Back

Poster Session A - Sunday Afternoon
Category: Interventional Endoscopy
A0438 - Diagnosis and Correction of Afferent Limb Reflux After Single Anastomosis Duodenoileostomy: A Novel Endoscopic Approach
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

William M. LaShomb, MD
San Antonio Uniformed Services Health Education Consortium
San Antonio, TX
Presenting Author(s)
Award: Presidential Poster Award
William M. LaShomb, MD1, Jerome C. Edelson, MD2, Elizabeth L. Carpenter, MD1, Timothy Schaffner, MD1, John G. Quiles, MD1
1San Antonio Uniformed Services Health Education Consortium, San Antonio, TX; 2Brooke Army Medical Center, San Antonio, TX
Introduction: Symptomatic afferent hepatobiliary limb reflux is a rare complication after single-anastomosis duodenoileostomy with sleeve gastrectomy (SADI-S). This condition is clinically distinct from afferent loop syndrome (ALS), and is characterized by retrograde filling of the afferent limb without features of mechanical obstruction. It previously necessitated surgical revision to include creation of a Braun entero-enterostomy (BEE). During surgery, preventative tacks can be placed to minimize afferent limb reflux. Endoscopic diagnosis and treatment are not well described. Here, we report a case of symptomatic afferent limb reflux causing dehydration treated with full thickness endoscopic plication.
Case Description/Methods: A 62-year-old male underwent SADI-S with afferent limb tacking proximal to the pylorus. Two months later, he presented with RUQ pain, nausea, constipation, and poor oral liquid intake necessitating IV fluid hydration. Heavier liquids and solids were tolerated. Due to concern for anastomotic complication, imaging was obtained with UGI series and CT with contrast which were normal. Given high clinical suspicion for limb reflux the patient was referred for upper endoscopy.
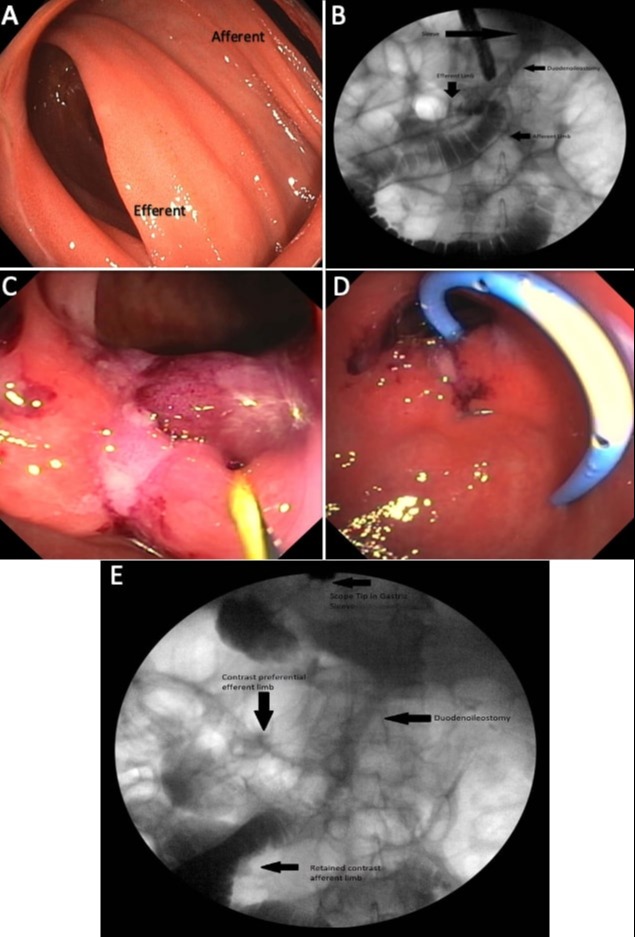
Endoscopy demonstrated a normal esophagus and gastric sleeve anatomy. The biliopancreatic (BP) limb was noted to have acute angulation and contained bile [A]. The scope was then advanced and fluoroscopy confirmed the correct limb. The patient was then placed in Trendelenburg position and contrast was injected into the stomach, demonstrating preferential flow in the BP limb, which confirming afferent limb reflux [B]. Using an endoscopic suturing device, the septum of the anastomosis was sutured to the pylorus, reducing the limb diameter and changing the angle of the anastomosis [C]. To avoid ALS, a double pigtail plastic stent was placed in the BP limb [D]. Final fluoroscopic image demonstrated preferential flow of contrast into the efferent limb [E]. The procedure was tolerated well at follow-up, his oral tolerance had returned to normal with resolution of all symptoms.
Discussion: We present the case of a patient who underwent SADI-S and developed symptomatic afferent hepatobiliary limb reflux despite prophylactic tacking. This was successfully managed with endoscopic suturing, avoiding further surgical intervention. Our case demonstrates a novel use of endoscopic suturing devices and future research is needed to better understand and develop uses of these devices in treating bariatric surgery complications.
Disclosures:
William M. LaShomb, MD1, Jerome C. Edelson, MD2, Elizabeth L. Carpenter, MD1, Timothy Schaffner, MD1, John G. Quiles, MD1. A0438 - Diagnosis and Correction of Afferent Limb Reflux After Single Anastomosis Duodenoileostomy: A Novel Endoscopic Approach, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
William M. LaShomb, MD1, Jerome C. Edelson, MD2, Elizabeth L. Carpenter, MD1, Timothy Schaffner, MD1, John G. Quiles, MD1
1San Antonio Uniformed Services Health Education Consortium, San Antonio, TX; 2Brooke Army Medical Center, San Antonio, TX
Introduction: Symptomatic afferent hepatobiliary limb reflux is a rare complication after single-anastomosis duodenoileostomy with sleeve gastrectomy (SADI-S). This condition is clinically distinct from afferent loop syndrome (ALS), and is characterized by retrograde filling of the afferent limb without features of mechanical obstruction. It previously necessitated surgical revision to include creation of a Braun entero-enterostomy (BEE). During surgery, preventative tacks can be placed to minimize afferent limb reflux. Endoscopic diagnosis and treatment are not well described. Here, we report a case of symptomatic afferent limb reflux causing dehydration treated with full thickness endoscopic plication.
Case Description/Methods: A 62-year-old male underwent SADI-S with afferent limb tacking proximal to the pylorus. Two months later, he presented with RUQ pain, nausea, constipation, and poor oral liquid intake necessitating IV fluid hydration. Heavier liquids and solids were tolerated. Due to concern for anastomotic complication, imaging was obtained with UGI series and CT with contrast which were normal. Given high clinical suspicion for limb reflux the patient was referred for upper endoscopy.
Endoscopy demonstrated a normal esophagus and gastric sleeve anatomy. The biliopancreatic (BP) limb was noted to have acute angulation and contained bile [A]. The scope was then advanced and fluoroscopy confirmed the correct limb. The patient was then placed in Trendelenburg position and contrast was injected into the stomach, demonstrating preferential flow in the BP limb, which confirming afferent limb reflux [B]. Using an endoscopic suturing device, the septum of the anastomosis was sutured to the pylorus, reducing the limb diameter and changing the angle of the anastomosis [C]. To avoid ALS, a double pigtail plastic stent was placed in the BP limb [D]. Final fluoroscopic image demonstrated preferential flow of contrast into the efferent limb [E]. The procedure was tolerated well at follow-up, his oral tolerance had returned to normal with resolution of all symptoms.
Discussion: We present the case of a patient who underwent SADI-S and developed symptomatic afferent hepatobiliary limb reflux despite prophylactic tacking. This was successfully managed with endoscopic suturing, avoiding further surgical intervention. Our case demonstrates a novel use of endoscopic suturing devices and future research is needed to better understand and develop uses of these devices in treating bariatric surgery complications.
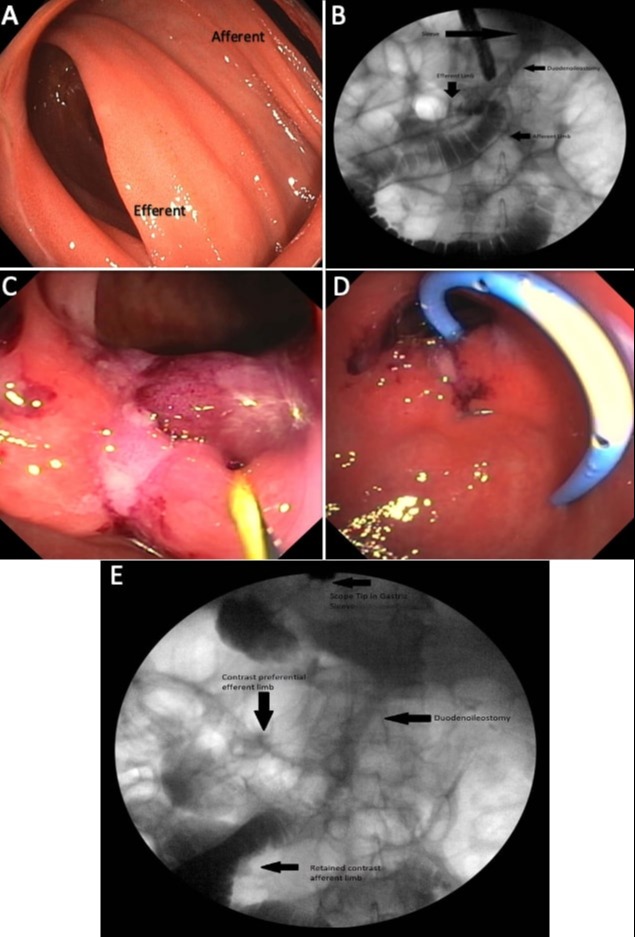
Figure: A. Biliopancreatic (BP) limb
B. Fluoroscopy demonstrating retrograde flow in the BP limb
C. Anastomotic septum after suturing
D. Pigtail placed in the BP limb
E. Preferential flow into the efferent limb after plication
B. Fluoroscopy demonstrating retrograde flow in the BP limb
C. Anastomotic septum after suturing
D. Pigtail placed in the BP limb
E. Preferential flow into the efferent limb after plication
Disclosures:
William LaShomb indicated no relevant financial relationships.
Jerome Edelson indicated no relevant financial relationships.
Elizabeth Carpenter indicated no relevant financial relationships.
Timothy Schaffner indicated no relevant financial relationships.
John Quiles indicated no relevant financial relationships.
William M. LaShomb, MD1, Jerome C. Edelson, MD2, Elizabeth L. Carpenter, MD1, Timothy Schaffner, MD1, John G. Quiles, MD1. A0438 - Diagnosis and Correction of Afferent Limb Reflux After Single Anastomosis Duodenoileostomy: A Novel Endoscopic Approach, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.


