Back

Poster Session B - Monday Morning
Category: Esophagus
B0221 - Mind the Steroids: Herpes Esophagitis in an Immunocompetent Patient After Steroid Therapy
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Saeed Graham, MD
East Carolina University Brody School of Medicine
Greenville, NC
Presenting Author(s)
Saeed Graham, MD1, Shiva Poola, MD2
1East Carolina University Brody School of Medicine, Greenville, NC; 2ECU Health Medical Center/Brody School of Medicine, Greenville, NC
Introduction: Infective esophagitis (IE) is rare, but well known to complicate the immunosuppressed state; particularly the HIV infected, transplant recipient, cancer patient and those treated with chronic corticosteroids or immunomodulators. Common infections include candida, cytomegalovirus, and herpes simplex virus (HSV). Steroids have been used for symptomatic relief of an acute sore throat. Short courses are considered benign with low risk of infectious complications. We report an immunocompetent patient found to have herpes esophagitis after a short course of corticosteroids.
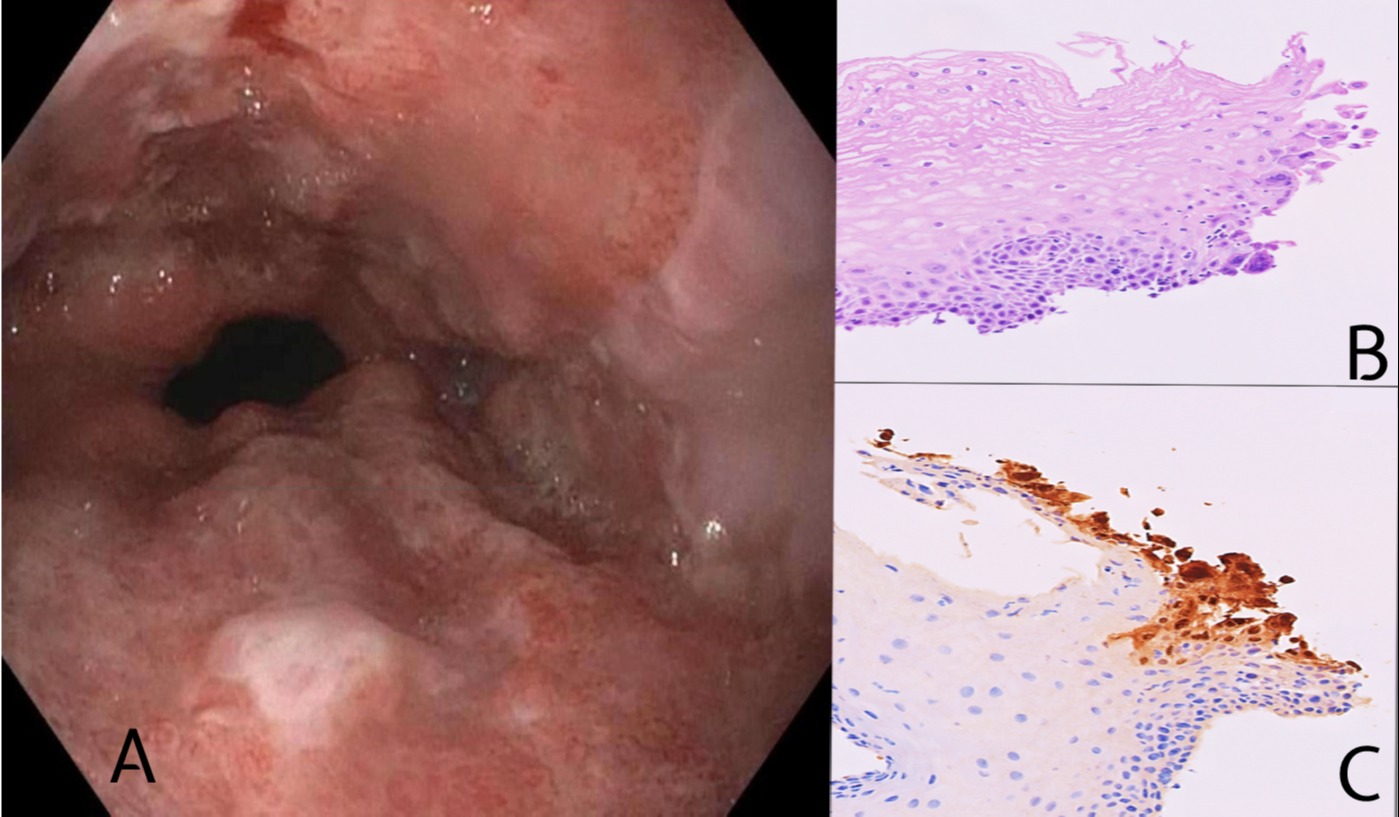
Case Description/Methods: A 41-year-old African American male with history of hypertension presented with worsening sore throat and odynophagia restricting oral intake. Prior to presentation, he had a 10-day history of sore throat. He was diagnosed with streptococcal pharyngitis and was on antibiotics and steroids 7 days ago. Given persistent symptoms he underwent laryngoscopy which demonstrated bilateral tonsillar exudates and normal pharyngeal mucosa, prompting admission and initiation of IV antibiotics and dexamethasone. He had modest improvement of pain, however 8 days later expressed worsening burning retrosternal chest pain and progressed oral intolerance. He underwent upper endoscopy revealing multiple circumferential erosions and Los Angeles grade D esophagitis of the lower third of the esophagus (Fig 1-A). Biopsies demonstrated viral intranuclear inclusions that stained positive for HSV1/HSV2 (Fig 1-B,C). His symptoms abated while on IV acyclovir allowing transition to oral valacyclovir.
Discussion: Corticosteroids are well known for their anti-inflammatory effect but immunosuppression with short courses may be underestimated. Infectious sequalae such as herpetic esophagitis may complicate steroid use even when therapy duration is short. This patient was found to have progressive odynophagia while on corticosteroids administered for analgesia and had significant improvement after antiviral therapy. It is easy to overlook IE as a cause of odynophagia in the immunocompetent, however, with history of steroid use, a diagnosis of IE, especially HSV esophagitis, should be considered in the differential. Therefore, one should have a low threshold for early endoscopy when evaluating these patients.
Disclosures:
Saeed Graham, MD1, Shiva Poola, MD2. B0221 - Mind the Steroids: Herpes Esophagitis in an Immunocompetent Patient After Steroid Therapy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1East Carolina University Brody School of Medicine, Greenville, NC; 2ECU Health Medical Center/Brody School of Medicine, Greenville, NC
Introduction: Infective esophagitis (IE) is rare, but well known to complicate the immunosuppressed state; particularly the HIV infected, transplant recipient, cancer patient and those treated with chronic corticosteroids or immunomodulators. Common infections include candida, cytomegalovirus, and herpes simplex virus (HSV). Steroids have been used for symptomatic relief of an acute sore throat. Short courses are considered benign with low risk of infectious complications. We report an immunocompetent patient found to have herpes esophagitis after a short course of corticosteroids.
Case Description/Methods: A 41-year-old African American male with history of hypertension presented with worsening sore throat and odynophagia restricting oral intake. Prior to presentation, he had a 10-day history of sore throat. He was diagnosed with streptococcal pharyngitis and was on antibiotics and steroids 7 days ago. Given persistent symptoms he underwent laryngoscopy which demonstrated bilateral tonsillar exudates and normal pharyngeal mucosa, prompting admission and initiation of IV antibiotics and dexamethasone. He had modest improvement of pain, however 8 days later expressed worsening burning retrosternal chest pain and progressed oral intolerance. He underwent upper endoscopy revealing multiple circumferential erosions and Los Angeles grade D esophagitis of the lower third of the esophagus (Fig 1-A). Biopsies demonstrated viral intranuclear inclusions that stained positive for HSV1/HSV2 (Fig 1-B,C). His symptoms abated while on IV acyclovir allowing transition to oral valacyclovir.
Discussion: Corticosteroids are well known for their anti-inflammatory effect but immunosuppression with short courses may be underestimated. Infectious sequalae such as herpetic esophagitis may complicate steroid use even when therapy duration is short. This patient was found to have progressive odynophagia while on corticosteroids administered for analgesia and had significant improvement after antiviral therapy. It is easy to overlook IE as a cause of odynophagia in the immunocompetent, however, with history of steroid use, a diagnosis of IE, especially HSV esophagitis, should be considered in the differential. Therefore, one should have a low threshold for early endoscopy when evaluating these patients.
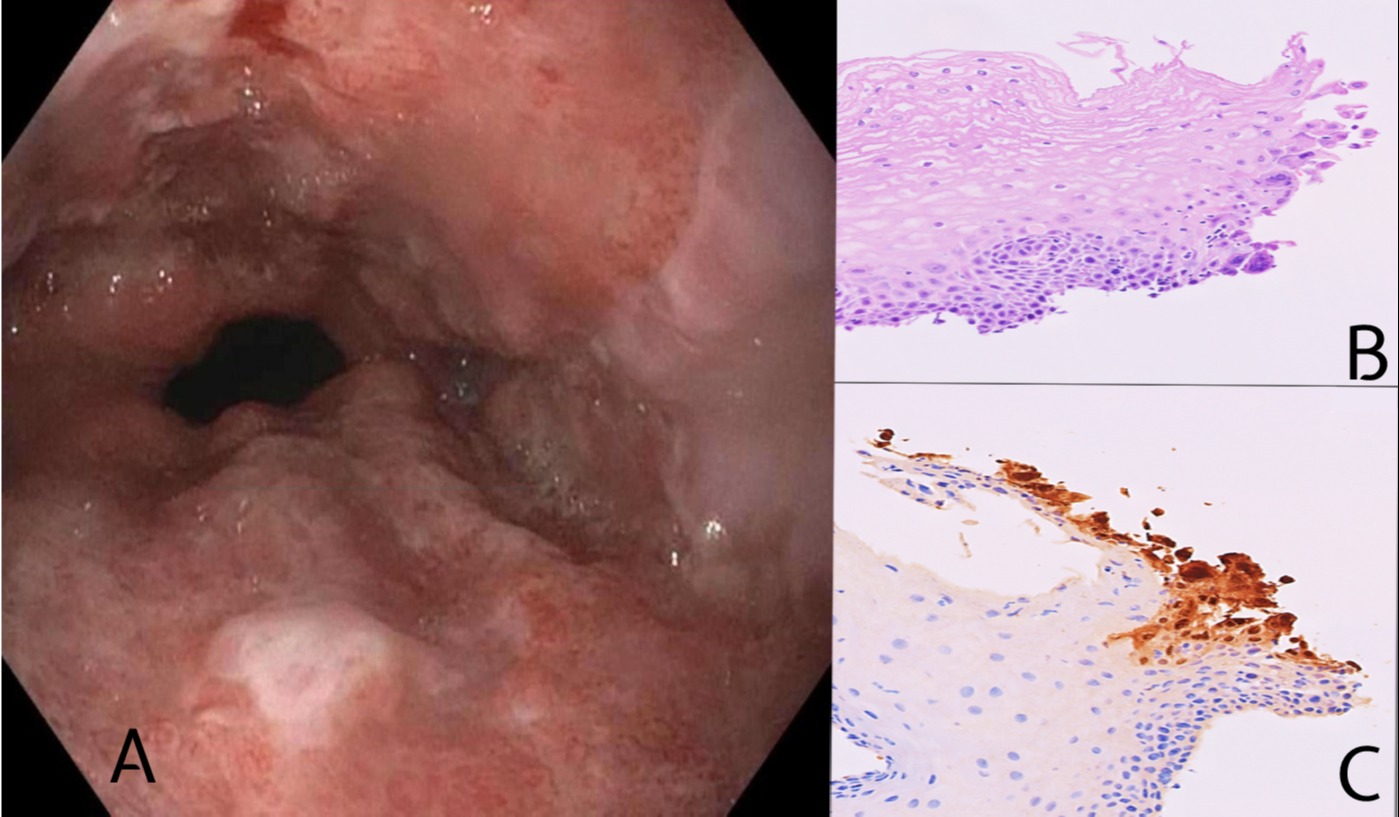
Figure: Fig 1
A: Endoscopic photograph displaying multiple circumferential erosions and Los Angeles grade D esophagitis of the lower third of the esophagus.
B: (x200): Photomicrograph of hematoxylin and eosin-stained section of the esophageal biopsy, showing multiple multinucleated epithelial cells. Cowdry type A is observed.
C: (x200): IHC study using antibodies against HSV-1. Numerous intranuclear viral inclusions are positive with HSV-1 within the infected cells.
A: Endoscopic photograph displaying multiple circumferential erosions and Los Angeles grade D esophagitis of the lower third of the esophagus.
B: (x200): Photomicrograph of hematoxylin and eosin-stained section of the esophageal biopsy, showing multiple multinucleated epithelial cells. Cowdry type A is observed.
C: (x200): IHC study using antibodies against HSV-1. Numerous intranuclear viral inclusions are positive with HSV-1 within the infected cells.
Disclosures:
Saeed Graham indicated no relevant financial relationships.
Shiva Poola indicated no relevant financial relationships.
Saeed Graham, MD1, Shiva Poola, MD2. B0221 - Mind the Steroids: Herpes Esophagitis in an Immunocompetent Patient After Steroid Therapy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
