Back

Poster Session C - Monday Afternoon
Category: Biliary/Pancreas
C0082 - Six Years of Evolution With Portal Cavernomatosis and Portal Biliopathy
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom
Has Audio
- JC
Jonnathan Omar Cázares Lara, MD
Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán
Izcalli, Mexico
Presenting Author(s)
Jonnathan Omar Cázares Lara, MD1, Carlos Casian Ruiz Velasco, MD2, Mara Karyme Suaste Luna, MS3, Lilia M. Soberanes-Contreras, MS4, Edgar Granados, MD5, Eduardo Carrillo Maravilla, MD2
1Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Izcalli, Estado de México, Mexico; 2Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico City, Distrito Federal, Mexico; 3Instituto Nacional de Ciencias Médicas y Nutrición “Salvador Zubirán”, Mexico City, Distrito Federal, Mexico; 4Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, México City, Distrito Federal, Mexico; 5INCMNSZ, Ciudad de Mexico, Distrito Federal, Mexico
Introduction: In patients with Portal Biliopathy (PB), It is paramount to engage several branches of gastroenterology to interject the aggressive evolution of this condition.
Case Description/Methods: Our patient is a Man of 45 years old. Medical history of pancreatic divisum, chronic pancreatitis, biliary litho extraction, cholecystectomy, use of endoprosthesis, and pancreatic conduct stenosis.
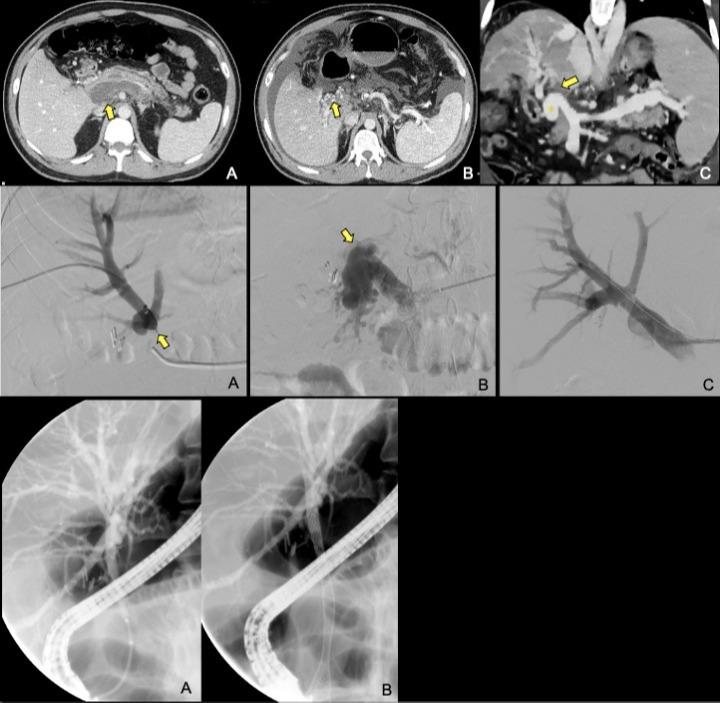
On CT scans in February 2015 he presented a pancreatitis Baltazar E, generating a perfusion defect, and multiple collaterals, in Abril 2015 portal cavernomatosis, and by January 2018 the collateral veins provoked biliary ectasis. During the next 2 years, he presented two events of mild cholangitis.
To solve the choledochal impingement, on October 8, 2019, it took place a portal vein angioplasty with a balloon. The direct extrahepatic portal vein pressure was 30 mmHg pre-plasty, diminishing to 22 mmHg post-plasty.
Posterior to the intervention, he had a new severe healthcare-associated colangitis plus acute pancreatitis, with a 7 mm dilatation only in the intrahepatic biliary pathway. To improve the biliary stasis, by CPRE it was placed a metallic stent covered with a Wallflex 10 mm x 8 cm.
By February 2020, a CT scan still showed a permeable porta in the confluence, yet the portal prosthesis was not visible.
Finally in September 2021, without clinic traits of portal hypertension, events of cholestasis, and improvement in hepatic function
Discussion: In the biliary tract, venous drainage passes through two venous plexus named, the epicholedochal venous plexus of Saint and the paracholedochal venous plexus of Petren. In portal biliopathy, changes are a result of dilatation of veins of the plexus of Saint, causing bile duct impingement. It has been hypothesized that this lead to fibrous scarring of porta hepatis, and ischemic injury to the bile ducts resulting in stricture formation and caliber irregularity with upstream dilatation.
Several studies have shown that bile duct changes occur in 81–100% of patients with extrahepatic portal vein obstruction, but only 5–30% of patients present symptoms of biliary obstruction.
In adults conditions such as thrombophilia, intra-abdominal infection, malignancy, myeloproliferative disorders and cirrhosis have been implicated
PB is mainly a feature of extrahepatic portal venous obstruction, patients presenting with symptoms require an integrated management addressing biliary obstruction and portal hypertension in tandem. However, the relief of both conditions is only temporary.
Disclosures:
Jonnathan Omar Cázares Lara, MD1, Carlos Casian Ruiz Velasco, MD2, Mara Karyme Suaste Luna, MS3, Lilia M. Soberanes-Contreras, MS4, Edgar Granados, MD5, Eduardo Carrillo Maravilla, MD2. C0082 - Six Years of Evolution With Portal Cavernomatosis and Portal Biliopathy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Izcalli, Estado de México, Mexico; 2Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, Mexico City, Distrito Federal, Mexico; 3Instituto Nacional de Ciencias Médicas y Nutrición “Salvador Zubirán”, Mexico City, Distrito Federal, Mexico; 4Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, México City, Distrito Federal, Mexico; 5INCMNSZ, Ciudad de Mexico, Distrito Federal, Mexico
Introduction: In patients with Portal Biliopathy (PB), It is paramount to engage several branches of gastroenterology to interject the aggressive evolution of this condition.
Case Description/Methods: Our patient is a Man of 45 years old. Medical history of pancreatic divisum, chronic pancreatitis, biliary litho extraction, cholecystectomy, use of endoprosthesis, and pancreatic conduct stenosis.
On CT scans in February 2015 he presented a pancreatitis Baltazar E, generating a perfusion defect, and multiple collaterals, in Abril 2015 portal cavernomatosis, and by January 2018 the collateral veins provoked biliary ectasis. During the next 2 years, he presented two events of mild cholangitis.
To solve the choledochal impingement, on October 8, 2019, it took place a portal vein angioplasty with a balloon. The direct extrahepatic portal vein pressure was 30 mmHg pre-plasty, diminishing to 22 mmHg post-plasty.
Posterior to the intervention, he had a new severe healthcare-associated colangitis plus acute pancreatitis, with a 7 mm dilatation only in the intrahepatic biliary pathway. To improve the biliary stasis, by CPRE it was placed a metallic stent covered with a Wallflex 10 mm x 8 cm.
By February 2020, a CT scan still showed a permeable porta in the confluence, yet the portal prosthesis was not visible.
Finally in September 2021, without clinic traits of portal hypertension, events of cholestasis, and improvement in hepatic function
Discussion: In the biliary tract, venous drainage passes through two venous plexus named, the epicholedochal venous plexus of Saint and the paracholedochal venous plexus of Petren. In portal biliopathy, changes are a result of dilatation of veins of the plexus of Saint, causing bile duct impingement. It has been hypothesized that this lead to fibrous scarring of porta hepatis, and ischemic injury to the bile ducts resulting in stricture formation and caliber irregularity with upstream dilatation.
Several studies have shown that bile duct changes occur in 81–100% of patients with extrahepatic portal vein obstruction, but only 5–30% of patients present symptoms of biliary obstruction.
In adults conditions such as thrombophilia, intra-abdominal infection, malignancy, myeloproliferative disorders and cirrhosis have been implicated
PB is mainly a feature of extrahepatic portal venous obstruction, patients presenting with symptoms require an integrated management addressing biliary obstruction and portal hypertension in tandem. However, the relief of both conditions is only temporary.
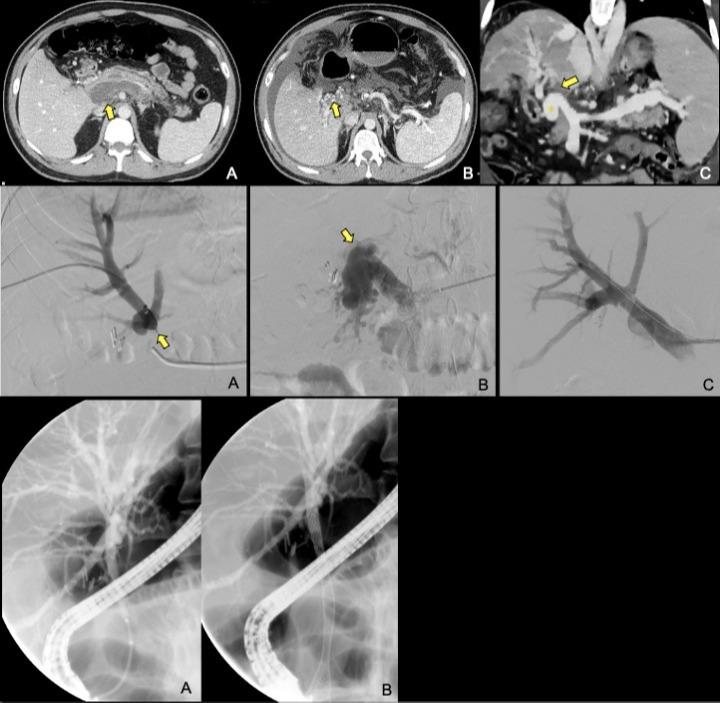
Figure: Figure 1. Initial axial CT scan following the known event of acute pancreatitis, showing acute splenic-portal venous thrombosis demonstrated by unenhanced and distended portal vein (yellow arrow in a). The middle image three months later shows the formation of small collateral vessels in the hepatic hilium, (yellow arrow in b), and also notes new-onset ascites due to impaired liver function. Coronal reformat image two years later, points to the focal area of chronic portal thrombosis, yellow arrow in (c) with more prominent appearance collateral vessels “cavernomatosis” (asterisk), several perfusion defects in the liver parenchyma, and marked splenomegaly.
Figure 2. DSA images, in (a) transhepatic percutaneous venography with opacification of intrahepatic portal vasculature with a sudden interruption in the site of thrombosis (yellow arrow in a). (b) splenic approach with opacification of the extrahepatic portal vein and aneurismatic collateral vessels due to cavernomatosis and upstream thrombotic interruption (yellow arrow in b). (c) final imagen after portal vein angioplasty demonstrates adequate and complete opacification of the portal vein and its branches.
Figure 3. ERCP in (a) shows intrahepatic bile duct dilatation and impingement and (b) after stent placement with diminished dilatation
Figure 2. DSA images, in (a) transhepatic percutaneous venography with opacification of intrahepatic portal vasculature with a sudden interruption in the site of thrombosis (yellow arrow in a). (b) splenic approach with opacification of the extrahepatic portal vein and aneurismatic collateral vessels due to cavernomatosis and upstream thrombotic interruption (yellow arrow in b). (c) final imagen after portal vein angioplasty demonstrates adequate and complete opacification of the portal vein and its branches.
Figure 3. ERCP in (a) shows intrahepatic bile duct dilatation and impingement and (b) after stent placement with diminished dilatation
Disclosures:
Jonnathan Omar Cázares Lara indicated no relevant financial relationships.
Carlos Casian Ruiz Velasco indicated no relevant financial relationships.
Mara Karyme Suaste Luna indicated no relevant financial relationships.
Lilia Soberanes-Contreras indicated no relevant financial relationships.
Edgar Granados indicated no relevant financial relationships.
Eduardo Carrillo Maravilla indicated no relevant financial relationships.
Jonnathan Omar Cázares Lara, MD1, Carlos Casian Ruiz Velasco, MD2, Mara Karyme Suaste Luna, MS3, Lilia M. Soberanes-Contreras, MS4, Edgar Granados, MD5, Eduardo Carrillo Maravilla, MD2. C0082 - Six Years of Evolution With Portal Cavernomatosis and Portal Biliopathy, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

