Back


Poster Session A - Sunday Afternoon
Category: Interventional Endoscopy
A0451 - Gastro-Cholecysto-Colonic Fistula Following Endoscopic Ultrasound-Guided Gallbladder Drainage for Stump Cholecystitis: A Case Report
Sunday, October 23, 2022
5:00 PM – 7:00 PM ET
Location: Crown Ballroom

Has Audio
- NK
Nicholas J. Koutlas, MD
Atrium Health - Wake Forest Baptist
Winston-Salem, NC
Presenting Author(s)
Nicholas J. Koutlas, MD1, Swati Pawa, MD2, Girish Mishra, MD2, Rishi Pawa, MBBS2
1Atrium Health - Wake Forest Baptist, Winston-Salem, NC; 2Atrium Health Wake Forest Baptist, Winston-Salem, NC
Introduction: Cholecystocolonic fistulas (CCF) usually occur as a complication of gallstones but cases due to malignancy, peptic ulcers, and Crohn’s disease have been reported. We present a case of a gastro-cholecysto-colonic fistula after endoscopic ultrasound guided-gallbladder drainage (EUS-GBD) for stump cholecystitis.
Case Description/Methods: A 50 year old male presented with abdominal pain. CT scan noted acute cholecystitis. He underwent laparoscopic converted to open subtotal cholecystectomy due to significant inflammation around the gallbladder. He represented 3 weeks later for abdominal pain. CT showed stump cholecystitis. Gastroenterology was consulted for EUS-GBD given his poor surgical candidacy. Diagnostic EUS revealed choledocholithiasis. Endoscopic retrograde cholangiography (ERC) with cholangioscopy, electrohydraulic lithotripsy, and stone removal was completed. Transgastric EUS-GBD with a 10 x 10 mm electrocautery enhanced lumen apposing metal stent (LAMS) was then performed followed by double pigtail stent (DPT) placement within the LAMS.
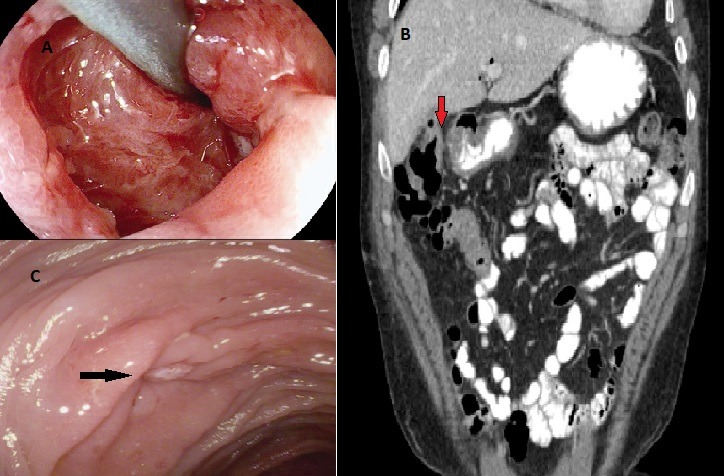
At a follow up visit, abdominal pain resolved but he developed debilitating diarrhea and was started on cholestyramine. Upper endoscopy 4 weeks after EUS-GBD revealed a gastro-cholecysto-colonic fistula with the proximal end of the DPT in the colon. Cholecystoscopy confirmed absence of gallstones so the LAMS and DPT were removed. Clips were used to close the cholecystogastric tract. Oral contrasted CT with delayed images showed tethering of the gallbladder to the hepatic flexure but no extravasation of contrast into the gallbladder from either the stomach or colon. Given this, clinical observation was pursued. Six weeks later, CT noted similar tethering without contrast leak. On colonoscopy, an area of inflamed mucosa at the hepatic flexure was seen without a patent fistula tract. Biopsies showed chronic colitis. Diarrhea subsequently resolved.
Discussion: CCFs are a rare complication of gallstone disease. If untreated, biliary sepsis can occur. Surgery is the standard treatment but endoscopic transpapillary gallbladder drainage with a DPT can promote fistula healing in non-surgical patients. We present a case of a gastro-cholecysto-colonic fistula in a poor surgical candidate after EUS-GBD for stump cholecystitis. This was managed with closure of the cholecystogastric tract. CCF closure occurred spontaneously. In cases of persistent CCF, transpapillary gallbladder drainage should be considered.
Disclosures:
Nicholas J. Koutlas, MD1, Swati Pawa, MD2, Girish Mishra, MD2, Rishi Pawa, MBBS2. A0451 - Gastro-Cholecysto-Colonic Fistula Following Endoscopic Ultrasound-Guided Gallbladder Drainage for Stump Cholecystitis: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Atrium Health - Wake Forest Baptist, Winston-Salem, NC; 2Atrium Health Wake Forest Baptist, Winston-Salem, NC
Introduction: Cholecystocolonic fistulas (CCF) usually occur as a complication of gallstones but cases due to malignancy, peptic ulcers, and Crohn’s disease have been reported. We present a case of a gastro-cholecysto-colonic fistula after endoscopic ultrasound guided-gallbladder drainage (EUS-GBD) for stump cholecystitis.
Case Description/Methods: A 50 year old male presented with abdominal pain. CT scan noted acute cholecystitis. He underwent laparoscopic converted to open subtotal cholecystectomy due to significant inflammation around the gallbladder. He represented 3 weeks later for abdominal pain. CT showed stump cholecystitis. Gastroenterology was consulted for EUS-GBD given his poor surgical candidacy. Diagnostic EUS revealed choledocholithiasis. Endoscopic retrograde cholangiography (ERC) with cholangioscopy, electrohydraulic lithotripsy, and stone removal was completed. Transgastric EUS-GBD with a 10 x 10 mm electrocautery enhanced lumen apposing metal stent (LAMS) was then performed followed by double pigtail stent (DPT) placement within the LAMS.
At a follow up visit, abdominal pain resolved but he developed debilitating diarrhea and was started on cholestyramine. Upper endoscopy 4 weeks after EUS-GBD revealed a gastro-cholecysto-colonic fistula with the proximal end of the DPT in the colon. Cholecystoscopy confirmed absence of gallstones so the LAMS and DPT were removed. Clips were used to close the cholecystogastric tract. Oral contrasted CT with delayed images showed tethering of the gallbladder to the hepatic flexure but no extravasation of contrast into the gallbladder from either the stomach or colon. Given this, clinical observation was pursued. Six weeks later, CT noted similar tethering without contrast leak. On colonoscopy, an area of inflamed mucosa at the hepatic flexure was seen without a patent fistula tract. Biopsies showed chronic colitis. Diarrhea subsequently resolved.
Discussion: CCFs are a rare complication of gallstone disease. If untreated, biliary sepsis can occur. Surgery is the standard treatment but endoscopic transpapillary gallbladder drainage with a DPT can promote fistula healing in non-surgical patients. We present a case of a gastro-cholecysto-colonic fistula in a poor surgical candidate after EUS-GBD for stump cholecystitis. This was managed with closure of the cholecystogastric tract. CCF closure occurred spontaneously. In cases of persistent CCF, transpapillary gallbladder drainage should be considered.
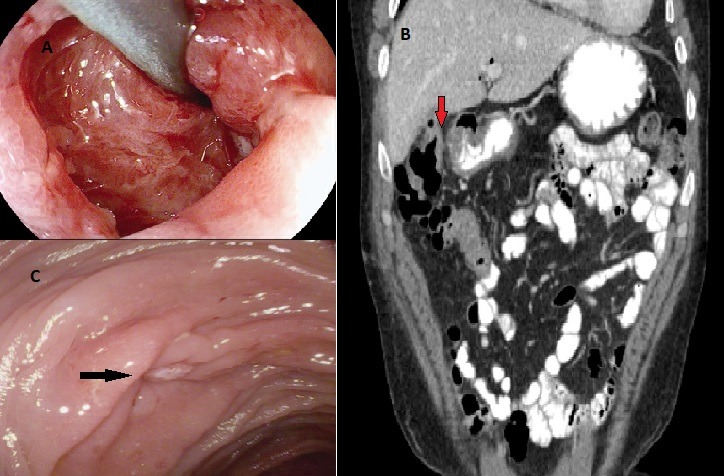
Figure: Figure 1: A. Double pigtail stent migrated into transverse colon with gastro-cholecysto-colonic fistula as viewed from the gallbladder lumen. B. CT scan showing tethering of hepatic flexure to remnant gallbladder (red arrow) without contrast extravasation into the gallbladder from the stomach or colon. C. Closed cholecystocolonic fistula (black arrow) viewed from the hepatic flexure.
Disclosures:
Nicholas Koutlas indicated no relevant financial relationships.
Swati Pawa indicated no relevant financial relationships.
Girish Mishra indicated no relevant financial relationships.
Rishi Pawa indicated no relevant financial relationships.
Nicholas J. Koutlas, MD1, Swati Pawa, MD2, Girish Mishra, MD2, Rishi Pawa, MBBS2. A0451 - Gastro-Cholecysto-Colonic Fistula Following Endoscopic Ultrasound-Guided Gallbladder Drainage for Stump Cholecystitis: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
