Back

Poster Session D - Tuesday Morning
Category: Biliary/Pancreas
D0033 - Severe Steatorrhea in the Setting of Chronic Pancreatitis Leading to Hyperoxaluria and Subsequent Oxalate Nephropathy Necessitating Dialysis
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Colin Leffert, DO
Ascension
Royal Oak, MI
Presenting Author(s)
Colin Leffert, DO1, Rene Peleman, MD2, Natalie Peleman, PA-C2
1Ascension, Royal Oak, MI; 2Henry Ford Health System, Clinton Township, MI
Introduction: Steatorrhea is a common clinical entity encountered by gastroenterologists spanning a wide array of patient populations. In addition to causing disruptive symptoms which negative impact quality of life, steatorrhea leads to fat-soluble vitamin deficiency and the corresponding adverse affects including mineral and bone disease, clotting factor deficiency, and delayed wound healing. While multiple disorders can lead to steatorrhea, this report will focus on chronic pancreatitis. Regardless of the etiology, some patients may ultimately develop hyperoxaluria due to the interaction between non absorbed fat in the gut lumen, calcium, and oxalate. This has the potential to lead to oxalate nephropathy, and in extreme cases, acute renal failure. We herein present the case of an 89-year-old man receiving treatment for chronic pancreatitis who developed acute renal failure requiring dialysis secondary to oxalate nephropathy.
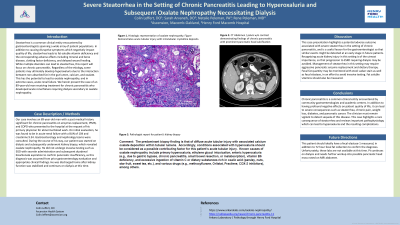
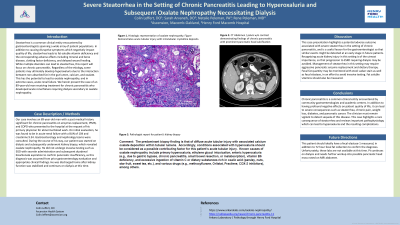
Case Description/Methods: Our case involves an 89-year-old man with a past medical history significant for chronic pancreatitis on enzymes replacement, IPMN, and COPD who presented to the hospital at the request of his primary physician for abnormal blood work. On initial evaluation, he was found to be in acute renal failure with a BUN of 104 and creatinine 9.34. Gastroenterology and nephrology teams were consulted. During the course of his stay, our patient was started on dialysis and subsequently underwent kidney biopsy, which revealed oxalate nephropathy. He did not undergo invasive testing such as EGD with secretin administration and subsequent duodenal bicarbonate aspiration to confirm pancreatic insufficiency, as this diagnosis was assumed from prior gastroenterology evaluation and appropriate clinical findings. He was discharged home after kidney function was stabilized and continues on dialysis at this time.
Discussion: This case presentation highlights a potential adverse outcome associated with severe steatorrhea in the setting of chronic pancreatitis, and is a useful lesson for the gastroenterologist so that similar events might be detected at an early stage in future patients. Recognizing acute kidney injury in this setting is of the utmost importance, so that progression to ESRD requiring dialysis may be avoided. Management of steatorrhea in this setting may require aggressive pancreatic enzyme replacement and dietary therapy. Fecal fat quantity may be monitored with stool sudan stain as well as fecal elastase, in an effort to avoid invasive testing.

Disclosures:
Colin Leffert, DO1, Rene Peleman, MD2, Natalie Peleman, PA-C2. D0033 - Severe Steatorrhea in the Setting of Chronic Pancreatitis Leading to Hyperoxaluria and Subsequent Oxalate Nephropathy Necessitating Dialysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Ascension, Royal Oak, MI; 2Henry Ford Health System, Clinton Township, MI
Introduction: Steatorrhea is a common clinical entity encountered by gastroenterologists spanning a wide array of patient populations. In addition to causing disruptive symptoms which negative impact quality of life, steatorrhea leads to fat-soluble vitamin deficiency and the corresponding adverse affects including mineral and bone disease, clotting factor deficiency, and delayed wound healing. While multiple disorders can lead to steatorrhea, this report will focus on chronic pancreatitis. Regardless of the etiology, some patients may ultimately develop hyperoxaluria due to the interaction between non absorbed fat in the gut lumen, calcium, and oxalate. This has the potential to lead to oxalate nephropathy, and in extreme cases, acute renal failure. We herein present the case of an 89-year-old man receiving treatment for chronic pancreatitis who developed acute renal failure requiring dialysis secondary to oxalate nephropathy.
Case Description/Methods: Our case involves an 89-year-old man with a past medical history significant for chronic pancreatitis on enzymes replacement, IPMN, and COPD who presented to the hospital at the request of his primary physician for abnormal blood work. On initial evaluation, he was found to be in acute renal failure with a BUN of 104 and creatinine 9.34. Gastroenterology and nephrology teams were consulted. During the course of his stay, our patient was started on dialysis and subsequently underwent kidney biopsy, which revealed oxalate nephropathy. He did not undergo invasive testing such as EGD with secretin administration and subsequent duodenal bicarbonate aspiration to confirm pancreatic insufficiency, as this diagnosis was assumed from prior gastroenterology evaluation and appropriate clinical findings. He was discharged home after kidney function was stabilized and continues on dialysis at this time.
Discussion: This case presentation highlights a potential adverse outcome associated with severe steatorrhea in the setting of chronic pancreatitis, and is a useful lesson for the gastroenterologist so that similar events might be detected at an early stage in future patients. Recognizing acute kidney injury in this setting is of the utmost importance, so that progression to ESRD requiring dialysis may be avoided. Management of steatorrhea in this setting may require aggressive pancreatic enzyme replacement and dietary therapy. Fecal fat quantity may be monitored with stool sudan stain as well as fecal elastase, in an effort to avoid invasive testing.
Disclosures:
Colin Leffert indicated no relevant financial relationships.
Rene Peleman indicated no relevant financial relationships.
Natalie Peleman indicated no relevant financial relationships.
Colin Leffert, DO1, Rene Peleman, MD2, Natalie Peleman, PA-C2. D0033 - Severe Steatorrhea in the Setting of Chronic Pancreatitis Leading to Hyperoxaluria and Subsequent Oxalate Nephropathy Necessitating Dialysis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
