Back

Poster Session A - Sunday Afternoon
Category: Esophagus
A0222 - An Unexpected Finding of a Black Esophagus: Atypical Presentation of Acute Esophageal Necrosis
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
.jpg)
Jessica Strzepka, MD
Rush University Medical Center
Chicago, IL
Presenting Author(s)
Jessica Strzepka, MD, Matthew Kroll, MD, Allison P. Rzepczynski, MD, David Cimbaluk, MD, Mark Demeo, MD
Rush University Medical Center, Chicago, IL
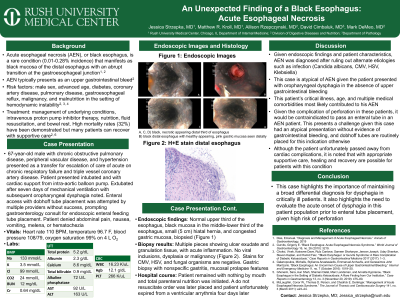
Introduction: Acute esophageal necrosis (AEN), or black esophagus, is a rare condition that manifests as black mucosa of the distal esophagus with an abrupt transition at the gastroesophageal junction. AEN typically presents as an upper gastrointestinal bleed. Risk factors include male sex, advanced age, diabetes, coronary artery disease, pulmonary disease, gastroesophageal reflux, malignancy, and malnutrition in the setting of hemodynamic instability. Treatment includes management of underlying conditions, intravenous proton pump inhibitor therapy, nutrition, fluid resuscitation, and bowel rest. High mortality rates have been demonstrated but many patients can recover with supportive care.
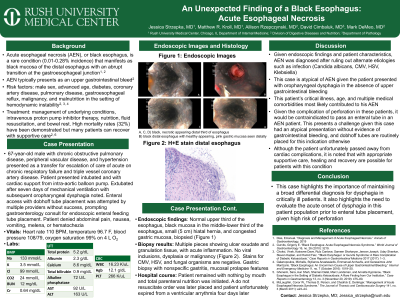
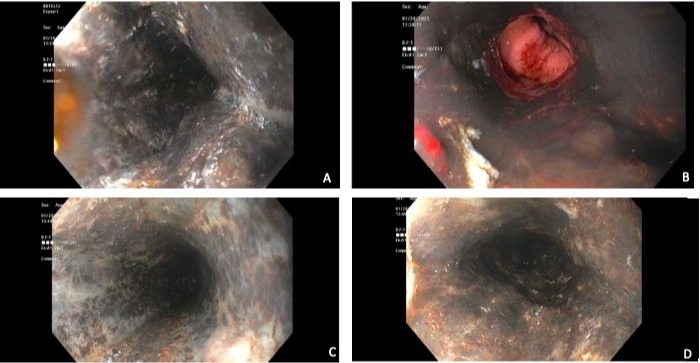
Case Description/Methods: A 67-year-old male with chronic obstructive pulmonary disease, peripheral vascular disease, and hypertension presented as a transfer for escalation of care of acute on chronic respiratory failure and triple vessel coronary artery disease. After seven days of mechanical ventilation, the patient experienced oropharyngeal dysphagia and failed a swallow evaluation. Enteral access with dobhoff tube placement was attempted without success, prompting gastroenterology consult for endoscopic placement. He was tachycardic, normotensive, afebrile, and saturating well on 4 L nasal cannula. Labs showed a hemoglobin of 12 g/dL, blood urea nitrogen 12 mg/dL, and creatinine 0.64 mg/dL. He denied abdominal pain, vomiting, melena, or hematochezia. Endoscopy showed a normal upper third of the esophagus with distal black mucosa, and an abrupt transition at the gastroesophageal mucosa. Biopsy showed ulcer exudate and granulation tissue with acute inflammation, negative for CMV, HSV, or fungal organisms. Patient remained with nothing by mouth and on total parenteral nutrition. A do not resuscitate order was placed and the patient unfortunately expired from a ventricular arrythmia four days later.
Discussion: This case demonstrates an unexpected finding of AEN in a patient presenting atypically with oropharyngeal dysphagia in the absence of obvious upper gastrointestinal bleeding. This patient’s critical illness, age, and multiple medical comorbidities most likely contributed to his AEN. This case highlights the importance of maintaining a broad differential diagnosis for dysphagia in critically ill patients. It also highlights the need to evaluate the acute onset of dysphagia in this patient population prior to enteral tube placement, given high risk of perforation.
Disclosures:
Jessica Strzepka, MD, Matthew Kroll, MD, Allison P. Rzepczynski, MD, David Cimbaluk, MD, Mark Demeo, MD. A0222 - An Unexpected Finding of a Black Esophagus: Atypical Presentation of Acute Esophageal Necrosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Rush University Medical Center, Chicago, IL
Introduction: Acute esophageal necrosis (AEN), or black esophagus, is a rare condition that manifests as black mucosa of the distal esophagus with an abrupt transition at the gastroesophageal junction. AEN typically presents as an upper gastrointestinal bleed. Risk factors include male sex, advanced age, diabetes, coronary artery disease, pulmonary disease, gastroesophageal reflux, malignancy, and malnutrition in the setting of hemodynamic instability. Treatment includes management of underlying conditions, intravenous proton pump inhibitor therapy, nutrition, fluid resuscitation, and bowel rest. High mortality rates have been demonstrated but many patients can recover with supportive care.
Case Description/Methods: A 67-year-old male with chronic obstructive pulmonary disease, peripheral vascular disease, and hypertension presented as a transfer for escalation of care of acute on chronic respiratory failure and triple vessel coronary artery disease. After seven days of mechanical ventilation, the patient experienced oropharyngeal dysphagia and failed a swallow evaluation. Enteral access with dobhoff tube placement was attempted without success, prompting gastroenterology consult for endoscopic placement. He was tachycardic, normotensive, afebrile, and saturating well on 4 L nasal cannula. Labs showed a hemoglobin of 12 g/dL, blood urea nitrogen 12 mg/dL, and creatinine 0.64 mg/dL. He denied abdominal pain, vomiting, melena, or hematochezia. Endoscopy showed a normal upper third of the esophagus with distal black mucosa, and an abrupt transition at the gastroesophageal mucosa. Biopsy showed ulcer exudate and granulation tissue with acute inflammation, negative for CMV, HSV, or fungal organisms. Patient remained with nothing by mouth and on total parenteral nutrition. A do not resuscitate order was placed and the patient unfortunately expired from a ventricular arrythmia four days later.
Discussion: This case demonstrates an unexpected finding of AEN in a patient presenting atypically with oropharyngeal dysphagia in the absence of obvious upper gastrointestinal bleeding. This patient’s critical illness, age, and multiple medical comorbidities most likely contributed to his AEN. This case highlights the importance of maintaining a broad differential diagnosis for dysphagia in critically ill patients. It also highlights the need to evaluate the acute onset of dysphagia in this patient population prior to enteral tube placement, given high risk of perforation.
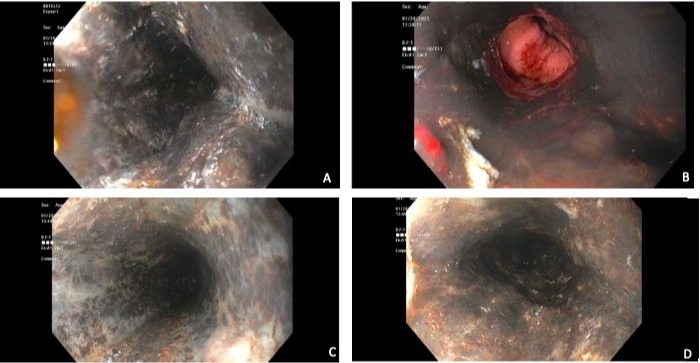
Figure: A, C, D) black, necrotic appearing distal esophagus B) black, necrotic appearing distal esophagus with abrupt transition at the gastroesophageal junction
Disclosures:
Jessica Strzepka indicated no relevant financial relationships.
Matthew Kroll indicated no relevant financial relationships.
Allison Rzepczynski indicated no relevant financial relationships.
David Cimbaluk indicated no relevant financial relationships.
Mark Demeo indicated no relevant financial relationships.
Jessica Strzepka, MD, Matthew Kroll, MD, Allison P. Rzepczynski, MD, David Cimbaluk, MD, Mark Demeo, MD. A0222 - An Unexpected Finding of a Black Esophagus: Atypical Presentation of Acute Esophageal Necrosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
