Back

Poster Session D - Tuesday Morning
Category: Biliary/Pancreas
D0031 - An Unusual Cause of Gastric Outlet Obstruction
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Kevin Chan, MD
New York Presbyterian - Weill Cornell
New Yorrk, NY
Presenting Author(s)
Kevin Chan, MD1, Preston Atteberry, MD2, David Wan, MD2, David L. Carr-Locke, MD2, Paul Basuk, MD3
1New York Presbyterian - Weill Cornell, New Yorrk, NY; 2New York-Presbyterian Hospital/Weill Cornell Medicine, New York, NY; 3New York Presbyterian - Weill Cornell, New York, NY
Introduction: Choledochoduodenal fistula (CDF) is a rare form of biliary tract fistula characterized by an abnormal connection between the common bile duct and duodenum. It is associated with duodenal ulcers, cholelithiasis, choledocholithiasis, and even malignancy. Given its low prevalence, understanding of CDF pathology remains limited.
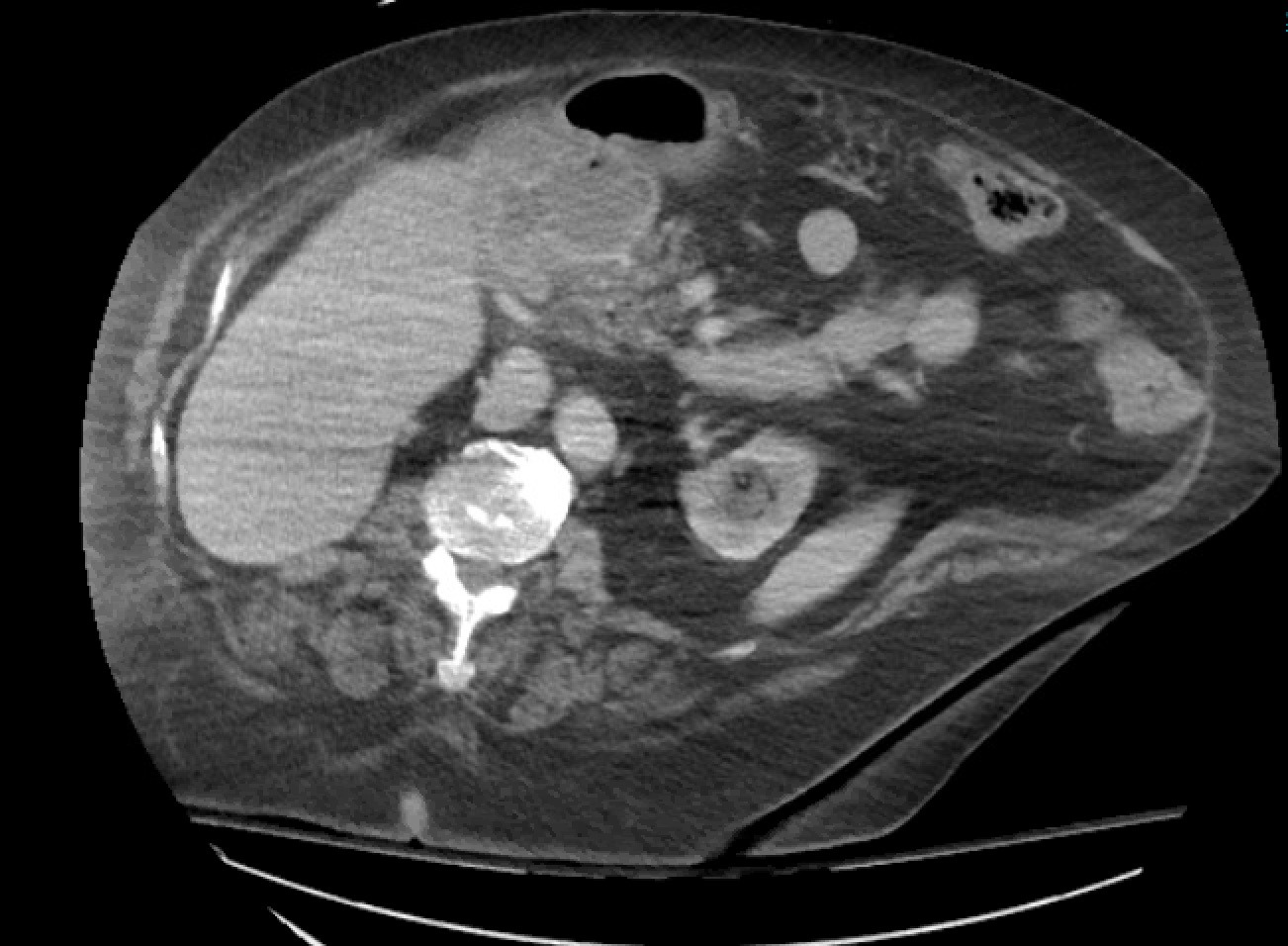
Case Description/Methods: A 75-year-old woman with hypertension, diabetes mellitus, osteoarthritis (OA), and stage IIIb right-sided colon cancer (in remission after FOLFOX and right hemicolectomy 3 years prior) presented to the hospital with one day of nausea and vomiting. She reported 20 episodes of coffee-ground emesis and taking up to 8 200mg ibuprofen daily for months to treat her OA. Labs were notable for hemoglobin of 8.7 g/dL without known baseline. She was started on intravenous pantoprazole given concern for upper gastrointestinal bleed. Esophagogastroduodenoscopy revealed 1.5 liters of retained non-bloody fluid with obstructing objects in the duodenal bulb immediately distal to the pylorus that were unable to be removed and adjacent ulcerations not amenable to endoscopic therapy. A nasogastric tube was placed for decompression. The obstructing bodies were initially thought to be bezoars, but later identified as gallstones. Abdominal CT demonstrated a CDF with adjacent abscess (Figure 1). The patient underwent exploratory laparotomy, gastrotomy, gastroduodenoscopy with morcellation and removal of gallstones, and successful decompression of the duodenum. The CDF was visualized with a free-flowing stone in the lumen. Post-operatively, the patient had resolution of nausea and vomiting and was discharged tolerating an oral diet.
Discussion: CDF is usually an incidental and asymptomatic finding. When symptomatic, they commonly present with cholangitic symptoms such as fever, abdominal pain, and jaundice. Rarely, patients can present with Bouveret Syndrome, a clinical process describing gastric outlet obstruction in the setting of gallstone ileus and CDF. Nausea, vomiting, and abdominal pain are common presenting symptoms, but hematemesis and melena have also been described. There is no standardized management, but the treatment goal involves removing the culprit obstruction either via endoscopic or surgical retrieval. Symptomatic CDF patients are at risk for recurrence, although ongoing debate exists on risk-stratifying candidates for CDF repair based on location versus size of fistula. Proper management of symptomatic CDF is important for preventing further morbidity.
Disclosures:
Kevin Chan, MD1, Preston Atteberry, MD2, David Wan, MD2, David L. Carr-Locke, MD2, Paul Basuk, MD3. D0031 - An Unusual Cause of Gastric Outlet Obstruction, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1New York Presbyterian - Weill Cornell, New Yorrk, NY; 2New York-Presbyterian Hospital/Weill Cornell Medicine, New York, NY; 3New York Presbyterian - Weill Cornell, New York, NY
Introduction: Choledochoduodenal fistula (CDF) is a rare form of biliary tract fistula characterized by an abnormal connection between the common bile duct and duodenum. It is associated with duodenal ulcers, cholelithiasis, choledocholithiasis, and even malignancy. Given its low prevalence, understanding of CDF pathology remains limited.
Case Description/Methods: A 75-year-old woman with hypertension, diabetes mellitus, osteoarthritis (OA), and stage IIIb right-sided colon cancer (in remission after FOLFOX and right hemicolectomy 3 years prior) presented to the hospital with one day of nausea and vomiting. She reported 20 episodes of coffee-ground emesis and taking up to 8 200mg ibuprofen daily for months to treat her OA. Labs were notable for hemoglobin of 8.7 g/dL without known baseline. She was started on intravenous pantoprazole given concern for upper gastrointestinal bleed. Esophagogastroduodenoscopy revealed 1.5 liters of retained non-bloody fluid with obstructing objects in the duodenal bulb immediately distal to the pylorus that were unable to be removed and adjacent ulcerations not amenable to endoscopic therapy. A nasogastric tube was placed for decompression. The obstructing bodies were initially thought to be bezoars, but later identified as gallstones. Abdominal CT demonstrated a CDF with adjacent abscess (Figure 1). The patient underwent exploratory laparotomy, gastrotomy, gastroduodenoscopy with morcellation and removal of gallstones, and successful decompression of the duodenum. The CDF was visualized with a free-flowing stone in the lumen. Post-operatively, the patient had resolution of nausea and vomiting and was discharged tolerating an oral diet.
Discussion: CDF is usually an incidental and asymptomatic finding. When symptomatic, they commonly present with cholangitic symptoms such as fever, abdominal pain, and jaundice. Rarely, patients can present with Bouveret Syndrome, a clinical process describing gastric outlet obstruction in the setting of gallstone ileus and CDF. Nausea, vomiting, and abdominal pain are common presenting symptoms, but hematemesis and melena have also been described. There is no standardized management, but the treatment goal involves removing the culprit obstruction either via endoscopic or surgical retrieval. Symptomatic CDF patients are at risk for recurrence, although ongoing debate exists on risk-stratifying candidates for CDF repair based on location versus size of fistula. Proper management of symptomatic CDF is important for preventing further morbidity.
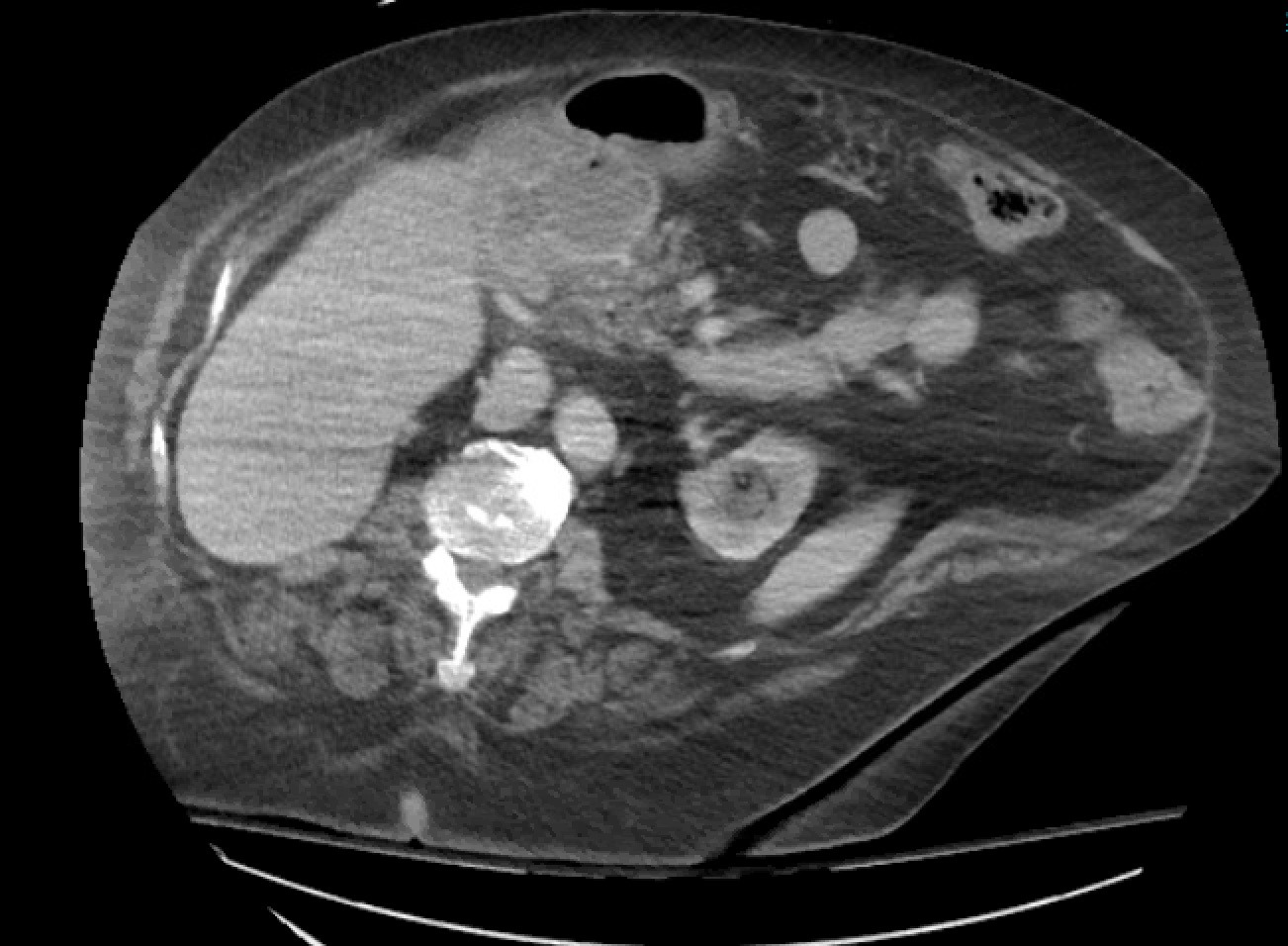
Figure: Figure 1 Abdominal CT demonstrating choledochoduodenal fistula and associated abscess
Disclosures:
Kevin Chan indicated no relevant financial relationships.
Preston Atteberry indicated no relevant financial relationships.
David Wan indicated no relevant financial relationships.
David Carr-Locke indicated no relevant financial relationships.
Paul Basuk indicated no relevant financial relationships.
Kevin Chan, MD1, Preston Atteberry, MD2, David Wan, MD2, David L. Carr-Locke, MD2, Paul Basuk, MD3. D0031 - An Unusual Cause of Gastric Outlet Obstruction, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
