Back

Poster Session B - Monday Morning
Category: Stomach
B0729 - Successful Endoscopic Pyloric Therapy in a Patient With Gastroparesis and Normal 3 Cpm Gastric Myoelectrical Activity After Failed Surgeries for Superior Mesentery Artery Syndrome and Median Arcuate Ligament Syndrome
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Fadi Chanaa, MD
Atrium Health Wake Forest Baptist Medical Center
Winston-Salem, North Carolina
Presenting Author(s)
Fadi Chanaa, MD1, Kenneth Koch, MD2
1Atrium Health Wake Forest Baptist Medical Center, Winston-Salem, NC; 2Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: Patients with chronic nausea and vomiting and gastroparesis (GP) may undergo empiric and often unnecessary surgical procedures in attempts to control symptoms. This case demonstrates the successful diagnosis and endoscopic management of pyloric neuromuscular dysfunction in a patient GP and refractory nausea and vomiting.
Case Description/Methods: AL is a 21 year old female with history of POTS, Ehlers Danlos, Superior Mesenteric Artery Syndrome (SMAS), Median Arcuate Ligament Syndrome (MALS), IBS-C, and GP presented initially with nausea, vomiting, early satiety, and post-prandial pain. Patient failed trials of anti-spasmodic and prokinetic medications. She also underwent cholecystectomy, duodenojejunostomy for SMAS, and median arcuate ligament release for MALS with minimal relief of symptoms. She underwent multiple dilations of her duodenojejunal anastomosis without improvement of symptoms. During this time, she lost 35 pounds, failed enteral nutrition, and required IV fluids and total parental nutrition.
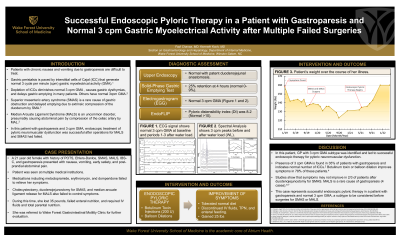
She was referred to the GI motility clinic for further evaluation. An EGD was normal with patent duodenojejunal anastomosis. A 4 hour solid-phase gastric emptying test revealed 25% retention at 4 hours (normal 0-9%). An electrogastrogram (EGG) with water load satiety test showed normal 3 cpm Gastric Myoelectrical Activity (GMA) after she ingested 125 ml of water (normal > 240 ml). Pyloric distensibility index (DI) was 8.2 (Normal >10). Botulinum toxin A was injected into each quadrant of the pylorus. Over the next 7 months, she had multiple botulinum injections and pyloric balloon dilations. Symptoms improved and she began eating food which led to a 25 lb weight gain. IV fluids and tube feedings were stopped.
Discussion: The diagnosis of GP is established after mechanical obstruction of the stomach is excluded. Previous studies have questioned whether surgical correction of SMAS improves symptoms in GP. A proportion of these patients also undergo correction of MALS to decrease abdominal pain potentially related to celiac artery compression from the median arcuate ligament. EGG was used in AL to subtype GP into dysrhythmic or normal 3 cpm GMA. GP with normal 3 cpm GMA is associated with pyloric stenosis and/or pyloric neuromuscular dysfunction. In this case, GP with 3 cpm GMA subtype was the cause of symptoms, not SMAS or MALS, and responded well to endoscopic pyloric therapies.

Disclosures:
Fadi Chanaa, MD1, Kenneth Koch, MD2. B0729 - Successful Endoscopic Pyloric Therapy in a Patient With Gastroparesis and Normal 3 Cpm Gastric Myoelectrical Activity After Failed Surgeries for Superior Mesentery Artery Syndrome and Median Arcuate Ligament Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Atrium Health Wake Forest Baptist Medical Center, Winston-Salem, NC; 2Wake Forest University School of Medicine, Winston-Salem, NC
Introduction: Patients with chronic nausea and vomiting and gastroparesis (GP) may undergo empiric and often unnecessary surgical procedures in attempts to control symptoms. This case demonstrates the successful diagnosis and endoscopic management of pyloric neuromuscular dysfunction in a patient GP and refractory nausea and vomiting.
Case Description/Methods: AL is a 21 year old female with history of POTS, Ehlers Danlos, Superior Mesenteric Artery Syndrome (SMAS), Median Arcuate Ligament Syndrome (MALS), IBS-C, and GP presented initially with nausea, vomiting, early satiety, and post-prandial pain. Patient failed trials of anti-spasmodic and prokinetic medications. She also underwent cholecystectomy, duodenojejunostomy for SMAS, and median arcuate ligament release for MALS with minimal relief of symptoms. She underwent multiple dilations of her duodenojejunal anastomosis without improvement of symptoms. During this time, she lost 35 pounds, failed enteral nutrition, and required IV fluids and total parental nutrition.
She was referred to the GI motility clinic for further evaluation. An EGD was normal with patent duodenojejunal anastomosis. A 4 hour solid-phase gastric emptying test revealed 25% retention at 4 hours (normal 0-9%). An electrogastrogram (EGG) with water load satiety test showed normal 3 cpm Gastric Myoelectrical Activity (GMA) after she ingested 125 ml of water (normal > 240 ml). Pyloric distensibility index (DI) was 8.2 (Normal >10). Botulinum toxin A was injected into each quadrant of the pylorus. Over the next 7 months, she had multiple botulinum injections and pyloric balloon dilations. Symptoms improved and she began eating food which led to a 25 lb weight gain. IV fluids and tube feedings were stopped.
Discussion: The diagnosis of GP is established after mechanical obstruction of the stomach is excluded. Previous studies have questioned whether surgical correction of SMAS improves symptoms in GP. A proportion of these patients also undergo correction of MALS to decrease abdominal pain potentially related to celiac artery compression from the median arcuate ligament. EGG was used in AL to subtype GP into dysrhythmic or normal 3 cpm GMA. GP with normal 3 cpm GMA is associated with pyloric stenosis and/or pyloric neuromuscular dysfunction. In this case, GP with 3 cpm GMA subtype was the cause of symptoms, not SMAS or MALS, and responded well to endoscopic pyloric therapies.

Figure: (A) EGG recordings of GMA showing 3 cpm waves at baseline and during Periods 1-3 after the WL. (B) Spectral analysis of EGG recording of GMA showing strong 3 cpm peaks before and after the water load satiety test (WL). (C) Graph displaying patient’s weight and procedures over time. She continued to lose weight after SMA and MALS operations but returned to baseline weight after starting endoscopic pyloric botulinum injections and dilations.
Disclosures:
Fadi Chanaa indicated no relevant financial relationships.
Kenneth Koch indicated no relevant financial relationships.
Fadi Chanaa, MD1, Kenneth Koch, MD2. B0729 - Successful Endoscopic Pyloric Therapy in a Patient With Gastroparesis and Normal 3 Cpm Gastric Myoelectrical Activity After Failed Surgeries for Superior Mesentery Artery Syndrome and Median Arcuate Ligament Syndrome, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
