Back

Poster Session D - Tuesday Morning
Category: Colon
D0145 - A Case of Abdominal Cocooning From Appendiceal Carcinomatosis
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Zalak Shah, MD
Carolinas Medical Center
Charlotte, NC
Presenting Author(s)
Zalak Shah, MD, Anika Noorali, MD, Jonathan Gee, MD
Carolinas Medical Center, Charlotte, NC
Introduction: Abdominal cocooning is a rare radiologic finding where thickened peritoneal membrane surrounds the intestines causing bowel to become trapped and adhered to each other. This is usually a result of chronic inflammation and can be associated with infections like tuberculosis (TB) or chronic processes like sarcoidosis, peritoneal dialysis, VP shunts, or carcinomatosis. Patients typically present with intractable nausea, vomiting, abdominal pain and distension. Here, we present a case of abdominal cocooning with recurrent ascites secondary to appendiceal carcinomatosis.
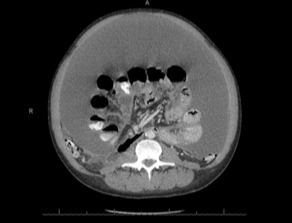
Case Description/Methods: 41-year-old male with history of remote polysubstance use (IV and alcohol) and incarceration who presented to the ED with progressively worsening abdominal distension and intractable nonbloody, nonbilious emesis. This patient had been hospitalized for a similar presentation weeks prior. At that time, he was found to have large volume ascites (SAAG 1.1, 774 nucleated cells, 3% segs) and was diagnosed with alcoholic cirrhosis though RUQ ultrasound with liver doppler and lab work were normal. CT abdomen and pelvis showed “peritoneal thickening concerning for peritonitis” (Figure 1) and the patient was treated for presumed spontaneous bacterial peritonitis. He presented to our facility weeks later with recurrent ascites (SAAG 1.2, 795 nucleated cells, 1% segs). Triphasic liver CT showed findings that were “highly suspicious for encapsulating peritoneal sclerosis/abdominal cocoon”. Ultimately, a peritoneal biopsy was performed given concerns for carcinomatosis vs. TB infection. Final pathology showed goblet cell adenocarcinoma with presumed appendiceal origin. Colonoscopy was unsuccessful due to cementing of the peritoneum. Patient was not a candidate for chemotherapy due to having severe malnutrition requiring the initiation of total parenteral nutrition. He was discharged with outpatient GI oncology follow up.
Discussion: Although cirrhotic ascites is commonly diagnosed and treated by physicians, it is vital that clinicians are also aware of the diagnostic findings of noncirrhotic ascites. In this case, the degree of WBC count elevation with low segmented cells likely indicated TB or carcinomatosis at the initial presentation. Familiarity with imaging findings of abdominal cocooning may have also contributed to an expedited diagnosis. This case reiterates the importance of questioning and further exploring symptom etiologies when routine workup is not consistent with common causes of an everyday complaint.
Disclosures:
Zalak Shah, MD, Anika Noorali, MD, Jonathan Gee, MD. D0145 - A Case of Abdominal Cocooning From Appendiceal Carcinomatosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Carolinas Medical Center, Charlotte, NC
Introduction: Abdominal cocooning is a rare radiologic finding where thickened peritoneal membrane surrounds the intestines causing bowel to become trapped and adhered to each other. This is usually a result of chronic inflammation and can be associated with infections like tuberculosis (TB) or chronic processes like sarcoidosis, peritoneal dialysis, VP shunts, or carcinomatosis. Patients typically present with intractable nausea, vomiting, abdominal pain and distension. Here, we present a case of abdominal cocooning with recurrent ascites secondary to appendiceal carcinomatosis.
Case Description/Methods: 41-year-old male with history of remote polysubstance use (IV and alcohol) and incarceration who presented to the ED with progressively worsening abdominal distension and intractable nonbloody, nonbilious emesis. This patient had been hospitalized for a similar presentation weeks prior. At that time, he was found to have large volume ascites (SAAG 1.1, 774 nucleated cells, 3% segs) and was diagnosed with alcoholic cirrhosis though RUQ ultrasound with liver doppler and lab work were normal. CT abdomen and pelvis showed “peritoneal thickening concerning for peritonitis” (Figure 1) and the patient was treated for presumed spontaneous bacterial peritonitis. He presented to our facility weeks later with recurrent ascites (SAAG 1.2, 795 nucleated cells, 1% segs). Triphasic liver CT showed findings that were “highly suspicious for encapsulating peritoneal sclerosis/abdominal cocoon”. Ultimately, a peritoneal biopsy was performed given concerns for carcinomatosis vs. TB infection. Final pathology showed goblet cell adenocarcinoma with presumed appendiceal origin. Colonoscopy was unsuccessful due to cementing of the peritoneum. Patient was not a candidate for chemotherapy due to having severe malnutrition requiring the initiation of total parenteral nutrition. He was discharged with outpatient GI oncology follow up.
Discussion: Although cirrhotic ascites is commonly diagnosed and treated by physicians, it is vital that clinicians are also aware of the diagnostic findings of noncirrhotic ascites. In this case, the degree of WBC count elevation with low segmented cells likely indicated TB or carcinomatosis at the initial presentation. Familiarity with imaging findings of abdominal cocooning may have also contributed to an expedited diagnosis. This case reiterates the importance of questioning and further exploring symptom etiologies when routine workup is not consistent with common causes of an everyday complaint.
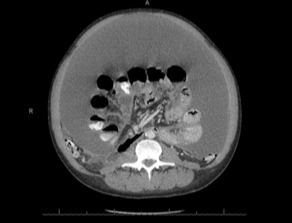
Figure: Figure 1: Peritoneal thickening consistent with abdominal cocooning with large-volume ascites
Disclosures:
Zalak Shah indicated no relevant financial relationships.
Anika Noorali indicated no relevant financial relationships.
Jonathan Gee indicated no relevant financial relationships.
Zalak Shah, MD, Anika Noorali, MD, Jonathan Gee, MD. D0145 - A Case of Abdominal Cocooning From Appendiceal Carcinomatosis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
