Back

Poster Session B - Monday Morning
Category: Stomach
B0722 - Eosinophilic Gastritis With Antral Pseudopolyps
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Matthew L. Silverman, MD
Wright State University and the United States Air Force
Wright Patterson AFB, Ohio
Presenting Author(s)
Matthew L. Silverman, MD1, Christopher Casaccio, DO1, Michael Brazeau, DO2
1Wright State University and the United States Air Force, Wright Patterson AFB, OH; 2United States Air Force, Wright Patterson AFB, Wright Patterson AFB, OH
Introduction: Eosinophilic gastritis (EG) is a rare disease distinguished by eosinophilic infiltration likely due to antigen driven humoral immunity affecting about 6 in 100,000 people. Diagnosis and treatment are often challenging due to the heterogeneity of manifestations and endoscopic findings. This case highlights a severe variant of EG.
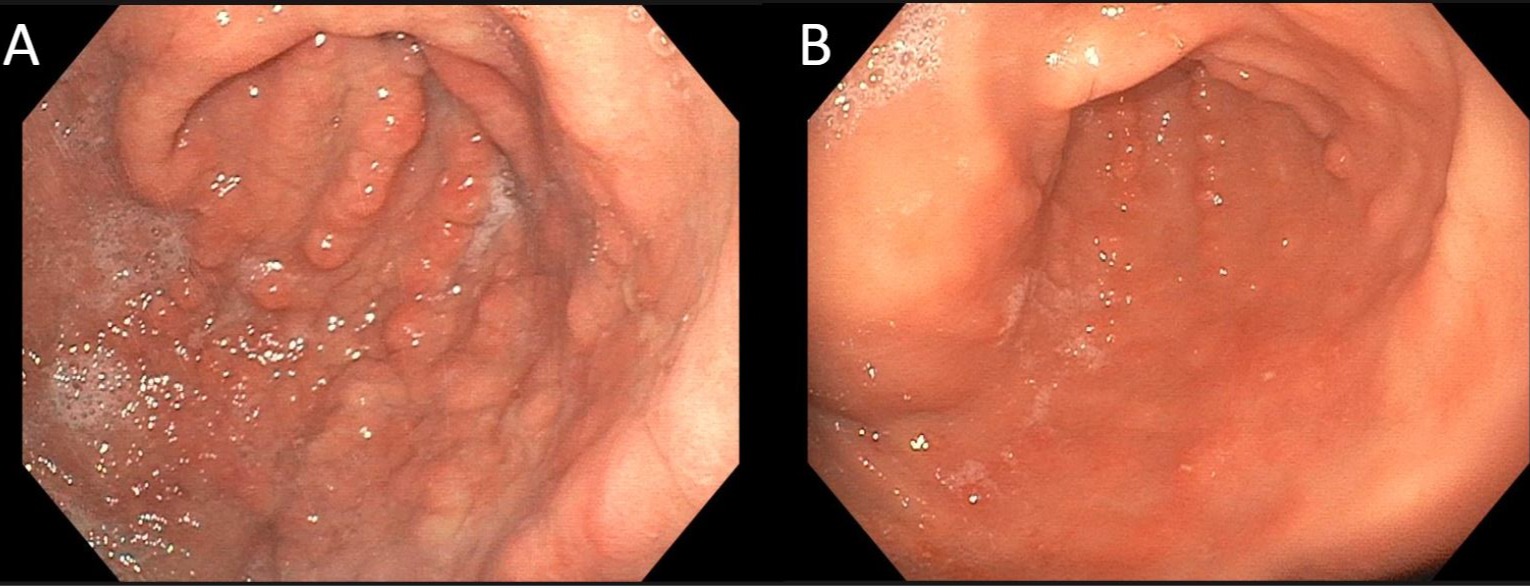
Case Description/Methods: A 20-year-old man with a history of atopy presented initially with bilateral lower extremity edema of 1 year duration. Initial workup was significant for hypoalbuminemia 2.5g/dL, iron deficiency anemia 8.5g/dL, and leukocytosis with eosinophilia >8 times the upper limit of normal. Liver function tests and Helicobacter pylorii serum antibody were unremarkable. He had one year of nausea and emesis associated with egg consumption but denied abdominal pain, constipation, or signs of blood loss. He was referred to gastroenterology where a colonoscopy was unremarkable and esophagogastroduodenoscopy showed innumerable 3-7 mm semi-pedunculated polyps in the gastric antrum (Figure 1). The duodenal bulb was unremarkable other than a single 3-5 mm polyp. Pathology showed marked gastric eosinophilic infiltration and normal duodenal mucosa. EG was diagnosed and the patient was started on a six-food elimination diet and Prednisone 40 mg for 2 weeks followed by a taper. Repeat EGD at 1 month showed 75% reduction in polyp burden. His anemia and hypoalbuminemia continue to improve though ongoing surveillance has shown persistent mild disease.
Discussion: The most common presenting symptoms of EG are nausea, vomiting, and abdominal pain. Weight loss, failure to thrive, hypoalbuminemia, and iron deficiency anemia in EG have been reported but poorly characterized as malabsorptive complications. In patients such as this with symptomatic edema and anemia, it is important to consider EG as a mucosal infiltrative disease that can induce such a malabsorptive syndrome.
The endoscopic findings in EG are variable and few prospective studies have elucidated the breadth of possible findings. Gastric pseudo-polyps have been described in case reports and are likely a high-severity feature of EG, correlating with this patient’s manifestations. However, as normal mucosa or erythema are the most common findings, random biopsies are important in its diagnosis. Pseudo-polyps also prove a clinical challenge in this demographic as polyposis syndromes must be considered. Histopathologic evaluation and region of involvement are important differentiators of EG from polyposis syndromes.
Disclosures:
Matthew L. Silverman, MD1, Christopher Casaccio, DO1, Michael Brazeau, DO2. B0722 - Eosinophilic Gastritis With Antral Pseudopolyps, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Wright State University and the United States Air Force, Wright Patterson AFB, OH; 2United States Air Force, Wright Patterson AFB, Wright Patterson AFB, OH
Introduction: Eosinophilic gastritis (EG) is a rare disease distinguished by eosinophilic infiltration likely due to antigen driven humoral immunity affecting about 6 in 100,000 people. Diagnosis and treatment are often challenging due to the heterogeneity of manifestations and endoscopic findings. This case highlights a severe variant of EG.
Case Description/Methods: A 20-year-old man with a history of atopy presented initially with bilateral lower extremity edema of 1 year duration. Initial workup was significant for hypoalbuminemia 2.5g/dL, iron deficiency anemia 8.5g/dL, and leukocytosis with eosinophilia >8 times the upper limit of normal. Liver function tests and Helicobacter pylorii serum antibody were unremarkable. He had one year of nausea and emesis associated with egg consumption but denied abdominal pain, constipation, or signs of blood loss. He was referred to gastroenterology where a colonoscopy was unremarkable and esophagogastroduodenoscopy showed innumerable 3-7 mm semi-pedunculated polyps in the gastric antrum (Figure 1). The duodenal bulb was unremarkable other than a single 3-5 mm polyp. Pathology showed marked gastric eosinophilic infiltration and normal duodenal mucosa. EG was diagnosed and the patient was started on a six-food elimination diet and Prednisone 40 mg for 2 weeks followed by a taper. Repeat EGD at 1 month showed 75% reduction in polyp burden. His anemia and hypoalbuminemia continue to improve though ongoing surveillance has shown persistent mild disease.
Discussion: The most common presenting symptoms of EG are nausea, vomiting, and abdominal pain. Weight loss, failure to thrive, hypoalbuminemia, and iron deficiency anemia in EG have been reported but poorly characterized as malabsorptive complications. In patients such as this with symptomatic edema and anemia, it is important to consider EG as a mucosal infiltrative disease that can induce such a malabsorptive syndrome.
The endoscopic findings in EG are variable and few prospective studies have elucidated the breadth of possible findings. Gastric pseudo-polyps have been described in case reports and are likely a high-severity feature of EG, correlating with this patient’s manifestations. However, as normal mucosa or erythema are the most common findings, random biopsies are important in its diagnosis. Pseudo-polyps also prove a clinical challenge in this demographic as polyposis syndromes must be considered. Histopathologic evaluation and region of involvement are important differentiators of EG from polyposis syndromes.
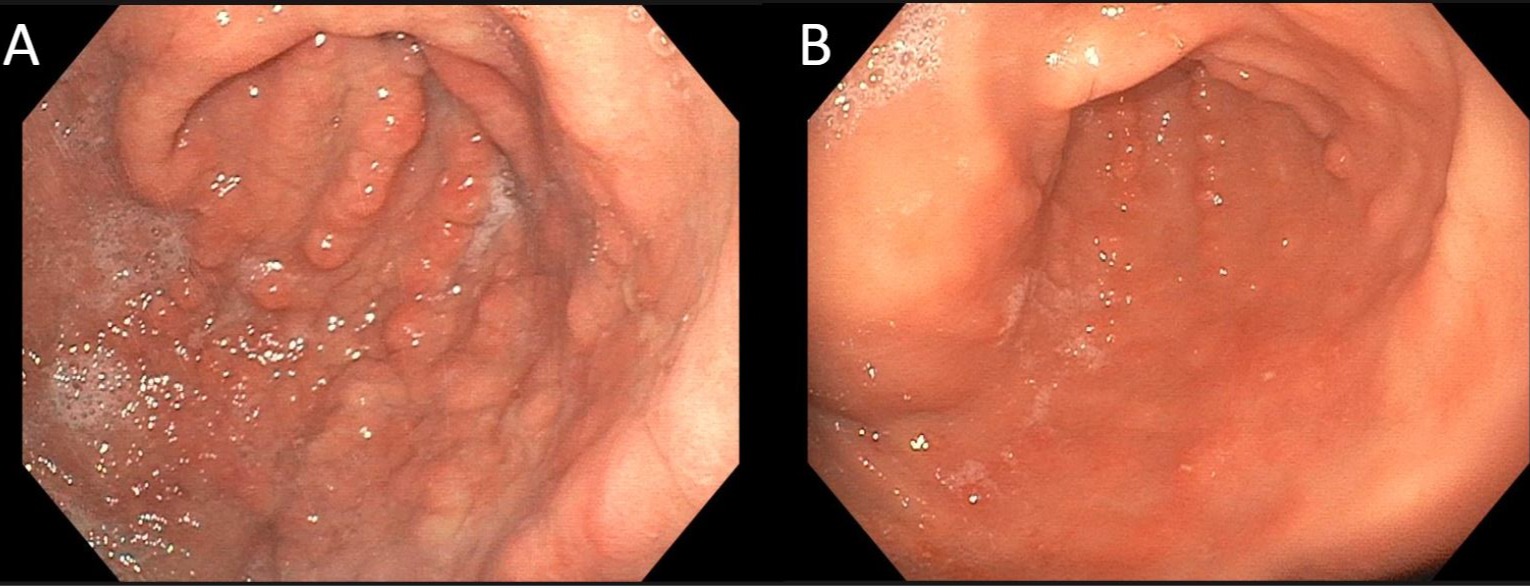
Figure: Figure 1: Gastric antrum before (A) and after (B) treatment.
Disclosures:
Matthew Silverman indicated no relevant financial relationships.
Christopher Casaccio indicated no relevant financial relationships.
Michael Brazeau indicated no relevant financial relationships.
Matthew L. Silverman, MD1, Christopher Casaccio, DO1, Michael Brazeau, DO2. B0722 - Eosinophilic Gastritis With Antral Pseudopolyps, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
