Back

Poster Session B - Monday Morning
Category: Esophagus
B0249 - Case Series: The Changing Paradigm in Management of Spontaneous Esophageal Perforation
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- KY
Kevin Yeroushalmi, MD
Nassau University Medical Center
East Meadow, NY
Presenting Author(s)
Kevin Yeroushalmi, MD, Sandra Gomez-Paz, MD, Jiten Desai, MD, Krishnaiyer Subramani, MD, Nausheer Khan, MD, Kaleem Rizvon, , Deepthi Kagolanu, MD
Nassau University Medical Center, East Meadow, NY
Introduction: Despite advances in medical knowledge, esophageal perforation remains a condition with high morbidity and mortality. Prognostic factors include: etiology and location of esophageal injury; presence of underlying esophageal disease; interval between perforation and intervention; and method of treatment. Here, we present two cases of spontaneous esophageal perforation that were managed differently but both resulted in favorable outcomes.
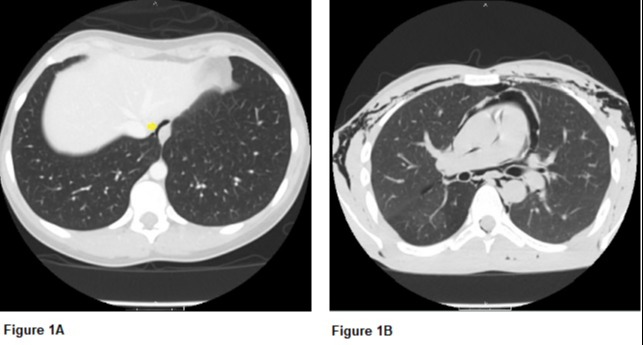
Case Description/Methods: Case 1: 26-year-old female experienced excruciating chest pain following a bout of intractable nausea and vomiting. Physical examination revealed tenderness to palpation in epigastrium and minimal amounts of crepitus in the neck. CT Thorax revealed small volume pneumomediastinum (Figure 1A). The patient was managed conservatively with intravenous (IV) fluid hydration, IV antibiotics, and nothing by mouth. Repeat imaging was performed 10 days after initial CT which revealed interval resolution of pneumomediastinum. Patient was started on clear liquids and diet was advanced thereafter.
Case 2: 20-year-old male presented to emergency department (ED) with intractable nausea and vomiting after cocaine inhalation. Patient subsequently developed substernal chest pain with shortness of breath. Physical examination was notable for subcutaneous emphysema in the neck, shoulders, and back. Emergent CT revealed extensive pneumomediastinum with extension of air into the chest, back, and neck (Figure 1B). Gastrograffin esophagram revealed extravasation of contrast at GE junction. The patient underwent primary closure of esophageal perforation. The patient was monitored closely on the inpatient service until his symptoms improved and he was discharged on hospital day 14.
Discussion: The optimal management of esophageal perforation remains debatable, particularly for small well-contained perforations. With advances in minimally invasive techniques, the need for surgical exploration appears to be diminishing. Neither patient in this case series suffered from underlying esophageal disease. Both patients had an injury to the distal esophagus that was addressed within 24 hours of presentation; however, one patient was managed conservatively whereas the other patient was managed surgically. While the outcome for both cases was favorable, the morbidity involved with surgical intervention was higher. Perhaps, a minimally invasive approach should be considered in all non-emergent cases prior to surgical intervention in an effort to further decrease morbidity.
Disclosures:
Kevin Yeroushalmi, MD, Sandra Gomez-Paz, MD, Jiten Desai, MD, Krishnaiyer Subramani, MD, Nausheer Khan, MD, Kaleem Rizvon, , Deepthi Kagolanu, MD. B0249 - Case Series: The Changing Paradigm in Management of Spontaneous Esophageal Perforation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Nassau University Medical Center, East Meadow, NY
Introduction: Despite advances in medical knowledge, esophageal perforation remains a condition with high morbidity and mortality. Prognostic factors include: etiology and location of esophageal injury; presence of underlying esophageal disease; interval between perforation and intervention; and method of treatment. Here, we present two cases of spontaneous esophageal perforation that were managed differently but both resulted in favorable outcomes.
Case Description/Methods: Case 1: 26-year-old female experienced excruciating chest pain following a bout of intractable nausea and vomiting. Physical examination revealed tenderness to palpation in epigastrium and minimal amounts of crepitus in the neck. CT Thorax revealed small volume pneumomediastinum (Figure 1A). The patient was managed conservatively with intravenous (IV) fluid hydration, IV antibiotics, and nothing by mouth. Repeat imaging was performed 10 days after initial CT which revealed interval resolution of pneumomediastinum. Patient was started on clear liquids and diet was advanced thereafter.
Case 2: 20-year-old male presented to emergency department (ED) with intractable nausea and vomiting after cocaine inhalation. Patient subsequently developed substernal chest pain with shortness of breath. Physical examination was notable for subcutaneous emphysema in the neck, shoulders, and back. Emergent CT revealed extensive pneumomediastinum with extension of air into the chest, back, and neck (Figure 1B). Gastrograffin esophagram revealed extravasation of contrast at GE junction. The patient underwent primary closure of esophageal perforation. The patient was monitored closely on the inpatient service until his symptoms improved and he was discharged on hospital day 14.
Discussion: The optimal management of esophageal perforation remains debatable, particularly for small well-contained perforations. With advances in minimally invasive techniques, the need for surgical exploration appears to be diminishing. Neither patient in this case series suffered from underlying esophageal disease. Both patients had an injury to the distal esophagus that was addressed within 24 hours of presentation; however, one patient was managed conservatively whereas the other patient was managed surgically. While the outcome for both cases was favorable, the morbidity involved with surgical intervention was higher. Perhaps, a minimally invasive approach should be considered in all non-emergent cases prior to surgical intervention in an effort to further decrease morbidity.
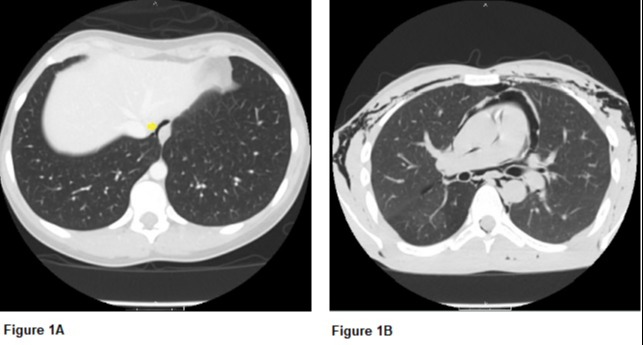
Figure: Figure 1A. CT thorax revealing free air around distal esophagus (see yellow arrow)
Figure 1B. CT thorax demonstrating extensive air throughout the mediastinum, extending into the pericardial sac and soft tissues of chest
Figure 1B. CT thorax demonstrating extensive air throughout the mediastinum, extending into the pericardial sac and soft tissues of chest
Disclosures:
Kevin Yeroushalmi indicated no relevant financial relationships.
Sandra Gomez-Paz indicated no relevant financial relationships.
Jiten Desai indicated no relevant financial relationships.
Krishnaiyer Subramani indicated no relevant financial relationships.
Nausheer Khan indicated no relevant financial relationships.
Kaleem Rizvon indicated no relevant financial relationships.
Deepthi Kagolanu indicated no relevant financial relationships.
Kevin Yeroushalmi, MD, Sandra Gomez-Paz, MD, Jiten Desai, MD, Krishnaiyer Subramani, MD, Nausheer Khan, MD, Kaleem Rizvon, , Deepthi Kagolanu, MD. B0249 - Case Series: The Changing Paradigm in Management of Spontaneous Esophageal Perforation, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
