Back

Poster Session D - Tuesday Morning
Category: Biliary/Pancreas
D0082 - Acute Pancreatitis After Liver Biopsy: Clots or Stones?
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Andrea Fernandez, MD
University of Oklahoma Health Sciences Center
Oklahoma City, OK
Presenting Author(s)
Andrea Fernandez, MD, Hashroop Gurm, MD, Ijlal Akbar Ali, MD
University of Oklahoma Health Sciences Center, Oklahoma City, OK
Introduction: Percutaneous liver biopsy is a frequently utilized tool in the diagnosis of many liver diseases including metastatic liver lesions. Bleeding complications occur in 1% of cases and hemobilia is rare. Hemobilia causing acute pancreatitis after percutaneous liver biopsy is extremely rare with approximately 20 reported cases in literature. Symptoms include right upper quadrant pain, nausea, jaundice, hematemesis, hematochezia or melena. We present an interesting case of a woman who developed acute pancreatitis secondary to hemobilia after liver biopsy.
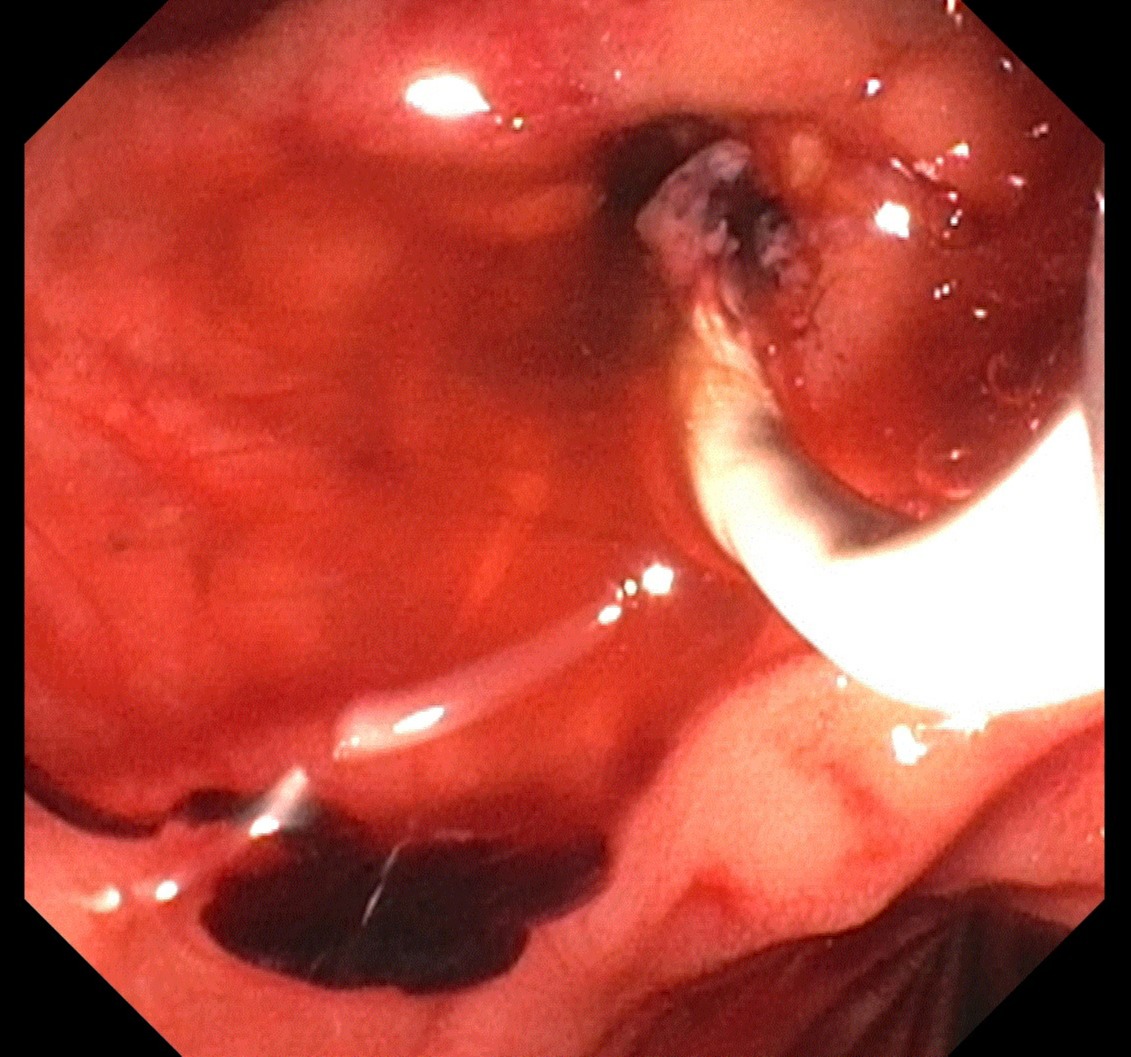
Case Description/Methods: A 60-year-old female with recurrent high-grade serious peritoneal cancer and recent metastases to liver was admitted for acute pancreatitis. Patient presented with nausea and right upper quadrant pain that started after percutaneous liver biopsy one day prior. Labs notable for Hgb 10.4, lipase > 3000, amylase 3349, total bilirubin 3.6, direct 3.3, AST 631, ALT 482, alkaline phosphatase 240. CT A/P showed diffuse swelling of pancreas with fluid and mesenteric fat stranding suspicious for acute pancreatitis. Given liver enzyme elevation with mixed hepatocellular and cholestasis pattern, abdominal MRI was obtained to evaluate any biliary obstruction. MRI showed mildly prominent CBD at 0.8 cm with debris in distal CBD, cystic duct, and gallbladder indicative of hemorrhagic products. No hematoma noted in the liver parenchyma. Patient underwent ERCP with sphincterotomy and clots were cleared from the duct with balloon sweep (Figure A).
Discussion: Hemobilia, described as upper GI bleeding within the biliary tree has a reported incidence of less than 0.059% after percutaneous liver biopsy. It can occur within a few hours or several days later, with an average interval of five days. Although rare, hemobilia can lead to acute pancreatitis in a mechanism similar to gallstone pancreatitis. Excessive bleeding and increased clot formation cause obstruction in the biliary tree and impedes drainage from the ampulla which in turn triggers pancreatitis. Diagnosis can be made by ultrasound, angiography, ERCP, or MRCP. Treatment depends on the extent of bleeding and includes conservative management to advanced interventions-hepatic angiography with arterial embolization, ERCP with sphincterotomy or stent placement. Thus, our case highlights importance of recognizing hemobilia as an etiology for acute pancreatitis after percutaneous liver biopsy.
Disclosures:
Andrea Fernandez, MD, Hashroop Gurm, MD, Ijlal Akbar Ali, MD. D0082 - Acute Pancreatitis After Liver Biopsy: Clots or Stones?, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Oklahoma Health Sciences Center, Oklahoma City, OK
Introduction: Percutaneous liver biopsy is a frequently utilized tool in the diagnosis of many liver diseases including metastatic liver lesions. Bleeding complications occur in 1% of cases and hemobilia is rare. Hemobilia causing acute pancreatitis after percutaneous liver biopsy is extremely rare with approximately 20 reported cases in literature. Symptoms include right upper quadrant pain, nausea, jaundice, hematemesis, hematochezia or melena. We present an interesting case of a woman who developed acute pancreatitis secondary to hemobilia after liver biopsy.
Case Description/Methods: A 60-year-old female with recurrent high-grade serious peritoneal cancer and recent metastases to liver was admitted for acute pancreatitis. Patient presented with nausea and right upper quadrant pain that started after percutaneous liver biopsy one day prior. Labs notable for Hgb 10.4, lipase > 3000, amylase 3349, total bilirubin 3.6, direct 3.3, AST 631, ALT 482, alkaline phosphatase 240. CT A/P showed diffuse swelling of pancreas with fluid and mesenteric fat stranding suspicious for acute pancreatitis. Given liver enzyme elevation with mixed hepatocellular and cholestasis pattern, abdominal MRI was obtained to evaluate any biliary obstruction. MRI showed mildly prominent CBD at 0.8 cm with debris in distal CBD, cystic duct, and gallbladder indicative of hemorrhagic products. No hematoma noted in the liver parenchyma. Patient underwent ERCP with sphincterotomy and clots were cleared from the duct with balloon sweep (Figure A).
Discussion: Hemobilia, described as upper GI bleeding within the biliary tree has a reported incidence of less than 0.059% after percutaneous liver biopsy. It can occur within a few hours or several days later, with an average interval of five days. Although rare, hemobilia can lead to acute pancreatitis in a mechanism similar to gallstone pancreatitis. Excessive bleeding and increased clot formation cause obstruction in the biliary tree and impedes drainage from the ampulla which in turn triggers pancreatitis. Diagnosis can be made by ultrasound, angiography, ERCP, or MRCP. Treatment depends on the extent of bleeding and includes conservative management to advanced interventions-hepatic angiography with arterial embolization, ERCP with sphincterotomy or stent placement. Thus, our case highlights importance of recognizing hemobilia as an etiology for acute pancreatitis after percutaneous liver biopsy.
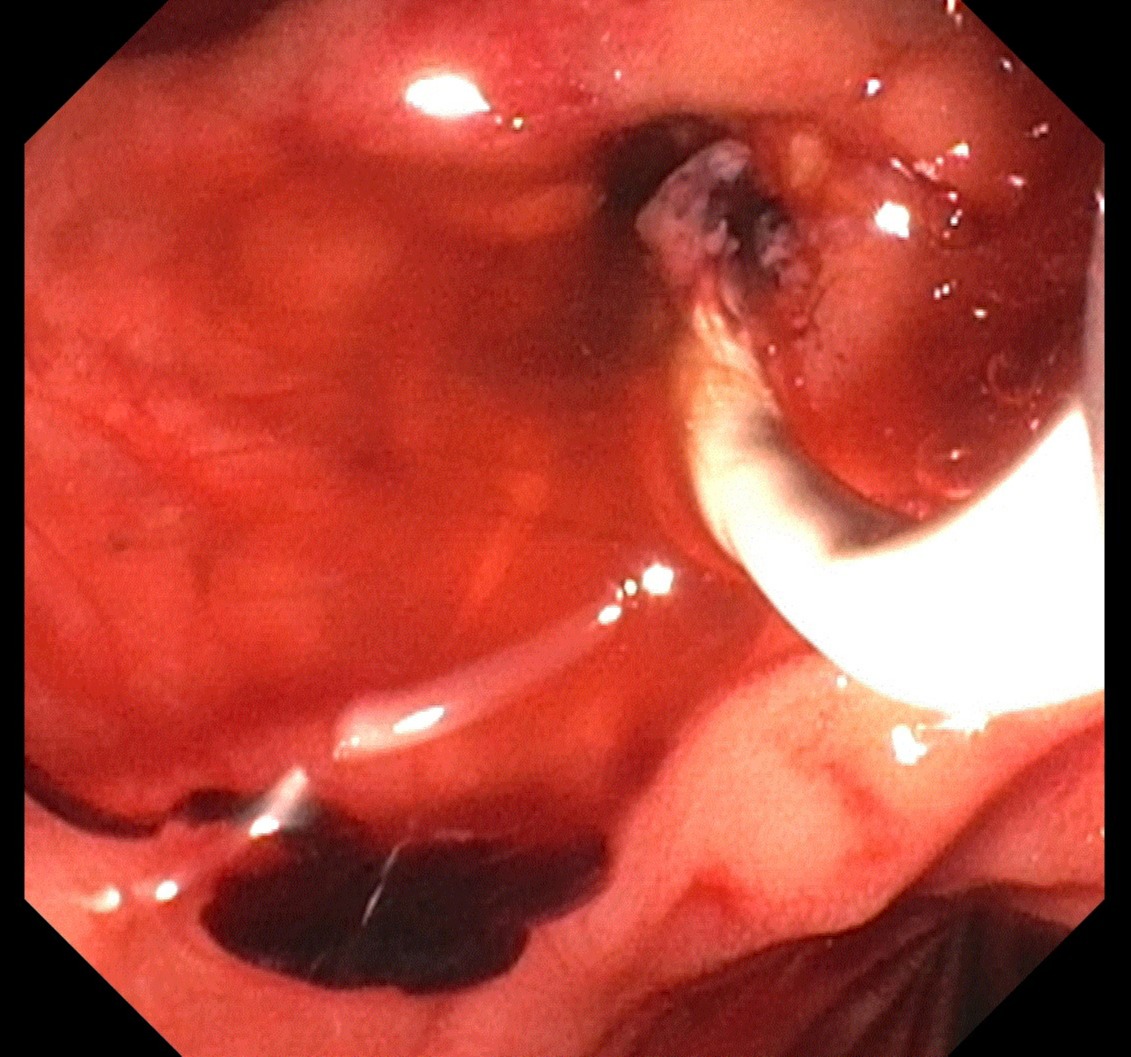
Figure: Figure A: Removal of blood clots from bile duct by balloon sweep via ERCP
Disclosures:
Andrea Fernandez indicated no relevant financial relationships.
Hashroop Gurm indicated no relevant financial relationships.
Ijlal Akbar Ali indicated no relevant financial relationships.
Andrea Fernandez, MD, Hashroop Gurm, MD, Ijlal Akbar Ali, MD. D0082 - Acute Pancreatitis After Liver Biopsy: Clots or Stones?, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
