Back

Poster Session D - Tuesday Morning
Category: Biliary/Pancreas
D0074 - An Uncommon Case of Smoldering Pancreatitis
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Kevin Kadado, DO
University of Kansas
Wichita, KS
Presenting Author(s)
Kevin Kadado, DO1, Winnie Sheu Woc, MD2, Ali Ahmad, MD3, Phu V. Truong, MD4, Bassem Matta, MD2
1University of Kansas, Wichita, KS; 2Kansas Gastroenterology, Wichita, KS; 3Wichita Surgical Specialists, Wichita, KS; 4Cancer Center of Kansas, Wichita, KS
Introduction: We describe a rapid onset, poorly differentiated, invasive pancreatic carcinoma with histiocytoid features diagnosed post-pancreaticoduodenectomy, after endoscopic ultrasound (EUS) guided fine needle biopsy failed to identify it.
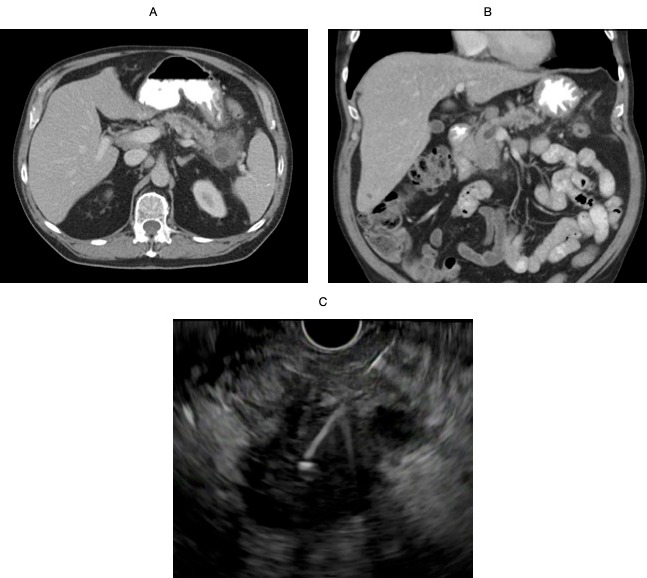
Case Description/Methods: A 69-year-old male with a history of alcohol abuse, and tobacco use, initially presented with epigastric pain and early satiety, diagnosed with acute pancreatitis. Computed tomography (CT) scan and Magnetic resonance imaging (MRI) of the abdomen/pelvis at this time were significant for a cystic lesion in the tail of the pancreas with fat stranding (figure A). EUS was performed however had extremely limited visibility given inflammatory changes, main pancreatic ductal dilation was noted but no clear mass was identified. Fine needle aspiration (FNA) of the cystic structure was suggestive of a pseudocyst on cytology (CEA 25 ng/ml, amylase 3250 units/L). A portal lymph node was appreciated, and fine needle biopsies (FNBx) yielded only inflammatory cells. Clinical course continued to deteriorate over the next few months with non-resolving smoldering pancreatitis symptoms and >80 lb weight loss. Repeat CT abdomen/pelvis was significant for a 2.7 x 2.1 cm lesion of the head of the pancreas (figure B). EUS was repeated and revealed a 32 x 29 mm hypoechoic mass in the head of the pancreas with upstream pancreatic ductal dilation to 13 mm with significant parenchymal atrophy as well as an enlarged porta hepatis lymph node. FNBx were obtained and were sent for analysis at a tertiary care center which revealed chronic inflammation with necrohistiocystic debris with atypical cells at both sites (figure C). Due to clinical deterioration and after multidisciplinary discussion, patient underwent a pancreaticoduodenectomy for smoldering pancreatitis involving the head of pancreas and concerning atypical cells. The final pathology report revealed a poorly differentiated, invasive pancreatic carcinoma with histiocytoid features that extensively involved 6/16 regional lymph nodes after multiple reviews by multiple pathologists.
Discussion: To our knowledge, poorly differentiated, invasive pancreatic carcinoma with histiocytoid features has not been previously documented. This presentation with smoldering pancreatitis significantly delayed the diagnosis due to the marked inflammatory changes compromising initial imaging (CT, MRI, EUS). This case highlights the importance of a multidisciplinary approach in managing complicated non resolving pancreatitis cases.
Disclosures:
Kevin Kadado, DO1, Winnie Sheu Woc, MD2, Ali Ahmad, MD3, Phu V. Truong, MD4, Bassem Matta, MD2. D0074 - An Uncommon Case of Smoldering Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Kansas, Wichita, KS; 2Kansas Gastroenterology, Wichita, KS; 3Wichita Surgical Specialists, Wichita, KS; 4Cancer Center of Kansas, Wichita, KS
Introduction: We describe a rapid onset, poorly differentiated, invasive pancreatic carcinoma with histiocytoid features diagnosed post-pancreaticoduodenectomy, after endoscopic ultrasound (EUS) guided fine needle biopsy failed to identify it.
Case Description/Methods: A 69-year-old male with a history of alcohol abuse, and tobacco use, initially presented with epigastric pain and early satiety, diagnosed with acute pancreatitis. Computed tomography (CT) scan and Magnetic resonance imaging (MRI) of the abdomen/pelvis at this time were significant for a cystic lesion in the tail of the pancreas with fat stranding (figure A). EUS was performed however had extremely limited visibility given inflammatory changes, main pancreatic ductal dilation was noted but no clear mass was identified. Fine needle aspiration (FNA) of the cystic structure was suggestive of a pseudocyst on cytology (CEA 25 ng/ml, amylase 3250 units/L). A portal lymph node was appreciated, and fine needle biopsies (FNBx) yielded only inflammatory cells. Clinical course continued to deteriorate over the next few months with non-resolving smoldering pancreatitis symptoms and >80 lb weight loss. Repeat CT abdomen/pelvis was significant for a 2.7 x 2.1 cm lesion of the head of the pancreas (figure B). EUS was repeated and revealed a 32 x 29 mm hypoechoic mass in the head of the pancreas with upstream pancreatic ductal dilation to 13 mm with significant parenchymal atrophy as well as an enlarged porta hepatis lymph node. FNBx were obtained and were sent for analysis at a tertiary care center which revealed chronic inflammation with necrohistiocystic debris with atypical cells at both sites (figure C). Due to clinical deterioration and after multidisciplinary discussion, patient underwent a pancreaticoduodenectomy for smoldering pancreatitis involving the head of pancreas and concerning atypical cells. The final pathology report revealed a poorly differentiated, invasive pancreatic carcinoma with histiocytoid features that extensively involved 6/16 regional lymph nodes after multiple reviews by multiple pathologists.
Discussion: To our knowledge, poorly differentiated, invasive pancreatic carcinoma with histiocytoid features has not been previously documented. This presentation with smoldering pancreatitis significantly delayed the diagnosis due to the marked inflammatory changes compromising initial imaging (CT, MRI, EUS). This case highlights the importance of a multidisciplinary approach in managing complicated non resolving pancreatitis cases.
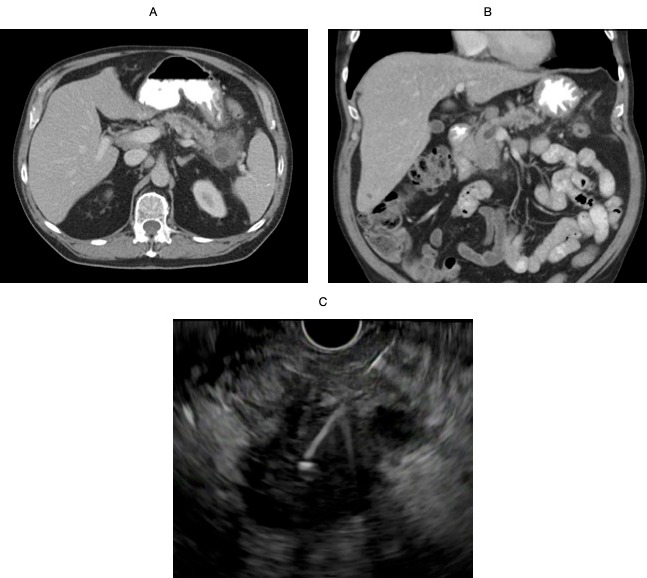
Figure: Figure A - Cystic lesion with inflammatory changes near the tail of the pancreas; Figure B - Mass in the head of the pancreas with upstream pancreatic duct dilation; Figure C - Endoscopic Ultrasound with fine needle biopsy of the mass in the head of pancreas
Disclosures:
Kevin Kadado indicated no relevant financial relationships.
Winnie Sheu Woc indicated no relevant financial relationships.
Ali Ahmad indicated no relevant financial relationships.
Phu Truong indicated no relevant financial relationships.
Bassem Matta indicated no relevant financial relationships.
Kevin Kadado, DO1, Winnie Sheu Woc, MD2, Ali Ahmad, MD3, Phu V. Truong, MD4, Bassem Matta, MD2. D0074 - An Uncommon Case of Smoldering Pancreatitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
