Back

Poster Session D - Tuesday Morning
Category: Biliary/Pancreas
D0063 - Emergent Decompressive ERCP or Not; Go With Your Gut
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- MM
Maryam Mubashir, MD
Louisiana State University Health Sciences Center
Shreveport, LA
Presenting Author(s)
Maryam Mubashir, MBBS1, Daniyal Raza, MD2, Syed Musa Raza, MD3, Philip Bouchette, MD3, Shazia Rashid, MD4, Nushra Paracha, DO5, Bohdan Zoshchuk, MD1, James Morris, MD, FACG6, Sudha Pandit, MD4
1O-LSUS, Shreveport, LA; 2Louisiana State University, Shreveport, LA; 3Louisiana State University Health Sciences Center, Shreveport, LA; 4LSUHSC, Shreveport, LA; 5Lincoln Medical Center, Bronx, NY; 6LSU Health Sciences Center, Shreveport, LA
Introduction: Acute Cholangitis is a biliary emergency that requires prompt diagnosis & appropriate management in a timely manner. Guidelines and best practices dictate that if the Charcot's triad and Tokyo guidelines are indicating moderate to severe cholangitis, ERCP should be performed urgently. In certain situations however, clinical decision making is not as straight forward. We present a case in which a number of confounding factors caused hesitancy in making that decision.
Case Description/Methods: 38-year female with PMH of Crohn’s colitis on adalimumab presented with 2 weeks of progressively worsening upper abdominal pain associated with decreased appetite, nausea, vomiting, change in urine color and chills but no fevers. She completed a course of Augmentin 20 days back for a URI. She was also recovering from alcohol use disorder. She was afebrile and hemodynamically stable. On exam, had marked scleral icterus, palpable liver, spleen with upper abdominal tenderness. Lab were remarkable for lymphocytic leukocytosis, thrombocytopenia and Alk phos 316 U/L, T and DBilirubin-7/6.3 mg/dL, AST/ALT-72/131 U/L, respectively. CT abdomen pelvis with contrast showed no intra-or extrahepatic biliary ductal dilation and moderate hepatosplenomegaly. Ultrasound liver with Doppler confirmed above. GI team was called to evaluate for possible ERCP for cholangitis. Later Peripheral smear which was initially ordered to evaluate low platelets, showed blasts cells following which flow cytometry and bone marrow biopsy confirmed B-lymphoblastic leukemia with BCR-ABL1 fusion 97% of cellularity by differential count. Liver enzymes normalized after initiation of R-HyperCVAD.
Discussion:
Disclosures:
Maryam Mubashir, MBBS1, Daniyal Raza, MD2, Syed Musa Raza, MD3, Philip Bouchette, MD3, Shazia Rashid, MD4, Nushra Paracha, DO5, Bohdan Zoshchuk, MD1, James Morris, MD, FACG6, Sudha Pandit, MD4. D0063 - Emergent Decompressive ERCP or Not; Go With Your Gut, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1O-LSUS, Shreveport, LA; 2Louisiana State University, Shreveport, LA; 3Louisiana State University Health Sciences Center, Shreveport, LA; 4LSUHSC, Shreveport, LA; 5Lincoln Medical Center, Bronx, NY; 6LSU Health Sciences Center, Shreveport, LA
Introduction: Acute Cholangitis is a biliary emergency that requires prompt diagnosis & appropriate management in a timely manner. Guidelines and best practices dictate that if the Charcot's triad and Tokyo guidelines are indicating moderate to severe cholangitis, ERCP should be performed urgently. In certain situations however, clinical decision making is not as straight forward. We present a case in which a number of confounding factors caused hesitancy in making that decision.
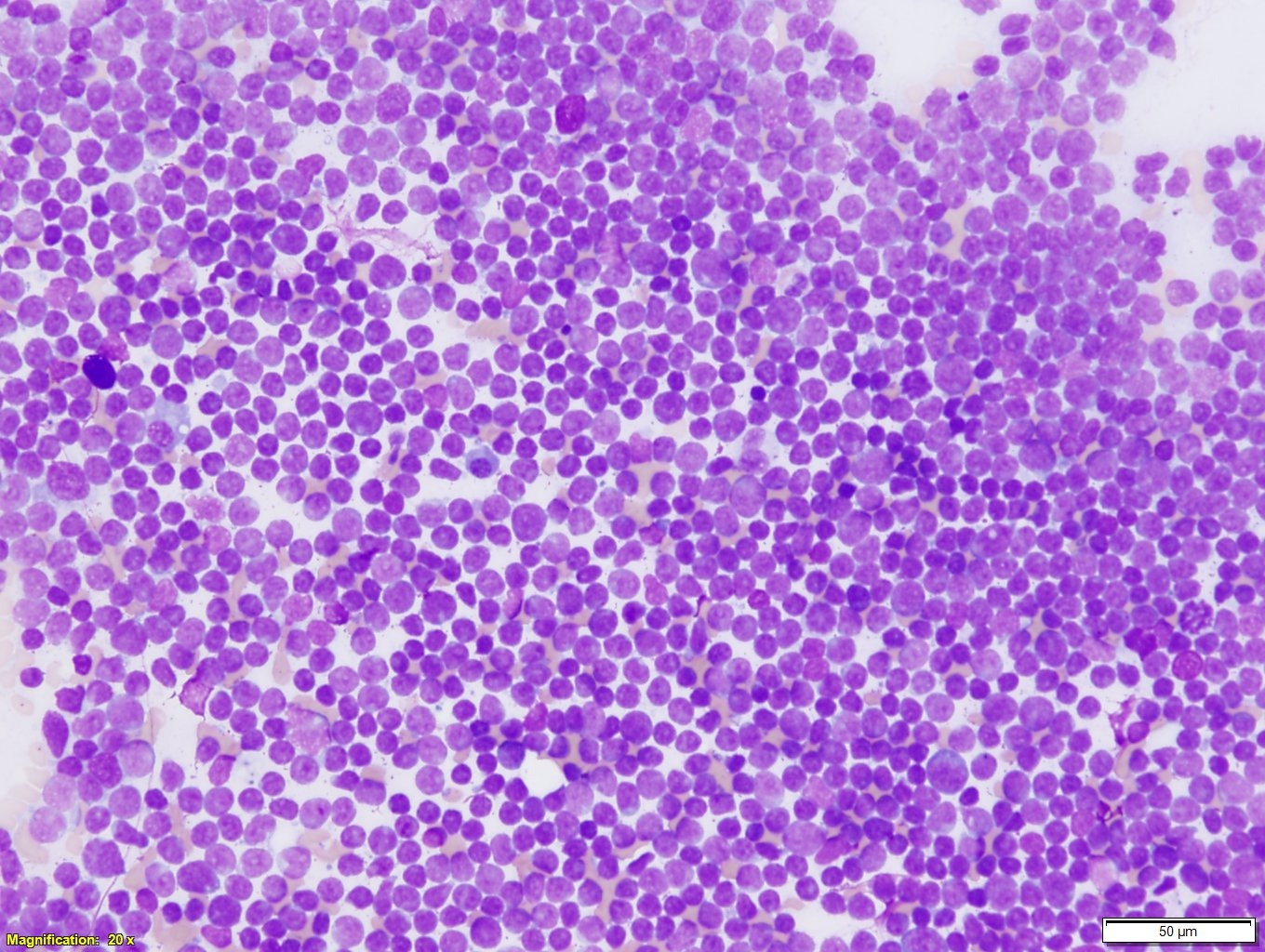
Case Description/Methods: 38-year female with PMH of Crohn’s colitis on adalimumab presented with 2 weeks of progressively worsening upper abdominal pain associated with decreased appetite, nausea, vomiting, change in urine color and chills but no fevers. She completed a course of Augmentin 20 days back for a URI. She was also recovering from alcohol use disorder. She was afebrile and hemodynamically stable. On exam, had marked scleral icterus, palpable liver, spleen with upper abdominal tenderness. Lab were remarkable for lymphocytic leukocytosis, thrombocytopenia and Alk phos 316 U/L, T and DBilirubin-7/6.3 mg/dL, AST/ALT-72/131 U/L, respectively. CT abdomen pelvis with contrast showed no intra-or extrahepatic biliary ductal dilation and moderate hepatosplenomegaly. Ultrasound liver with Doppler confirmed above. GI team was called to evaluate for possible ERCP for cholangitis. Later Peripheral smear which was initially ordered to evaluate low platelets, showed blasts cells following which flow cytometry and bone marrow biopsy confirmed B-lymphoblastic leukemia with BCR-ABL1 fusion 97% of cellularity by differential count. Liver enzymes normalized after initiation of R-HyperCVAD.
Discussion:
Intrahepatic cholestasis is a known phenomenon in ALL, however initial presentation with intrahepatic cholestasis is rare except for few reported cases in pediatric population. Leukemic infiltration causing intrahepatic cholestasis causes an important diagnostic dilemma and establishing correct diagnosis has important implications especially since the treatment of choice, ERCP, for the alternate diagnosis is not only invasive but the risk of adverse events is high. Keeping this in mind hematologic malignancies should always be considered as a differential in patients with constitutional symptoms and hepatosplenomegaly. The diagnosis can be confirmed by immunohistochemical stains showing immature B cell lineage from a Liver biopsy; however, it is not necessary as in above case. Systemic chemotherapy is the main treatment for B-ALL/LBL.
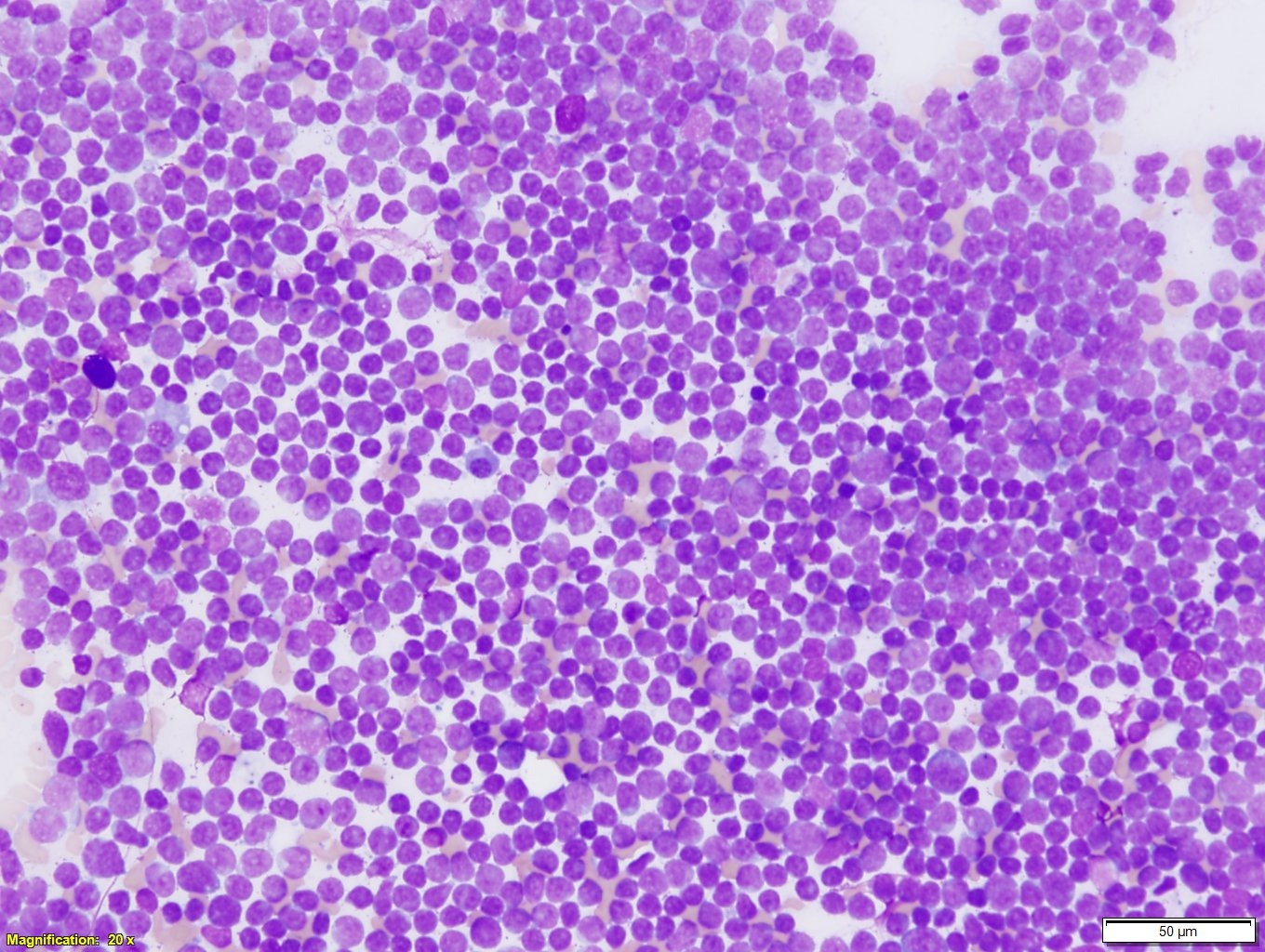
Figure: Bone Marrow Smear
Disclosures:
Maryam Mubashir indicated no relevant financial relationships.
Daniyal Raza indicated no relevant financial relationships.
Syed Musa Raza indicated no relevant financial relationships.
Philip Bouchette indicated no relevant financial relationships.
Shazia Rashid indicated no relevant financial relationships.
Nushra Paracha indicated no relevant financial relationships.
Bohdan Zoshchuk indicated no relevant financial relationships.
James Morris: Celgene – Grant/Research Support.
Sudha Pandit indicated no relevant financial relationships.
Maryam Mubashir, MBBS1, Daniyal Raza, MD2, Syed Musa Raza, MD3, Philip Bouchette, MD3, Shazia Rashid, MD4, Nushra Paracha, DO5, Bohdan Zoshchuk, MD1, James Morris, MD, FACG6, Sudha Pandit, MD4. D0063 - Emergent Decompressive ERCP or Not; Go With Your Gut, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
