Back

Poster Session B - Monday Morning
Category: IBD
B0432 - An Unexpected Cause of Abdominal Pain in a Patient With Ulcerative Colitis
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- CS
Caleb Shin, BS
Texas A&M College of Medicine
Bryan, TX
Presenting Author(s)
Caleb Shin, BS1, Mimi Tan, MD, MPH2
1Texas A&M College of Medicine, Bryan, TX; 2Baylor College of Medicine, Houston, TX
Introduction: Sickle cell crisis and Ulcerative Colitis (UC) can both present with abdominal pain, which can present a diagnostic challenge in patients with concomitant disease. Thorough work-up is required to appopriately achieve the diagnosis and guide treatment.
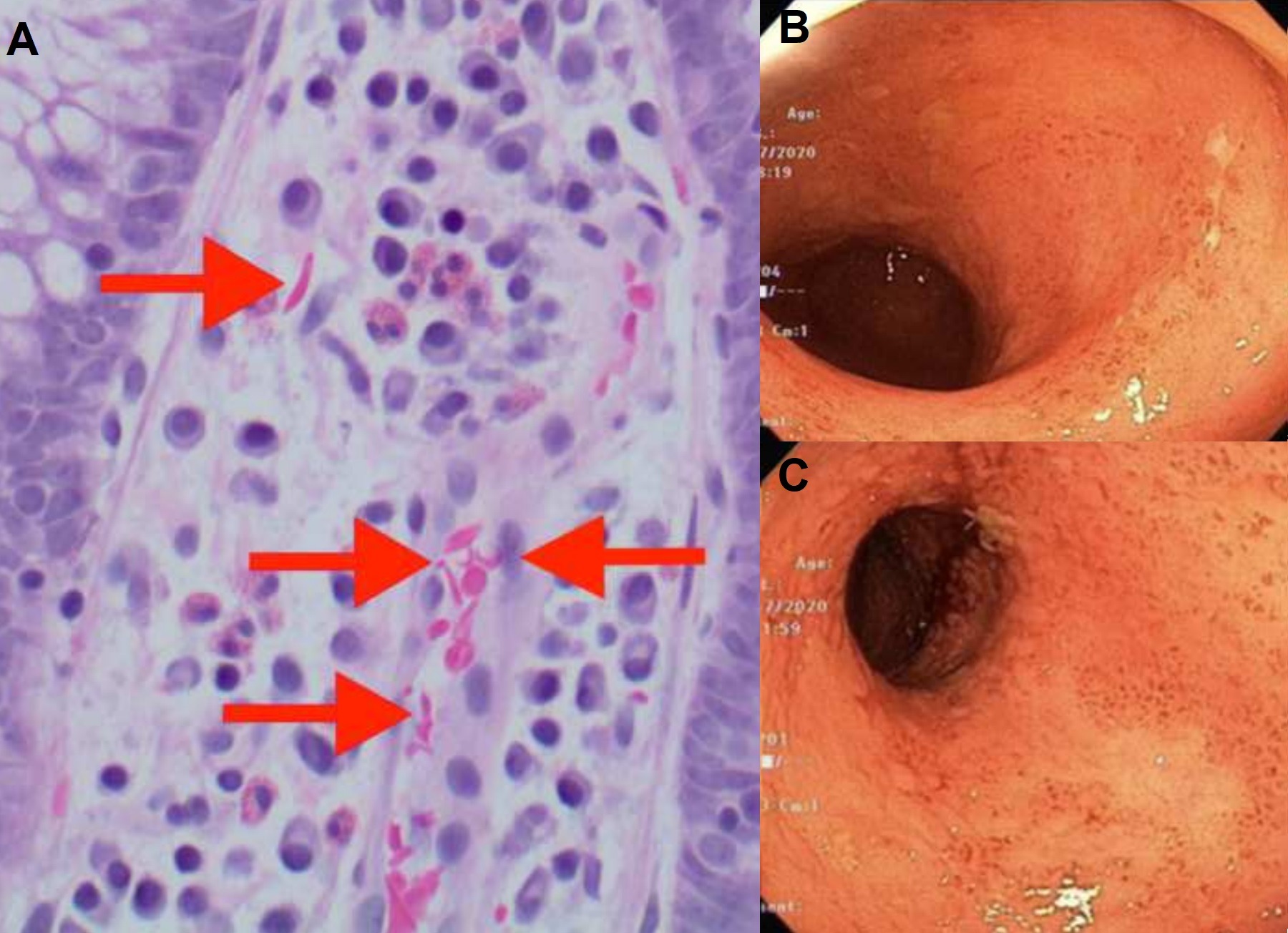
Case Description/Methods: A 27 year old female with a history of UC presented to the ED with non-bloody diarrhea, diffuse abdominal pain, and right lower extremity pain. On exam, she was mildly hypotensive with decreased strength in bilateral lower extremities. CBC showed Hgb 7.6g/dL, and iron panel revealed: iron saturation 28%, elevated ferritin (580.5ng/mL), low haptoglobin ( < 30mg/dL), elevated reticulocyte count (7.47%), and reticulocyte index of 2.05. CT scan showed splenomegaly and diffuse bony infracts. Colonoscopy revealed Mayo 3 ulcerative pancolitis (Fig. 1B and Fig. 1C). Biopsy (Fig. 1A) showed sickle cells in the capillaries and lamina propria with background features of chronic colitis. She was diagnosed with concomitant UC flare and sickle cell crisis. Her sickle cell crisis was managed with IV fluids, analgesics, and folic acid, and her UC was treated with IV solumedrol. She was discharged on a prednisone taper and initiated on infliximab infusions with significant improvement in her symptoms.
Discussion: There is a rare predisposition of SCD to IBD, though the cause is not well elucidated [1]. In these patients, abdominal pain may be either due to SCD crisis or UC flare. Hence, elucidating the cause is important in guiding treatment. While acute pain due to vaso-occlusion often affects the extremities, it can also manifest as abdominal pain due to mesenteric vaso-occlusion. UC on the other hand, typically presents with left lower quadrant abdominal pain with associated diarrhea; however UC can also present with diffuse abdominal pain in the setting of pancolitis. Diarrhea and dehydration due to UC flares could presumably exacerbate SCD leading to more frequent crises. Dehydrated SCD patients, in the setting of travel, were more likely to be hospitalized for vaso-occlusive crises. Additional complications to consider in treating concurrent SCD and UC is avascular necrosis (AVN). AVN is an associated complication of SCD, as well as a side effect of long-term corticosteroid use. Due to the pro-thrombotic state associated with both diseases, prophylactic anticoagulation can also be considered in the setting of immobilization or hospitalization, and do not necessarily have to be stopped due to bloody diarrhea or anemia [3].
Disclosures:
Caleb Shin, BS1, Mimi Tan, MD, MPH2. B0432 - An Unexpected Cause of Abdominal Pain in a Patient With Ulcerative Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Texas A&M College of Medicine, Bryan, TX; 2Baylor College of Medicine, Houston, TX
Introduction: Sickle cell crisis and Ulcerative Colitis (UC) can both present with abdominal pain, which can present a diagnostic challenge in patients with concomitant disease. Thorough work-up is required to appopriately achieve the diagnosis and guide treatment.
Case Description/Methods: A 27 year old female with a history of UC presented to the ED with non-bloody diarrhea, diffuse abdominal pain, and right lower extremity pain. On exam, she was mildly hypotensive with decreased strength in bilateral lower extremities. CBC showed Hgb 7.6g/dL, and iron panel revealed: iron saturation 28%, elevated ferritin (580.5ng/mL), low haptoglobin ( < 30mg/dL), elevated reticulocyte count (7.47%), and reticulocyte index of 2.05. CT scan showed splenomegaly and diffuse bony infracts. Colonoscopy revealed Mayo 3 ulcerative pancolitis (Fig. 1B and Fig. 1C). Biopsy (Fig. 1A) showed sickle cells in the capillaries and lamina propria with background features of chronic colitis. She was diagnosed with concomitant UC flare and sickle cell crisis. Her sickle cell crisis was managed with IV fluids, analgesics, and folic acid, and her UC was treated with IV solumedrol. She was discharged on a prednisone taper and initiated on infliximab infusions with significant improvement in her symptoms.
Discussion: There is a rare predisposition of SCD to IBD, though the cause is not well elucidated [1]. In these patients, abdominal pain may be either due to SCD crisis or UC flare. Hence, elucidating the cause is important in guiding treatment. While acute pain due to vaso-occlusion often affects the extremities, it can also manifest as abdominal pain due to mesenteric vaso-occlusion. UC on the other hand, typically presents with left lower quadrant abdominal pain with associated diarrhea; however UC can also present with diffuse abdominal pain in the setting of pancolitis. Diarrhea and dehydration due to UC flares could presumably exacerbate SCD leading to more frequent crises. Dehydrated SCD patients, in the setting of travel, were more likely to be hospitalized for vaso-occlusive crises. Additional complications to consider in treating concurrent SCD and UC is avascular necrosis (AVN). AVN is an associated complication of SCD, as well as a side effect of long-term corticosteroid use. Due to the pro-thrombotic state associated with both diseases, prophylactic anticoagulation can also be considered in the setting of immobilization or hospitalization, and do not necessarily have to be stopped due to bloody diarrhea or anemia [3].
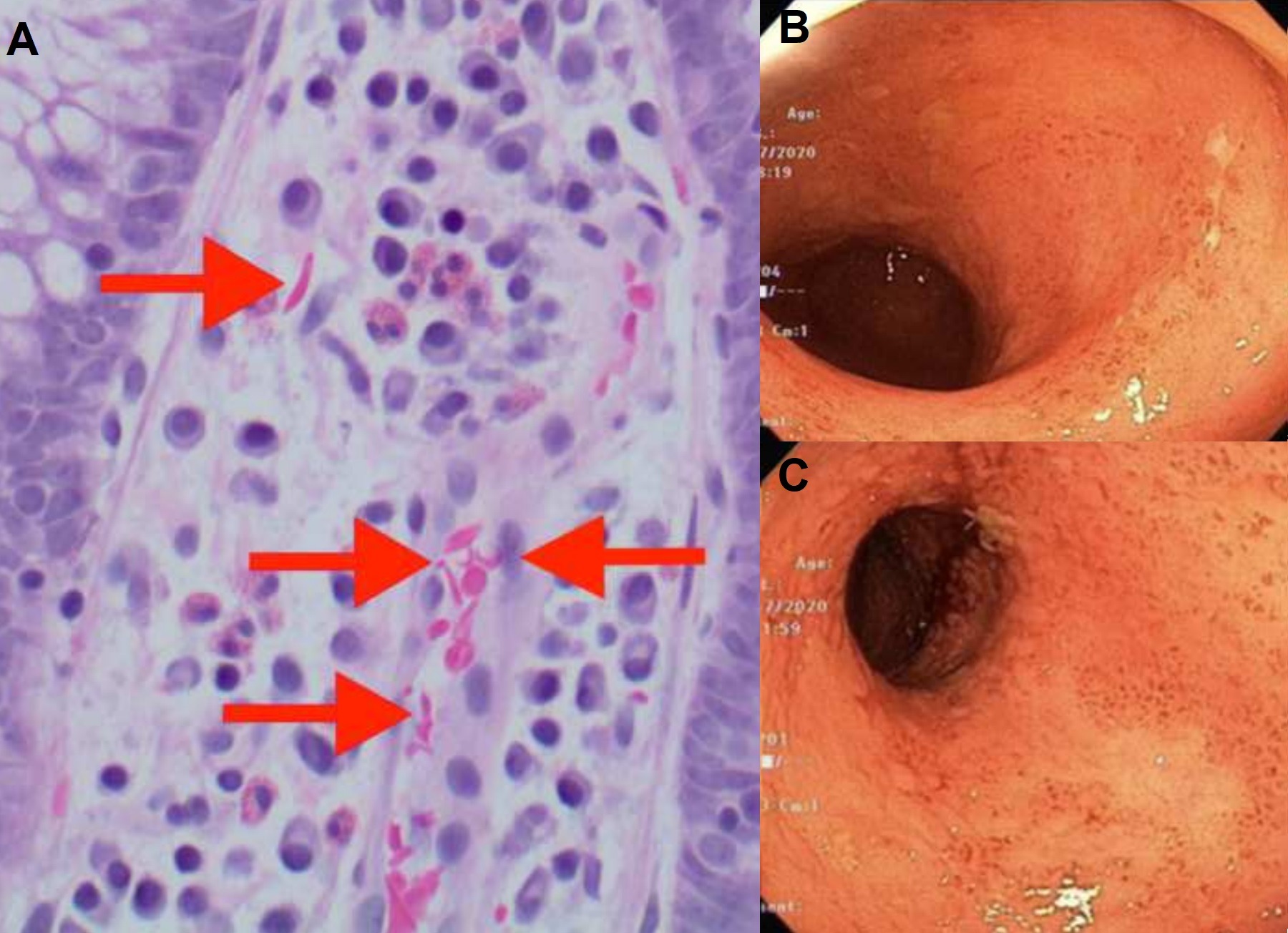
Figure: Fig 1A depicts colonic biopsy demonstrating sickled red blood cells in the lamina propria and capillary
Fig 1B and C depict Mayo 3 pancolitis
Fig 1B and C depict Mayo 3 pancolitis
Disclosures:
Caleb Shin indicated no relevant financial relationships.
Mimi Tan indicated no relevant financial relationships.
Caleb Shin, BS1, Mimi Tan, MD, MPH2. B0432 - An Unexpected Cause of Abdominal Pain in a Patient With Ulcerative Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
