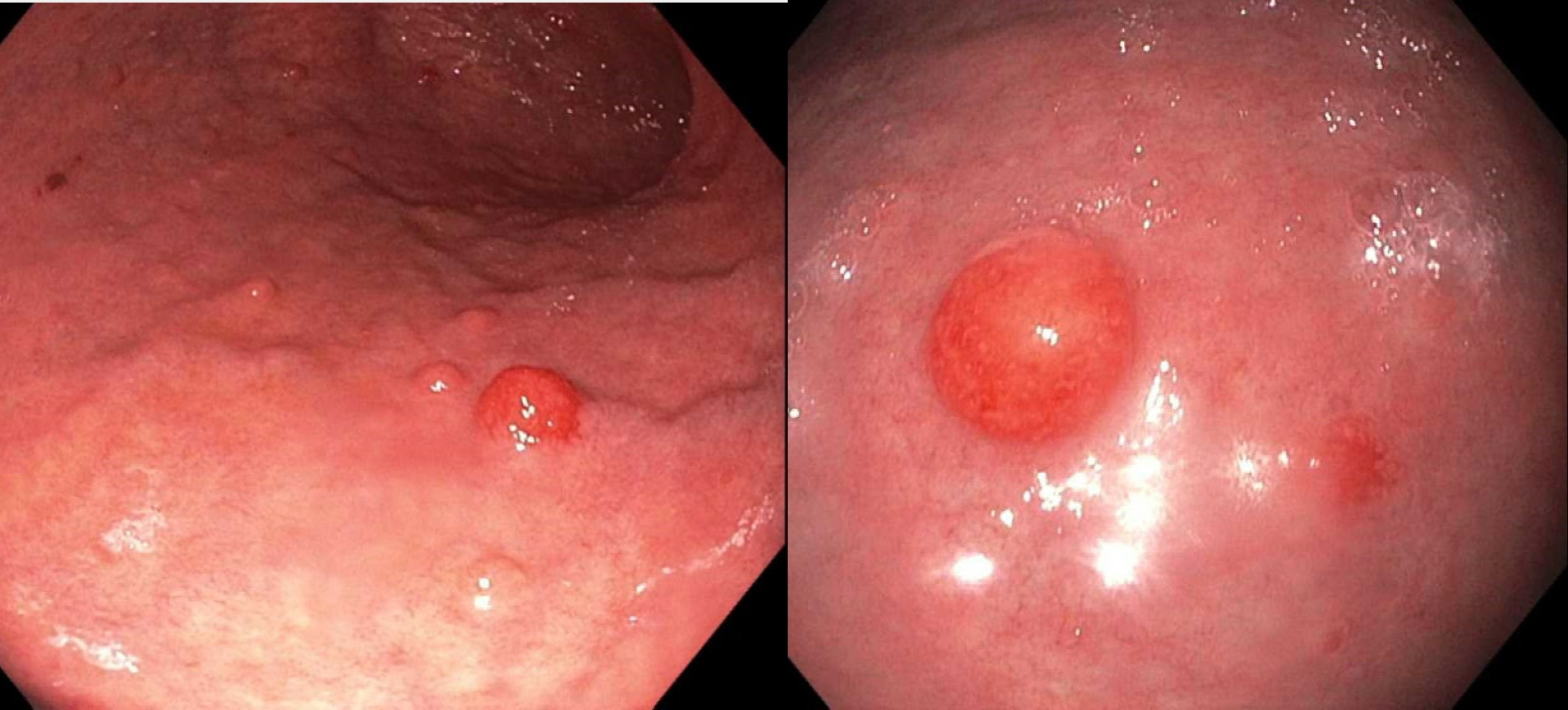
We present a case of an asymptomatic 47-year-old female diagnosed with a neuroendocrine tumor via upper endoscopy performed for surveillance of gastric intestinal metaplasia. She was found to have several gastric polyps (Figure 1), of which two had immunohistochemistry (IHC) and histology suggestive of well-differentiated neuroendocrine tumor (grade one). Notably, these polyps were found amidst the backdrop of chronic gastritis and elevated chromogranin (638.9) and gastrin (1088) levels. Biopsy results from one gastric polyp showed ink margin positive for tumor and the patient is currently scheduled to undergo endoscopic ultrasound (EUS) with polypectomy to ensure complete removal of tumors with clean margins.
Discussion: GNETs are classified into three distinct subtypes based on serum gastrin levels. Literature suggests that type 1 and type 2 GNETs are usually discovered incidentally on endoscopy. They appear as either multiple small polypoid lesions or as multiple smooth hemispherical submucosal lesions. Notably, type 1 GNETs are found commonly in the setting of atrophic gastric mucosa while type 2 GNETS are found in hypertrophic gastric mucosa.
Of note, there has been growing literature on the increasing incidence of GNET type 1 in patients with gastric metaplasia in the setting of chronic atrophic gastritis. Our case supports the literature and emphasizes the importance of being able to identify the gross morphology of GNET while carrying a high index of suspicion for this rare yet clinically relevant entity. Furthermore, the origin of neuroendocrine tumor from gastric metaplasia is intriguing and invites further studies for understanding the pathophysiology.
Disclosures:
Aditya Chauhan, MD, Vijay Gayam, MD, Praneeth Bandaru, MD, Srilaxmi Gujjula, MD, Jamil Shah, MD, Derrick Cheung, MD, Denzil Etienne, MD, Madhavi Reddy, MD. C0721 - Neuroendocrine Tumor Diagnosed While Performing Upper Endoscopy Surveillance of Gastric Intestinal Metaplasia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
The Brooklyn Hospital Center, Brooklyn, NY
Introduction: Gastric neuroendocrine tumors (GNET) are rare tumors arising from the enterochromaffin cells of the gastric mucosa, which comprise less than one percent of all gastric neoplasms and around eight percent of all gastrointestinal neuroendocrine tumors. Endoscopic resection is considered the best treatment option for type 1 GNETs. However, due to the rarity of this entity, no specific management guidelines are currently available.
Case Description/Methods:
We present a case of an asymptomatic 47-year-old female diagnosed with a neuroendocrine tumor via upper endoscopy performed for surveillance of gastric intestinal metaplasia. She was found to have several gastric polyps (Figure 1), of which two had immunohistochemistry (IHC) and histology suggestive of well-differentiated neuroendocrine tumor (grade one). Notably, these polyps were found amidst the backdrop of chronic gastritis and elevated chromogranin (638.9) and gastrin (1088) levels. Biopsy results from one gastric polyp showed ink margin positive for tumor and the patient is currently scheduled to undergo endoscopic ultrasound (EUS) with polypectomy to ensure complete removal of tumors with clean margins.
Discussion: GNETs are classified into three distinct subtypes based on serum gastrin levels. Literature suggests that type 1 and type 2 GNETs are usually discovered incidentally on endoscopy. They appear as either multiple small polypoid lesions or as multiple smooth hemispherical submucosal lesions. Notably, type 1 GNETs are found commonly in the setting of atrophic gastric mucosa while type 2 GNETS are found in hypertrophic gastric mucosa.
Of note, there has been growing literature on the increasing incidence of GNET type 1 in patients with gastric metaplasia in the setting of chronic atrophic gastritis. Our case supports the literature and emphasizes the importance of being able to identify the gross morphology of GNET while carrying a high index of suspicion for this rare yet clinically relevant entity. Furthermore, the origin of neuroendocrine tumor from gastric metaplasia is intriguing and invites further studies for understanding the pathophysiology.
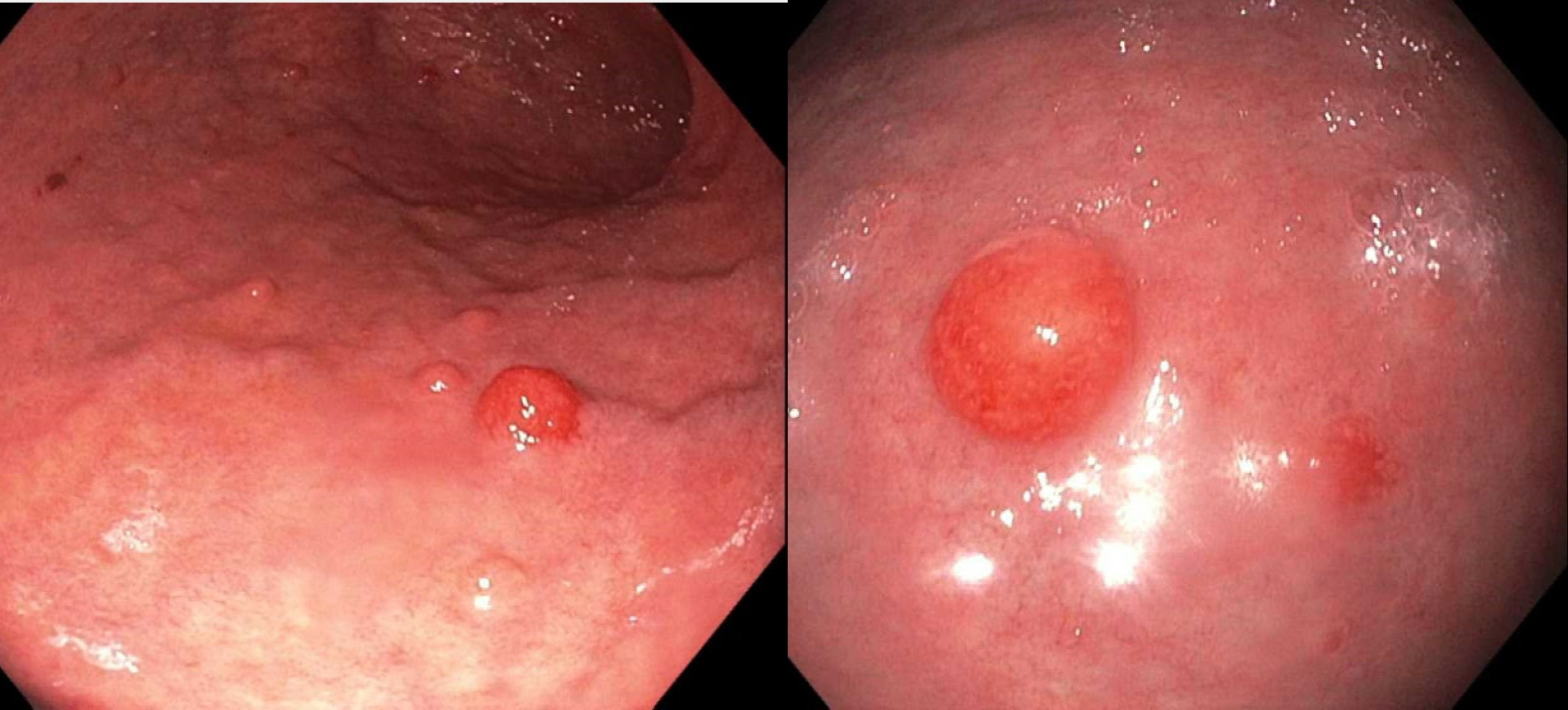
Figure: Figure 1: Multiple inflammatory gastric polyps (blue arrows) visualized on upper endoscopy
Disclosures:
Aditya Chauhan indicated no relevant financial relationships.
Vijay Gayam indicated no relevant financial relationships.
Praneeth Bandaru indicated no relevant financial relationships.
Srilaxmi Gujjula indicated no relevant financial relationships.
Jamil Shah indicated no relevant financial relationships.
Derrick Cheung indicated no relevant financial relationships.
Denzil Etienne indicated no relevant financial relationships.
Madhavi Reddy indicated no relevant financial relationships.
Aditya Chauhan, MD, Vijay Gayam, MD, Praneeth Bandaru, MD, Srilaxmi Gujjula, MD, Jamil Shah, MD, Derrick Cheung, MD, Denzil Etienne, MD, Madhavi Reddy, MD. C0721 - Neuroendocrine Tumor Diagnosed While Performing Upper Endoscopy Surveillance of Gastric Intestinal Metaplasia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
