Back

Poster Session D - Tuesday Morning
Category: Biliary/Pancreas
D0045 - All Nodules Are Not Equal: A Rare Presentation of Pancreatic Cancer
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- BW
Brian Woods, BS
Prisma Health
Greenville, South Carolina
Presenting Author(s)
Brian Woods, BS1, Anthony Scholer, MD1, Robert Farrar, MD1, Veeral Oza, MD2
1Prisma Health, Greenville, SC; 2University of South Carolina School of Medicine Greenville, Prisma Health, Greenville, SC
Introduction: Pancreatic cancer has a 5-year survival of about 11%. An atypical presentation can make early diagnosis a challenge. Standard diagnostic measures such as computed tomography (CT) and endoscopy (EGD/EUS) may not provide enough information for diagnosis of a pancreatic cancer, particularly if presence of unusual anatomy was not previously known. In this case, we present a patient with adenocarcinoma developing in an ectopic pancreas (EP) adjacent to the third part of duodenum (D3)
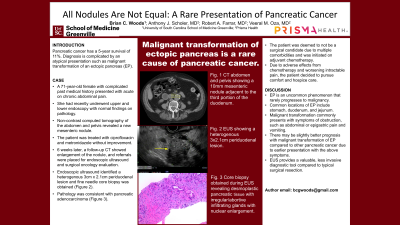
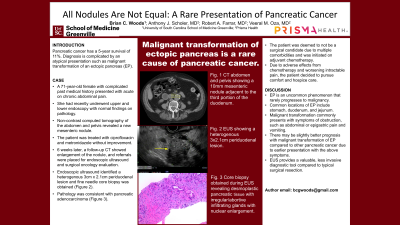
Case Description/Methods: A 71-year-old female with past medical history of an abdominal aortic aneurysm, coronary artery disease, end-stage lung disease on home oxygen, hypertension, and chronic abdominal pain presented with abdominal pain and nausea. She had a CT scan which revealed a 10mm mesenteric nodule adjacent to D3. A follow-up study six weeks later revealed enlargement of the node to 13mm x 11mm (Fig 1a), and she was referred to surgery for evaluation. Patient was then referred to the gastroenterology for an endoscopic evaluation of what was initially thought to be a lymph node. An EGD/EUS revealed normal endoscopic findings, with a heterogenous periduodenal lesion measuring 3cm x 2.1cm was identified (Fig 1b). This was separate from the remainder of the pancreas. A biopsy of this lesion was performed.
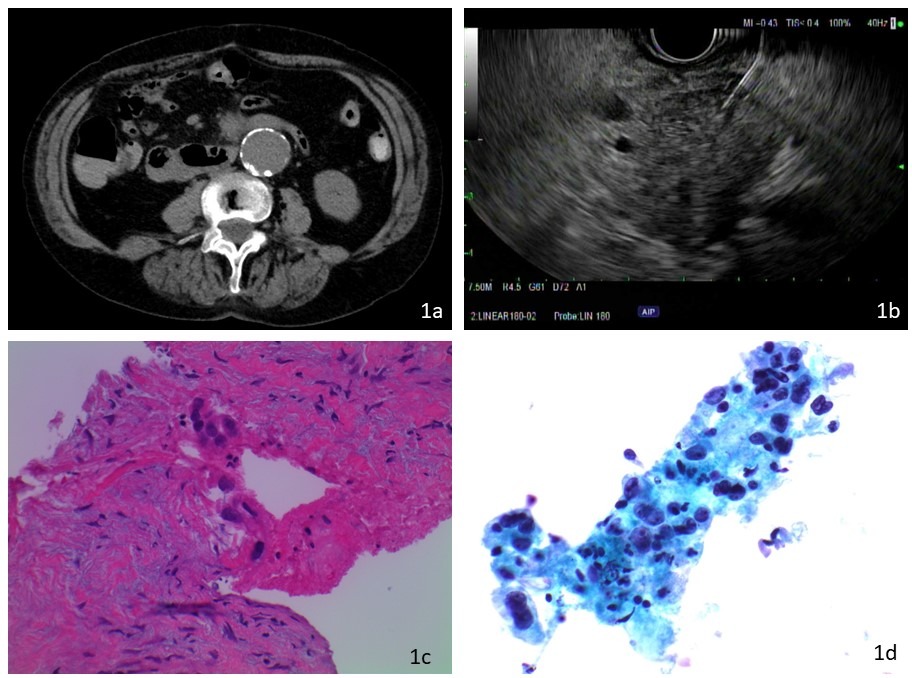
Pathology revealed groups of crowded atypical glandular cells with anisonucleosis; consistent with a diagnosis of pancreatic tissue with well-differentiated adenocarcinoma (Fig1c,d). The patient was deemed to not be a surgical candidate due to advanced COPD. The patient decided to pursue comfort and hospice care
Discussion: Prior research has shown that EP is uncommon, with discovery during surgery and autopsies estimated at 0.25% to 0.55-13.7% respectively. Still rare is the frequency of malignant transformation, estimated at 0.7-1.8% of all EP cases. Studies have shown that patients with a malignancy in EP have higher rates of symptomatic disease as compared to non-ectopic primary pancreatic cancer.
A challenge in the diagnosis of malignant EP is the varying sites where ectopic tissue occurs. The most common location is the stomach (25-38%), followed by the duodenum (17-21%) and jejunum (15-21%), with other sites much less common. Our patients’ presentation of malignancy in EP tissue adjacent to D3 was exceedingly rare.
The prognosis of malignant EP remains unclear, primarily due to the rarity of this condition. Further research is needed to better evaluate and assess the natural course of the condition
Disclosures:
Brian Woods, BS1, Anthony Scholer, MD1, Robert Farrar, MD1, Veeral Oza, MD2. D0045 - All Nodules Are Not Equal: A Rare Presentation of Pancreatic Cancer, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Prisma Health, Greenville, SC; 2University of South Carolina School of Medicine Greenville, Prisma Health, Greenville, SC
Introduction: Pancreatic cancer has a 5-year survival of about 11%. An atypical presentation can make early diagnosis a challenge. Standard diagnostic measures such as computed tomography (CT) and endoscopy (EGD/EUS) may not provide enough information for diagnosis of a pancreatic cancer, particularly if presence of unusual anatomy was not previously known. In this case, we present a patient with adenocarcinoma developing in an ectopic pancreas (EP) adjacent to the third part of duodenum (D3)
Case Description/Methods: A 71-year-old female with past medical history of an abdominal aortic aneurysm, coronary artery disease, end-stage lung disease on home oxygen, hypertension, and chronic abdominal pain presented with abdominal pain and nausea. She had a CT scan which revealed a 10mm mesenteric nodule adjacent to D3. A follow-up study six weeks later revealed enlargement of the node to 13mm x 11mm (Fig 1a), and she was referred to surgery for evaluation. Patient was then referred to the gastroenterology for an endoscopic evaluation of what was initially thought to be a lymph node. An EGD/EUS revealed normal endoscopic findings, with a heterogenous periduodenal lesion measuring 3cm x 2.1cm was identified (Fig 1b). This was separate from the remainder of the pancreas. A biopsy of this lesion was performed.
Pathology revealed groups of crowded atypical glandular cells with anisonucleosis; consistent with a diagnosis of pancreatic tissue with well-differentiated adenocarcinoma (Fig1c,d). The patient was deemed to not be a surgical candidate due to advanced COPD. The patient decided to pursue comfort and hospice care
Discussion: Prior research has shown that EP is uncommon, with discovery during surgery and autopsies estimated at 0.25% to 0.55-13.7% respectively. Still rare is the frequency of malignant transformation, estimated at 0.7-1.8% of all EP cases. Studies have shown that patients with a malignancy in EP have higher rates of symptomatic disease as compared to non-ectopic primary pancreatic cancer.
A challenge in the diagnosis of malignant EP is the varying sites where ectopic tissue occurs. The most common location is the stomach (25-38%), followed by the duodenum (17-21%) and jejunum (15-21%), with other sites much less common. Our patients’ presentation of malignancy in EP tissue adjacent to D3 was exceedingly rare.
The prognosis of malignant EP remains unclear, primarily due to the rarity of this condition. Further research is needed to better evaluate and assess the natural course of the condition
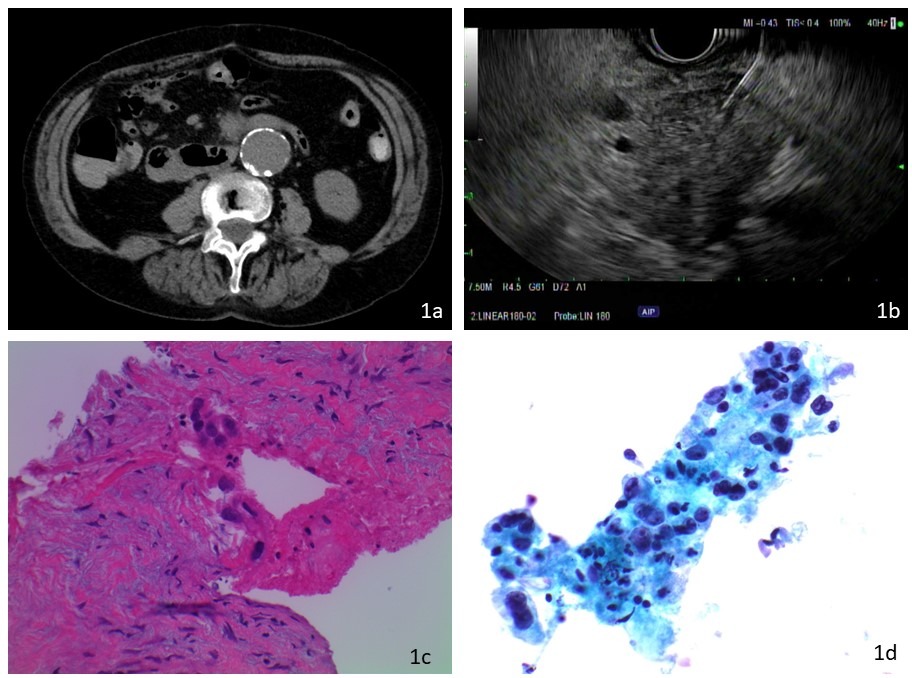
Figure: Fig 1a: CT scan showing the nodule; 1b: EUS image with nodule appearing as a hypoechoic lesion. Biopsy was performed. 1c: Pathologic staining, H&E (200x) show fibrotic / desmoplastic pancreatic tissue with irregular / abortive infiltrating glands with nuclear enlargement. 1d: Papanicolou staining at 400x magnification with similar findings
Disclosures:
Brian Woods indicated no relevant financial relationships.
Anthony Scholer indicated no relevant financial relationships.
Robert Farrar indicated no relevant financial relationships.
Veeral Oza: Boston Scientific – Consultant. S4 Medical – Advisor or Review Panel Member.
Brian Woods, BS1, Anthony Scholer, MD1, Robert Farrar, MD1, Veeral Oza, MD2. D0045 - All Nodules Are Not Equal: A Rare Presentation of Pancreatic Cancer, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
