Back

Poster Session A - Sunday Afternoon
Category: GI Bleeding
A0319 - Does Size Matter? A Case Series on Management of Duodenal Varices
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom
Has Audio

Danyal O. Imam, MBBS
Riverside University Health System
Moreno Valley, CA
Presenting Author(s)
Danyal O. Imam, MBBS1, Beenish Naqvi, MBBS1, Joy Lee, MD2, Steve Serrao, MD1, Christopher Bent, MD1, Pejman Solaimani, MD1
1Riverside University Health System, Moreno Valley, CA; 2Loma Linda University Medical Center, Loma Linda, CA
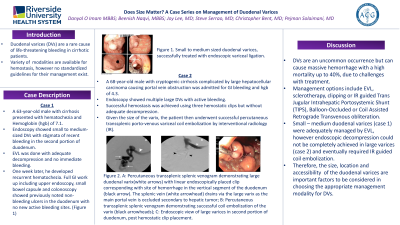
Introduction: Duodenal varices (DVs) are a rare cause of life-threatening bleeding in cirrhotic patients. No standardized guidelines for their management exist. We present two cases of DV hemorrhage who were successfully managed by endoscopic variceal band ligation (EVL) and coil embolization respectively.
Case Description/Methods: Case 1: A 63-year-old male with cirrhosis was admitted for upper GI bleeding and Hemoglobin (hgb) of 7.1. Endoscopy showed small to medium-sized DVs with stigmata of recent bleeding with a platelet plug in the second portion of duodenum. EVL was done with adequate decompression and no immediate bleeding. One week later, he developed recurrent hematochezia. Full GI work up including upper endoscopy, small bowel capsule and colonoscopy showed previously noted non-bleeding ulcers in the duodenum with no new active bleeding sites.
Case 2: A 68-year-old male with cryptogenic cirrhosis complicated by large hepatocellular carcinoma causing portal vein obstruction was admitted for GI bleeding and hgb of 4.3. Endoscopy showed multiple large DVs with active bleeding. Successful hemostasis was achieved using three hemostatic clips but without adequate decompression. However, given the size of the varix, the patient then underwent successful percutaneous transsplenic porto-venous variceal coil embolization by interventional radiology (IR).
Discussion: Variceal bleeding occurs in 25-30% of cirrhotic patients with ectopic varices accounting for 1-5% of these bleeds. DVs are uncommon but can cause massive hemorrhage with a high mortality up to 40%, due to challenges with treatment. Management options include EVL, sclerotherapy, clipping or IR guided Trans Jugular Intrahepatic Portosystemic Shunt (TIPS), Balloon-Occluded or Coil Assisted Retrograde Transvenous obliteration. One concern with EVL is the size of the DV and risk of re-bleeding. Among case reports using EVL, re-bleeding was seen only in 3/19 cases with hemostasis achieved with repeat banding in 2 out of the three cases. However, for successful band ligation, accessibility, and size of the varices to fit into the banding cap are important factors to consider. Small – medium duodenal varices (case 1) were adequately managed by EVL, however endoscopic decompression could not be completely achieved in large varices (case 2) and eventually required IR guided coil embolization. Therefore, the size and location of the duodenal varices are important factors to be considered in choosing the appropriate management modality for DVs.

Disclosures:
Danyal O. Imam, MBBS1, Beenish Naqvi, MBBS1, Joy Lee, MD2, Steve Serrao, MD1, Christopher Bent, MD1, Pejman Solaimani, MD1. A0319 - Does Size Matter? A Case Series on Management of Duodenal Varices, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Riverside University Health System, Moreno Valley, CA; 2Loma Linda University Medical Center, Loma Linda, CA
Introduction: Duodenal varices (DVs) are a rare cause of life-threatening bleeding in cirrhotic patients. No standardized guidelines for their management exist. We present two cases of DV hemorrhage who were successfully managed by endoscopic variceal band ligation (EVL) and coil embolization respectively.
Case Description/Methods: Case 1: A 63-year-old male with cirrhosis was admitted for upper GI bleeding and Hemoglobin (hgb) of 7.1. Endoscopy showed small to medium-sized DVs with stigmata of recent bleeding with a platelet plug in the second portion of duodenum. EVL was done with adequate decompression and no immediate bleeding. One week later, he developed recurrent hematochezia. Full GI work up including upper endoscopy, small bowel capsule and colonoscopy showed previously noted non-bleeding ulcers in the duodenum with no new active bleeding sites.
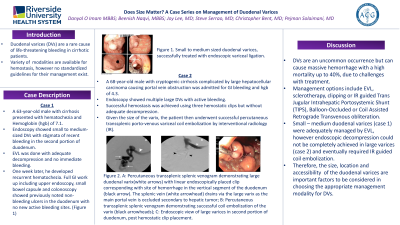
Case 2: A 68-year-old male with cryptogenic cirrhosis complicated by large hepatocellular carcinoma causing portal vein obstruction was admitted for GI bleeding and hgb of 4.3. Endoscopy showed multiple large DVs with active bleeding. Successful hemostasis was achieved using three hemostatic clips but without adequate decompression. However, given the size of the varix, the patient then underwent successful percutaneous transsplenic porto-venous variceal coil embolization by interventional radiology (IR).
Discussion: Variceal bleeding occurs in 25-30% of cirrhotic patients with ectopic varices accounting for 1-5% of these bleeds. DVs are uncommon but can cause massive hemorrhage with a high mortality up to 40%, due to challenges with treatment. Management options include EVL, sclerotherapy, clipping or IR guided Trans Jugular Intrahepatic Portosystemic Shunt (TIPS), Balloon-Occluded or Coil Assisted Retrograde Transvenous obliteration. One concern with EVL is the size of the DV and risk of re-bleeding. Among case reports using EVL, re-bleeding was seen only in 3/19 cases with hemostasis achieved with repeat banding in 2 out of the three cases. However, for successful band ligation, accessibility, and size of the varices to fit into the banding cap are important factors to consider. Small – medium duodenal varices (case 1) were adequately managed by EVL, however endoscopic decompression could not be completely achieved in large varices (case 2) and eventually required IR guided coil embolization. Therefore, the size and location of the duodenal varices are important factors to be considered in choosing the appropriate management modality for DVs.

Figure: A: Percutaneous transsplenic splenic venogram demonstrating large duodenal varix(white arrows) with linear endoscopically placed clip corresponding with site of hemorrhage in the vertical segment of the duodenum (black arrow). The splenic vein (white arrowhead) drains via the large varix as the main portal vein is occluded secondary to hepatic tumor; B: Percutaneous transsplenic splenic venogram demonstrating successful coil embolization of the varix (black arrowheads); C: Endoscopic view of large varices in second portion of duodenum, post hemostatic clip placement.
Disclosures:
Danyal Imam indicated no relevant financial relationships.
Beenish Naqvi indicated no relevant financial relationships.
Joy Lee indicated no relevant financial relationships.
Steve Serrao indicated no relevant financial relationships.
Christopher Bent indicated no relevant financial relationships.
Pejman Solaimani indicated no relevant financial relationships.
Danyal O. Imam, MBBS1, Beenish Naqvi, MBBS1, Joy Lee, MD2, Steve Serrao, MD1, Christopher Bent, MD1, Pejman Solaimani, MD1. A0319 - Does Size Matter? A Case Series on Management of Duodenal Varices, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

