Back

Poster Session A - Sunday Afternoon
Category: Small Intestine
A0645 - Lemmel Syndrome Due to Periampullary Diverticular Food Impaction
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio
- JC
Juan Castano, MD
UTRGV at DHR Gastroenterology Fellowship
Edinburg, TX
Presenting Author(s)
Juan Castano, MD1, Lyla Saeed, MD1, Martha M. Solis, MD2, Asif Zamir, MD, FACG3
1UTRGV at DHR Gastroenterology Fellowship, Edinburg, TX; 2University of Texas Rio Grande Valley, Edinburg, TX; 3University of Texas Rio Grande Valley at Doctors Hospital at Renaissance, Edinburg, TX
Introduction: Lemmel Syndrome is a rare cause of mechanical biliary obstruction attributed to periampullary duodenal diverticula (PAD). It was first described in 1934 as obstructive jaundice in the absence of biliary stones or malignancy. The majority of PAD are asymptomatic, however, about 5% have symptomatic disease. We present a symptomatic case.
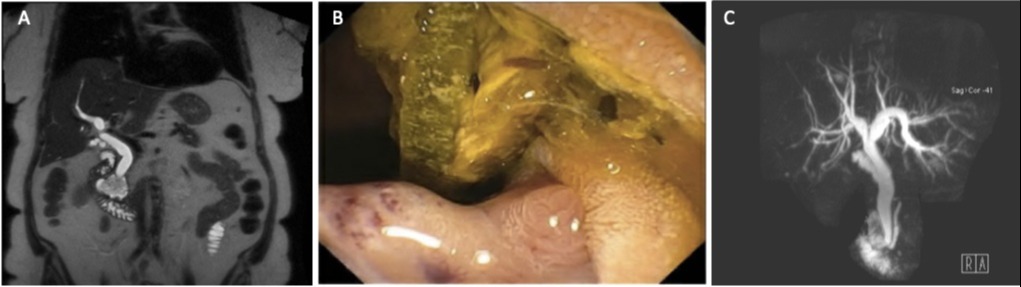
Case Description/Methods: An 80-year-old woman with history of cholecystectomy, coronary artery disease, hypertension, and diabetes was transferred from a free-standing emergency room for acute pancreatitis. She had a one day history of postprandial epigastric pain with radiation to the back. Labs on presentation included lipase above 4000 U/L, BUN 27 mg/dL, AST 316 U/L, ALT 422 U/L, ALP 292 IU/L, total bilirubin 0.6 mg/dL. Abdominal ultrasound revealed 12mm common bile duct (CBD) with intrahepatic ductal dilatation. MRCP showed intra and extrahepatic biliary ductal dilatation with dilated pancreatic duct and a 3.6 cm fluid filled periampullary diverticulum. ERCP showed a large periampullary duodenal diverticulum with food impaction causing obstruction of the ampullary orifice which was removed with forceps. Cholangiogram revealed dilation of pancreatic, common bile, and intrahepatic ducts without any filling defects. Patient improved and was discharged home.
Discussion: The incidence of duodenal diverticula is approximately 17% with PAD being the most common type. PADs are pseudo-diverticula most commonly found in the second part of the duodenum and they pose a cannulation challenge during ERCP with an increased risk of complications. PAD in the setting of biliary obstruction is known as Lemmel Syndrome. It can cause biliary obstruction by sphincter of Oddi dysfunction, direct obstruction, or via external compression by fluid or material-filled PAD. In our case, there was biliary compression due to a food-filled PAD. Cross sectional imaging is critical for diagnosis, however, ERCP is the gold standard. Several therapeutic modalities including endoscopic extraction of entrapped food or stones, extracorporeal shock wave lithotripsy, and laparoscopic diverticulectomy have been used. Our case required endoscopic extraction of diverticular food debris and adds to the limited published cases to date. Lemmel Syndrome requires a high index of suspicion when a PAD is found in the setting of biliary obstruction.
Disclosures:
Juan Castano, MD1, Lyla Saeed, MD1, Martha M. Solis, MD2, Asif Zamir, MD, FACG3. A0645 - Lemmel Syndrome Due to Periampullary Diverticular Food Impaction, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1UTRGV at DHR Gastroenterology Fellowship, Edinburg, TX; 2University of Texas Rio Grande Valley, Edinburg, TX; 3University of Texas Rio Grande Valley at Doctors Hospital at Renaissance, Edinburg, TX
Introduction: Lemmel Syndrome is a rare cause of mechanical biliary obstruction attributed to periampullary duodenal diverticula (PAD). It was first described in 1934 as obstructive jaundice in the absence of biliary stones or malignancy. The majority of PAD are asymptomatic, however, about 5% have symptomatic disease. We present a symptomatic case.
Case Description/Methods: An 80-year-old woman with history of cholecystectomy, coronary artery disease, hypertension, and diabetes was transferred from a free-standing emergency room for acute pancreatitis. She had a one day history of postprandial epigastric pain with radiation to the back. Labs on presentation included lipase above 4000 U/L, BUN 27 mg/dL, AST 316 U/L, ALT 422 U/L, ALP 292 IU/L, total bilirubin 0.6 mg/dL. Abdominal ultrasound revealed 12mm common bile duct (CBD) with intrahepatic ductal dilatation. MRCP showed intra and extrahepatic biliary ductal dilatation with dilated pancreatic duct and a 3.6 cm fluid filled periampullary diverticulum. ERCP showed a large periampullary duodenal diverticulum with food impaction causing obstruction of the ampullary orifice which was removed with forceps. Cholangiogram revealed dilation of pancreatic, common bile, and intrahepatic ducts without any filling defects. Patient improved and was discharged home.
Discussion: The incidence of duodenal diverticula is approximately 17% with PAD being the most common type. PADs are pseudo-diverticula most commonly found in the second part of the duodenum and they pose a cannulation challenge during ERCP with an increased risk of complications. PAD in the setting of biliary obstruction is known as Lemmel Syndrome. It can cause biliary obstruction by sphincter of Oddi dysfunction, direct obstruction, or via external compression by fluid or material-filled PAD. In our case, there was biliary compression due to a food-filled PAD. Cross sectional imaging is critical for diagnosis, however, ERCP is the gold standard. Several therapeutic modalities including endoscopic extraction of entrapped food or stones, extracorporeal shock wave lithotripsy, and laparoscopic diverticulectomy have been used. Our case required endoscopic extraction of diverticular food debris and adds to the limited published cases to date. Lemmel Syndrome requires a high index of suspicion when a PAD is found in the setting of biliary obstruction.
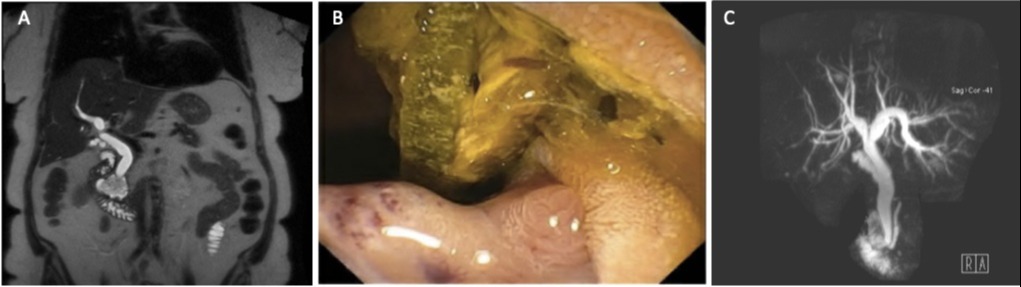
Figure: A. MRCP image showing a large periampullary diverticulum packed with debris.
B. ERCP image of food impacted inside periampullary diverticulum.
C. MRCP image demonstrating a dilated common bile duct in absence of choledocholithiasis.
B. ERCP image of food impacted inside periampullary diverticulum.
C. MRCP image demonstrating a dilated common bile duct in absence of choledocholithiasis.
Disclosures:
Juan Castano indicated no relevant financial relationships.
Lyla Saeed indicated no relevant financial relationships.
Martha Solis indicated no relevant financial relationships.
Asif Zamir indicated no relevant financial relationships.
Juan Castano, MD1, Lyla Saeed, MD1, Martha M. Solis, MD2, Asif Zamir, MD, FACG3. A0645 - Lemmel Syndrome Due to Periampullary Diverticular Food Impaction, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
