Back

Poster Session D - Tuesday Morning
Category: Biliary/Pancreas
D0035 - Atypical Presentation of Pancreatic Serous Cystadenoma
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Chisom Anyanwoke, MD
University of Miami, Holy Cross Hospital
Fort Lauderdale, FL
Presenting Author(s)
Chisom Anyanwoke, MD1, Wisam Zakko, MD2
1University of Miami, Holy Cross Hospital, Fort Lauderdale, FL; 2MD, Fort Lauderdale, FL
Introduction: Pancreatic serous cystadenomas (PSCA) which represent one-third of pancreatic cystic neoplasms are typically benign asymptomatic lesions usually found incidentally on imaging studies at the body or tail of the pancreas. When symptomatic, presents typically with abdominal pain and a palpable mass. We report a case with PSCA presented as chronic diarrhea due to pancreatic duct (PD) obstruction with further enlargement over the years leading to biliary and partial duodenal obstruction.
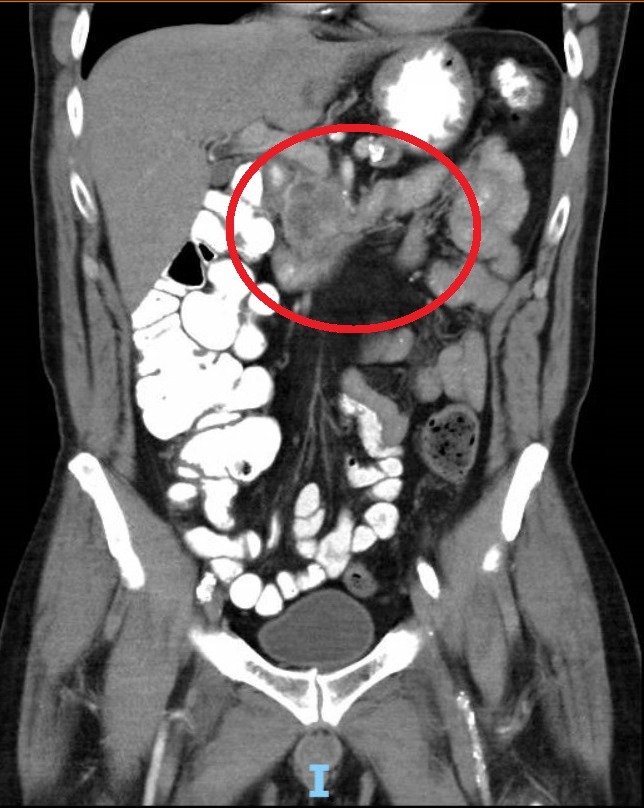
Case Description/Methods: 65 year old man with chronic diarrhea and a remote history of Hodgkin’s Lymphoma treated with Mantle and pelvic radiation. Initially diagnosed as radiation enteritis, presented to our clinic with worsening diarrhea, flatulence, bloating, and weight loss. Endoscopic evaluation was negative for celiac disease or microscopic colitis. Diarrhea responded to empiric trial of pancreatic enzymes and he regained weight. CT scan of abdomen done to determine the etiology of exocrine pancreatic insufficiency (EPI) revealed a 3.7 cm complex cystic mass in the in the head of the pancreas with PD dilation and atrophy of the body and tail. Endoscopic ultrasound showed pancreatic mass with involvement of SMA and portal vein. Fine needle aspiration was not diagnostic. CT-guided biopsy was consistent with PSCA. 4 years later he complained of pale stools and dark urine; labs revealed ALT 495, alkaline phosphatase 463, bilirubin 4.5. MRI showed cyst enlargement to 5.7 cm with biliary dilation. Surgical consultation deemed him not to be a surgical candidate because of radiation induced vascular disease. ERCP with fully covered stent placement led to resolution of symptoms and normalization of liver tests. A year later ERCP with stent exchange showed compression of the duodenum distal to the stent leading to partial obstruction.
Discussion: PSCA is usually an incidental finding on imaging studies. EPI is most commonly a result of chronic pancreatitis. Our patient presented with chronic diarrhea due to EPI as a result of PD obstruction by a PSCA. This case underscores the importance of imaging the pancreas in all patients with EPI to evaluate for potential underlying neoplasm causing obstruction of the PD. Our case also highlights that PSCA although benign if in the head of the pancreas can grow in size leading to gastric outlet obstruction and obstructive jaundice which can be associated with significant morbidity if the patient is not a surgical candidate.
Disclosures:
Chisom Anyanwoke, MD1, Wisam Zakko, MD2. D0035 - Atypical Presentation of Pancreatic Serous Cystadenoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Miami, Holy Cross Hospital, Fort Lauderdale, FL; 2MD, Fort Lauderdale, FL
Introduction: Pancreatic serous cystadenomas (PSCA) which represent one-third of pancreatic cystic neoplasms are typically benign asymptomatic lesions usually found incidentally on imaging studies at the body or tail of the pancreas. When symptomatic, presents typically with abdominal pain and a palpable mass. We report a case with PSCA presented as chronic diarrhea due to pancreatic duct (PD) obstruction with further enlargement over the years leading to biliary and partial duodenal obstruction.
Case Description/Methods: 65 year old man with chronic diarrhea and a remote history of Hodgkin’s Lymphoma treated with Mantle and pelvic radiation. Initially diagnosed as radiation enteritis, presented to our clinic with worsening diarrhea, flatulence, bloating, and weight loss. Endoscopic evaluation was negative for celiac disease or microscopic colitis. Diarrhea responded to empiric trial of pancreatic enzymes and he regained weight. CT scan of abdomen done to determine the etiology of exocrine pancreatic insufficiency (EPI) revealed a 3.7 cm complex cystic mass in the in the head of the pancreas with PD dilation and atrophy of the body and tail. Endoscopic ultrasound showed pancreatic mass with involvement of SMA and portal vein. Fine needle aspiration was not diagnostic. CT-guided biopsy was consistent with PSCA. 4 years later he complained of pale stools and dark urine; labs revealed ALT 495, alkaline phosphatase 463, bilirubin 4.5. MRI showed cyst enlargement to 5.7 cm with biliary dilation. Surgical consultation deemed him not to be a surgical candidate because of radiation induced vascular disease. ERCP with fully covered stent placement led to resolution of symptoms and normalization of liver tests. A year later ERCP with stent exchange showed compression of the duodenum distal to the stent leading to partial obstruction.
Discussion: PSCA is usually an incidental finding on imaging studies. EPI is most commonly a result of chronic pancreatitis. Our patient presented with chronic diarrhea due to EPI as a result of PD obstruction by a PSCA. This case underscores the importance of imaging the pancreas in all patients with EPI to evaluate for potential underlying neoplasm causing obstruction of the PD. Our case also highlights that PSCA although benign if in the head of the pancreas can grow in size leading to gastric outlet obstruction and obstructive jaundice which can be associated with significant morbidity if the patient is not a surgical candidate.
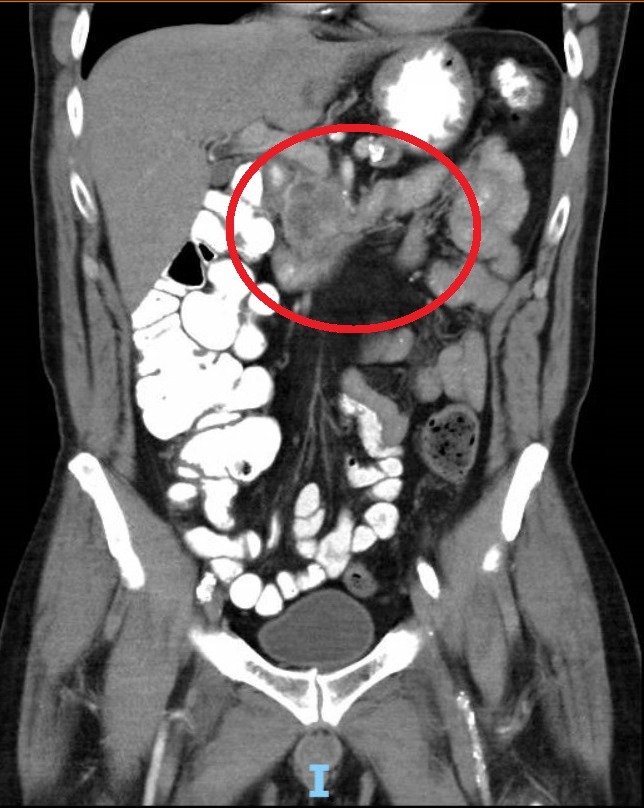
Figure: There is an approximately 4.0 cm x 3.7 cm ill-defined complex mass in the head of the pancreas.
Disclosures:
Chisom Anyanwoke indicated no relevant financial relationships.
Wisam Zakko indicated no relevant financial relationships.
Chisom Anyanwoke, MD1, Wisam Zakko, MD2. D0035 - Atypical Presentation of Pancreatic Serous Cystadenoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

