Back

Poster Session A - Sunday Afternoon
Category: Stomach
A0714 - Agent Orange as a Possible Cause of Helicobacter pylori Negative Gastric Mucosa-Associated Lymphoid Tissue Lymphoma
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Samantha Wu, MD
Tulane University School of Medicine
New Orleans, LA
Presenting Author(s)
Samantha Wu, MD1, Justin Roy, MD1, Victoria Jackson, MD1, Vance Hartke, MD1, Leela Nayak, MD2
1Tulane University School of Medicine, New Orleans, LA; 2VA Southeast Louisiana Health Care, New Orleans, LA
Introduction: Gastric mucosa-associated lymphoid tissue (MALT) lymphoma was first described in 1983 as the most common extranodal site of non-Hodgkin lymphoma. Helicobacter pylori (H. pylori) infection is implicated in 90% of all gastric MALT lymphoma cases. Agent Orange (AO), with traces of oncogenic 2,3,7,8-tetrachlorodibenzo-p-dioxin, has also been classified as a causative agent in non-Hodgkin lymphoma, which includes gastric MALT lymphoma. Here we report a case of H. pylori negative gastric MALT lymphoma in a patient with history of significant AO exposure.
Case Description/Methods: A 75-year-old Caucasian male veteran who served in the Vietnam War with significant AO exposure, as well as history of chronic gastroesophageal reflux disease, was referred for endoscopy to evaluate a reported history of un-staged Barrett’s esophagus 5-years prior but with two subsequent normal endoscopies at an outside facility. He noted symptoms of burning chest pain and dyspepsia following large meals, all of which were worsened with spicy foods and improved with omeprazole. Family history was negative for a history of gastric cancer, and he had a 25-pack year smoking history but quit 20 years prior to presentation.
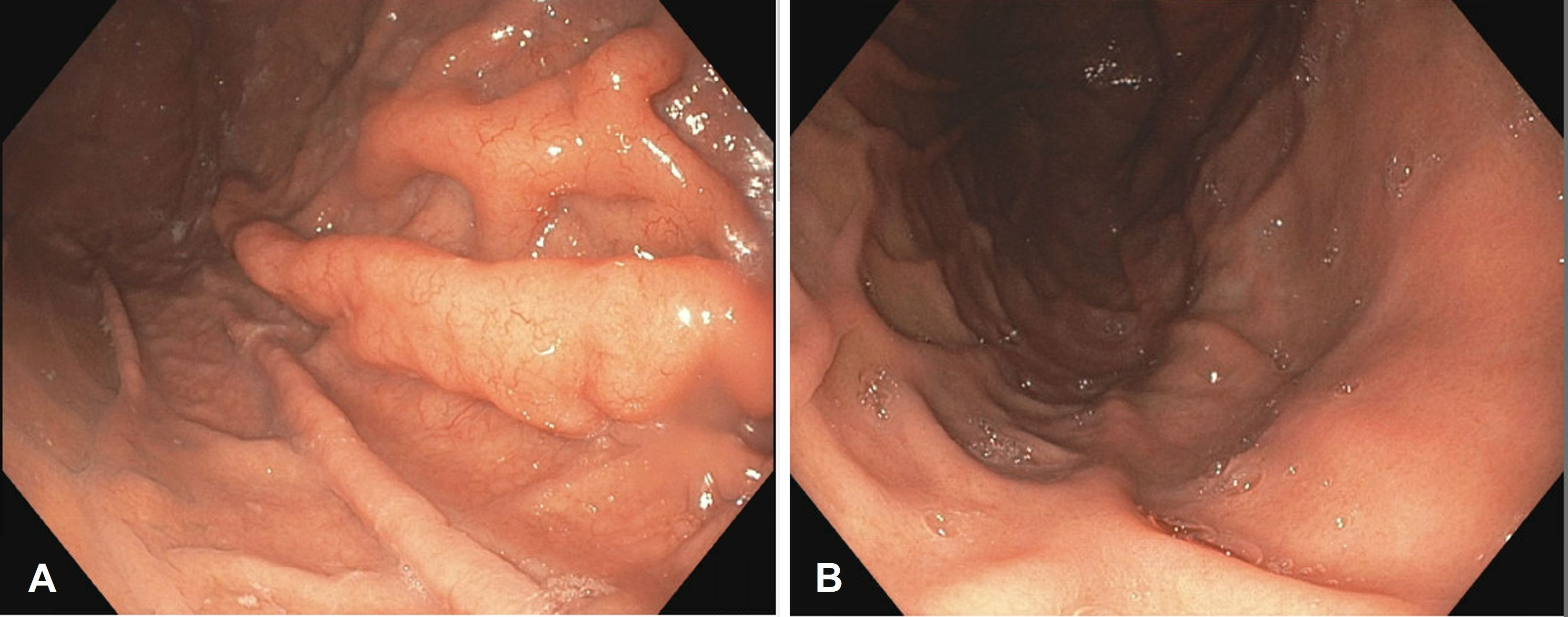
Initial esophagogastroduodenoscopy (EGD) revealed abnormal folds in the gastric fundus and erythema in the gastric antrum, but otherwise normal exam including normal duodenum and esophagus. Random gastric biopsies and biopsies of the abnormal folds were consistent with gastric MALT lymphoma, negative for H. pylori and t(11;18)(q21;q21). Repeat EGD 1 month later for further sampling demonstrated identical findings (Figure 1A). Stool testing for H. pylori antigen was also negative.
The patient was referred to oncology and after staging imaging was found to have stage IE gastric MALT lymphoma. He was treated with involved site radiation therapy and EGD 3 months later showed both endoscopic and pathologic resolution (Figure 1B).
Discussion: The 10% of cases of H. pylori negative gastric MALT lymphoma have an unclear etiology, although dysregulation of nuclear factor-kappa B (NF-κB) principally via translocations t(11;18)(q21;q21) is thought to be a potentially causative genetic alteration. In this patient, neither H. pylori nor the common t(11,18) genetic alteration were present. Given AO is implicated in non-Hodgkin lymphoma and the most common site of extranodal non-Hodgkin lymphoma is the gastric mucosa, AO exposure should be considered a risk factor for development of gastric MALT lymphoma.
Disclosures:
Samantha Wu, MD1, Justin Roy, MD1, Victoria Jackson, MD1, Vance Hartke, MD1, Leela Nayak, MD2. A0714 - Agent Orange as a Possible Cause of Helicobacter pylori Negative Gastric Mucosa-Associated Lymphoid Tissue Lymphoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Tulane University School of Medicine, New Orleans, LA; 2VA Southeast Louisiana Health Care, New Orleans, LA
Introduction: Gastric mucosa-associated lymphoid tissue (MALT) lymphoma was first described in 1983 as the most common extranodal site of non-Hodgkin lymphoma. Helicobacter pylori (H. pylori) infection is implicated in 90% of all gastric MALT lymphoma cases. Agent Orange (AO), with traces of oncogenic 2,3,7,8-tetrachlorodibenzo-p-dioxin, has also been classified as a causative agent in non-Hodgkin lymphoma, which includes gastric MALT lymphoma. Here we report a case of H. pylori negative gastric MALT lymphoma in a patient with history of significant AO exposure.
Case Description/Methods: A 75-year-old Caucasian male veteran who served in the Vietnam War with significant AO exposure, as well as history of chronic gastroesophageal reflux disease, was referred for endoscopy to evaluate a reported history of un-staged Barrett’s esophagus 5-years prior but with two subsequent normal endoscopies at an outside facility. He noted symptoms of burning chest pain and dyspepsia following large meals, all of which were worsened with spicy foods and improved with omeprazole. Family history was negative for a history of gastric cancer, and he had a 25-pack year smoking history but quit 20 years prior to presentation.
Initial esophagogastroduodenoscopy (EGD) revealed abnormal folds in the gastric fundus and erythema in the gastric antrum, but otherwise normal exam including normal duodenum and esophagus. Random gastric biopsies and biopsies of the abnormal folds were consistent with gastric MALT lymphoma, negative for H. pylori and t(11;18)(q21;q21). Repeat EGD 1 month later for further sampling demonstrated identical findings (Figure 1A). Stool testing for H. pylori antigen was also negative.
The patient was referred to oncology and after staging imaging was found to have stage IE gastric MALT lymphoma. He was treated with involved site radiation therapy and EGD 3 months later showed both endoscopic and pathologic resolution (Figure 1B).
Discussion: The 10% of cases of H. pylori negative gastric MALT lymphoma have an unclear etiology, although dysregulation of nuclear factor-kappa B (NF-κB) principally via translocations t(11;18)(q21;q21) is thought to be a potentially causative genetic alteration. In this patient, neither H. pylori nor the common t(11,18) genetic alteration were present. Given AO is implicated in non-Hodgkin lymphoma and the most common site of extranodal non-Hodgkin lymphoma is the gastric mucosa, AO exposure should be considered a risk factor for development of gastric MALT lymphoma.
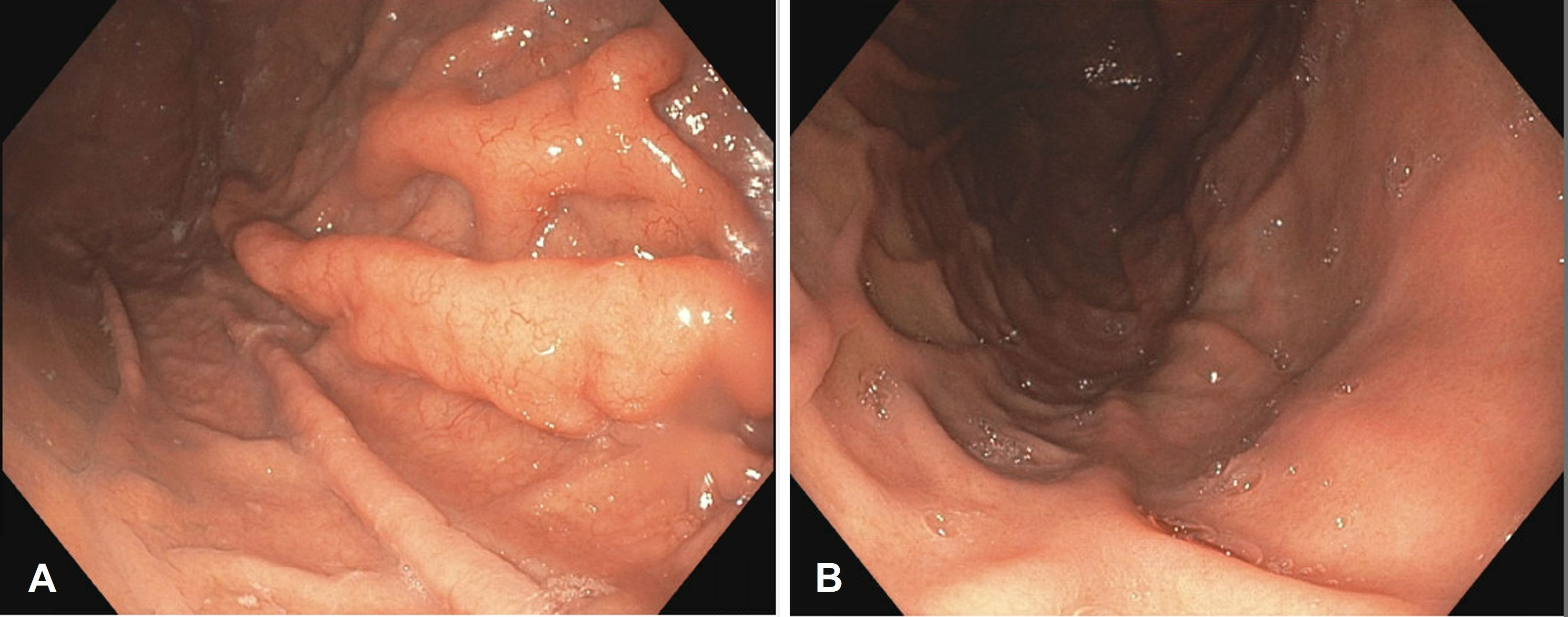
Figure: Figure 1 A&B. (A) EGD demonstrating abnormal gastric mucosa with prominent gastric fundus folds seen on retroflexion during EGD prior to ISRT (radiation) therapy. (B) Post-radiation EGD demonstrating resolution of the abnormalities seen with the pre-treatment EGD including disappearance of the prominent gastric fundus folds.
Disclosures:
Samantha Wu indicated no relevant financial relationships.
Justin Roy indicated no relevant financial relationships.
Victoria Jackson indicated no relevant financial relationships.
Vance Hartke indicated no relevant financial relationships.
Leela Nayak indicated no relevant financial relationships.
Samantha Wu, MD1, Justin Roy, MD1, Victoria Jackson, MD1, Vance Hartke, MD1, Leela Nayak, MD2. A0714 - Agent Orange as a Possible Cause of Helicobacter pylori Negative Gastric Mucosa-Associated Lymphoid Tissue Lymphoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
