Back

Poster Session B - Monday Morning
Category: Esophagus
B0238 - Black Esophagus Manifesting as Upper Gastrointestinal Bleeding in Diabetic Ketoacidosis: A Case Report
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Fouad S. Jaber, MD
University of Missouri-Kansas City
KANSAS CITY, MO
Presenting Author(s)
Fouad S. Jaber, MD1, Rawan Rajab, MD1, Islam Mohamed, MD1, Noor Hassan, MD2, Kimberly Sanders, MD2
1University of Missouri-Kansas City, Kansas City, MO; 2University of Missouri Kansas City School of Medicine, Kansas City, MO
Introduction: Acute esophageal necrosis, or black esophagus, is a rare clinical entity manifesting as upper gastrointestinal bleeding and complicating various conditions. However, black esophagus in the setting of diabetic ketoacidosis (DKA) has been rarely reported. We present a case of a 36-year-old male with black esophagus presenting as hematemesis complicating an episode of DKA.
Case Description/Methods: A 36-year-old male with uncontrolled type 1 diabetes mellitus complicated by end-stage renal disease and hypertension presented to the emergency department with abdominal pain, nausea, and vomiting. Patient reported worsening abdominal pain and associated blood-tinged emesis. On presentation, patient was hemodynamically stable. Physical exam included an abdomen that was diffusely tender to palpation without peritoneal signs. Initial labs remarkable for serum glucose 1491, anion gap 41, bicarbonate 9, and hemoglobin 7.5.
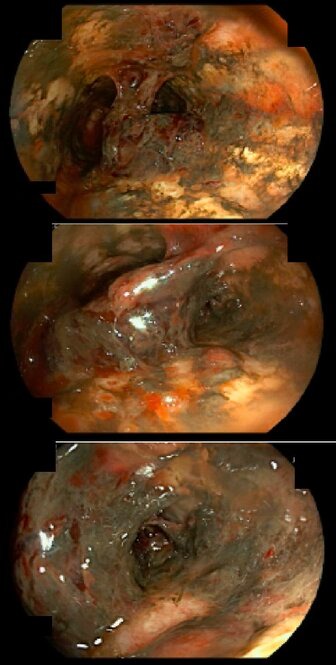
Patient was admitted to Critical Care for insulin drip and intravenous fluid resuscitation for DKA. Later, patient had an episode of hematemesis resulting in tachycardia, hypotension, and drop in hemoglobin to 5.6. Patient was further resuscitated with blood transfusions with improvement in hemodynamics and hemoglobin to 8.9. Continuous pantoprazole infusion was initiated. Upper endoscopy demonstrated severe, ulcerative necrotizing circumferential esophagitis in the middle and lower third esophagus and a medium size blood clot without evidence of active bleeding. No biopsies were taken due to concern for possible false lumen; CT chest with contrast demonstrated no signs of esophageal perforation. Following EGD, patient had several small self-limiting episodes of hematemesis and melena, while maintaining hemodynamics. He was continued on pantoprazole infusion and placed on strict nothing by mouth (NPO) precautions for 3 days with gradual advancement of diet. He received 6 days of empiric antimicrobial therapy with ampicillin-sulbactam and fluconazole. Patient reported no further episodes of hematemesis. Hemoglobin stabilized around 8.0.
Discussion: DKA is a rare but life-threatening cause of acute esophageal necrosis which may develop due to a combination of tissue hypoperfusion, impaired mucosal defenses, and gastric reflux. Upper gastrointestinal bleeding in the setting of DKA should raise suspicion for black esophagus which is a potential cause of mortality. Early diagnosis and treatment of underlying etiology are the key factors in management.
Disclosures:
Fouad S. Jaber, MD1, Rawan Rajab, MD1, Islam Mohamed, MD1, Noor Hassan, MD2, Kimberly Sanders, MD2. B0238 - Black Esophagus Manifesting as Upper Gastrointestinal Bleeding in Diabetic Ketoacidosis: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Missouri-Kansas City, Kansas City, MO; 2University of Missouri Kansas City School of Medicine, Kansas City, MO
Introduction: Acute esophageal necrosis, or black esophagus, is a rare clinical entity manifesting as upper gastrointestinal bleeding and complicating various conditions. However, black esophagus in the setting of diabetic ketoacidosis (DKA) has been rarely reported. We present a case of a 36-year-old male with black esophagus presenting as hematemesis complicating an episode of DKA.
Case Description/Methods: A 36-year-old male with uncontrolled type 1 diabetes mellitus complicated by end-stage renal disease and hypertension presented to the emergency department with abdominal pain, nausea, and vomiting. Patient reported worsening abdominal pain and associated blood-tinged emesis. On presentation, patient was hemodynamically stable. Physical exam included an abdomen that was diffusely tender to palpation without peritoneal signs. Initial labs remarkable for serum glucose 1491, anion gap 41, bicarbonate 9, and hemoglobin 7.5.
Patient was admitted to Critical Care for insulin drip and intravenous fluid resuscitation for DKA. Later, patient had an episode of hematemesis resulting in tachycardia, hypotension, and drop in hemoglobin to 5.6. Patient was further resuscitated with blood transfusions with improvement in hemodynamics and hemoglobin to 8.9. Continuous pantoprazole infusion was initiated. Upper endoscopy demonstrated severe, ulcerative necrotizing circumferential esophagitis in the middle and lower third esophagus and a medium size blood clot without evidence of active bleeding. No biopsies were taken due to concern for possible false lumen; CT chest with contrast demonstrated no signs of esophageal perforation. Following EGD, patient had several small self-limiting episodes of hematemesis and melena, while maintaining hemodynamics. He was continued on pantoprazole infusion and placed on strict nothing by mouth (NPO) precautions for 3 days with gradual advancement of diet. He received 6 days of empiric antimicrobial therapy with ampicillin-sulbactam and fluconazole. Patient reported no further episodes of hematemesis. Hemoglobin stabilized around 8.0.
Discussion: DKA is a rare but life-threatening cause of acute esophageal necrosis which may develop due to a combination of tissue hypoperfusion, impaired mucosal defenses, and gastric reflux. Upper gastrointestinal bleeding in the setting of DKA should raise suspicion for black esophagus which is a potential cause of mortality. Early diagnosis and treatment of underlying etiology are the key factors in management.
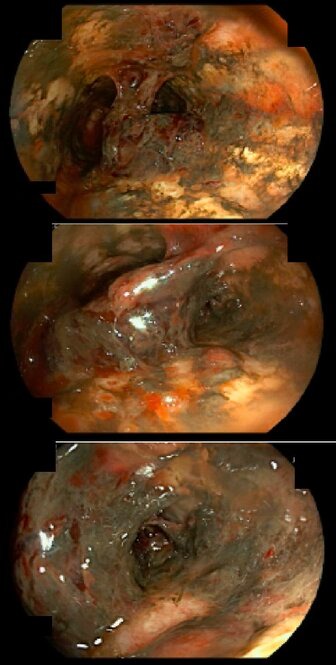
Figure: Figure 1: severe, ulcerative necrotizing circumferential esophagitis in the middle and lower third esophagus and a medium size blood clot without evidence of active bleeding
Disclosures:
Fouad Jaber indicated no relevant financial relationships.
Rawan Rajab indicated no relevant financial relationships.
Islam Mohamed indicated no relevant financial relationships.
Noor Hassan indicated no relevant financial relationships.
Kimberly Sanders indicated no relevant financial relationships.
Fouad S. Jaber, MD1, Rawan Rajab, MD1, Islam Mohamed, MD1, Noor Hassan, MD2, Kimberly Sanders, MD2. B0238 - Black Esophagus Manifesting as Upper Gastrointestinal Bleeding in Diabetic Ketoacidosis: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
