Back


Poster Session C - Monday Afternoon
Category: Liver
C0602 - An Unusual Case of Jaundice
Monday, October 24, 2022
3:00 PM – 5:00 PM ET
Location: Crown Ballroom

Has Audio

Lyndie R. Wilkins Parker, DO
Mountain Vista Medical Center
Mesa, AZ
Presenting Author(s)
Lyndie R. Wilkins Parker, DO, Idrees Suliman, MD, Spogmai R. Khan, MD, Abdul Nadir, MD
Mountain Vista Medical Center, Mesa, AZ
Introduction: Peripheral T- Cell Non-Hodgkin’s lymphoma is the most common subtype of hematologic malignancies, which rarely presents as jaundice. Here in, a case of obstructive jaundice attributable to recurrent Peripheral T Cell Lymphoma (PTCL) is described.
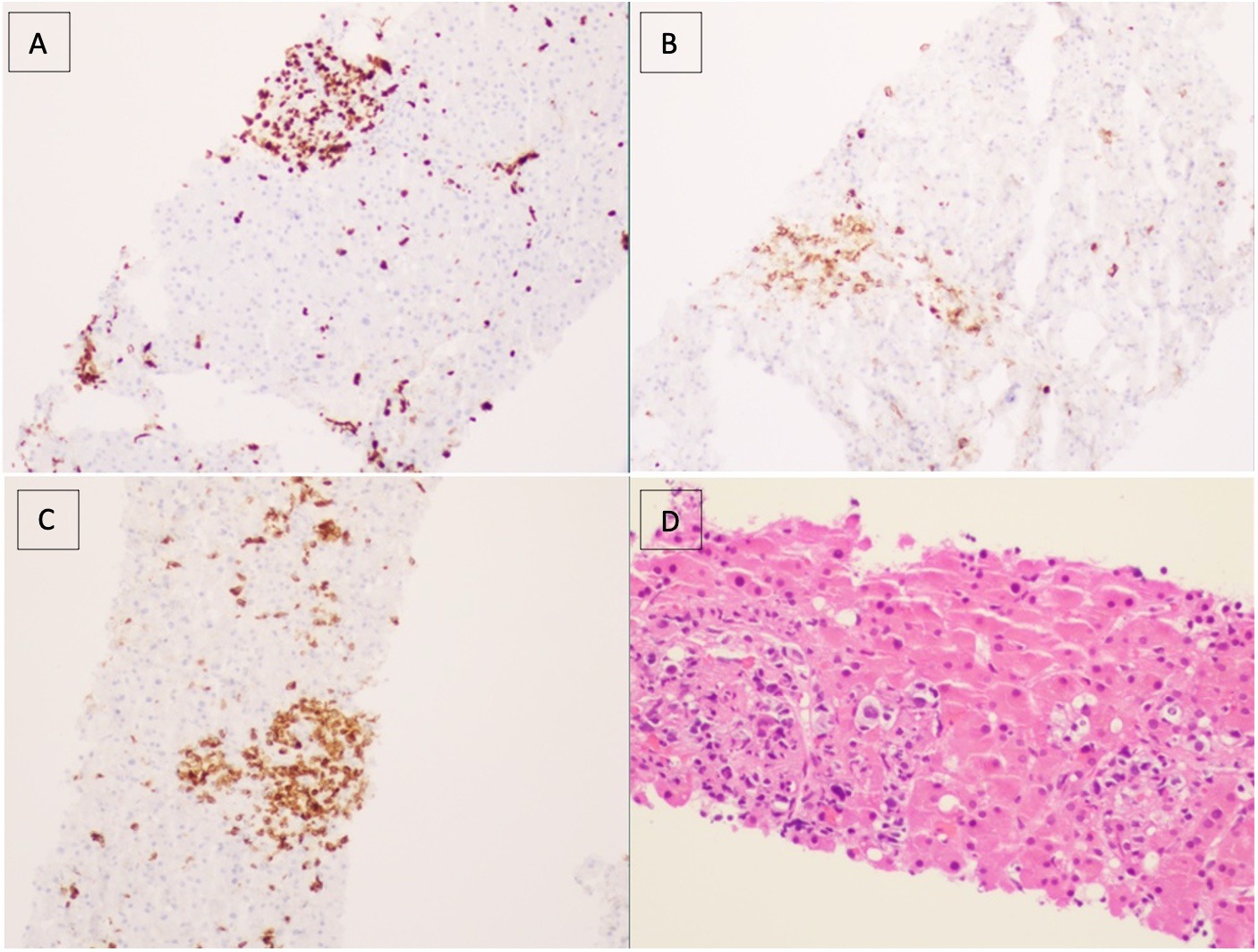
Case Description/Methods: A 75-year-old Caucasian man presented to the Emergency Department with confusion. Fifteen months earlier he was diagnosed with PTCL on axillary lymph node biopsy and treatment with Cyclophosphamide, Etoposide, Prednisolone, and Vincristine (CEOP) was initiated with improvement in his symptoms, primarily itching. Eight months later, he was found to have a cardiac ejection fraction of 20% and a relapse of PTCL was documented. Romidepsin was initiated three months prior to the current hospital admission, but was stopped within three weeks due to the relapse of PTCL, documented on bone marrow biopsy. His liver tests were normal two months prior to admission. On current admission, liver tests showed alkaline phosphatase of 400 IU, AST of 148 IU, ALT 142 IU, and total bilirubin of 3.4 mg/dL. A week later, bilirubin increased to 20.1 IU, being predominantly direct. CT scan and ultrasound of the abdomen, as well as nuclear medicine biliary scan, did not indicate extrahepatic biliary obstruction. A liver biopsy showed diffuse infiltration of the liver parenchyma with abnormal lymphocytes which were stained with CD3+ and CD5+ markers, but did not stain with CD7, documenting relapse of his PTCL in the liver. Diffuse intrahepatic cholestasis was also documented (Image). Two days after the liver biopsy, supportive treatment was withdrawn; and he expired.
Discussion: While the bile duct may be compressed by lymphomatous mass’ anywhere along its path; more commonly at the hepatic hilum (by porta hepatis lymph nodes) and the distal common bile duct (by peripancreatic nodes), canalicular obstruction and resultant intrahepatic cholestasis from relapse in the liver has rarely been reported. This case highlights the importance of performing a liver biopsy to document the diagnosis and provide closure for the family. In this particular situation, the family decided to withdraw care, after a liver biopsy confirmed relapse of PTCL.
Disclosures:
Lyndie R. Wilkins Parker, DO, Idrees Suliman, MD, Spogmai R. Khan, MD, Abdul Nadir, MD. C0602 - An Unusual Case of Jaundice, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Mountain Vista Medical Center, Mesa, AZ
Introduction: Peripheral T- Cell Non-Hodgkin’s lymphoma is the most common subtype of hematologic malignancies, which rarely presents as jaundice. Here in, a case of obstructive jaundice attributable to recurrent Peripheral T Cell Lymphoma (PTCL) is described.
Case Description/Methods: A 75-year-old Caucasian man presented to the Emergency Department with confusion. Fifteen months earlier he was diagnosed with PTCL on axillary lymph node biopsy and treatment with Cyclophosphamide, Etoposide, Prednisolone, and Vincristine (CEOP) was initiated with improvement in his symptoms, primarily itching. Eight months later, he was found to have a cardiac ejection fraction of 20% and a relapse of PTCL was documented. Romidepsin was initiated three months prior to the current hospital admission, but was stopped within three weeks due to the relapse of PTCL, documented on bone marrow biopsy. His liver tests were normal two months prior to admission. On current admission, liver tests showed alkaline phosphatase of 400 IU, AST of 148 IU, ALT 142 IU, and total bilirubin of 3.4 mg/dL. A week later, bilirubin increased to 20.1 IU, being predominantly direct. CT scan and ultrasound of the abdomen, as well as nuclear medicine biliary scan, did not indicate extrahepatic biliary obstruction. A liver biopsy showed diffuse infiltration of the liver parenchyma with abnormal lymphocytes which were stained with CD3+ and CD5+ markers, but did not stain with CD7, documenting relapse of his PTCL in the liver. Diffuse intrahepatic cholestasis was also documented (Image). Two days after the liver biopsy, supportive treatment was withdrawn; and he expired.
Discussion: While the bile duct may be compressed by lymphomatous mass’ anywhere along its path; more commonly at the hepatic hilum (by porta hepatis lymph nodes) and the distal common bile duct (by peripancreatic nodes), canalicular obstruction and resultant intrahepatic cholestasis from relapse in the liver has rarely been reported. This case highlights the importance of performing a liver biopsy to document the diagnosis and provide closure for the family. In this particular situation, the family decided to withdraw care, after a liver biopsy confirmed relapse of PTCL.
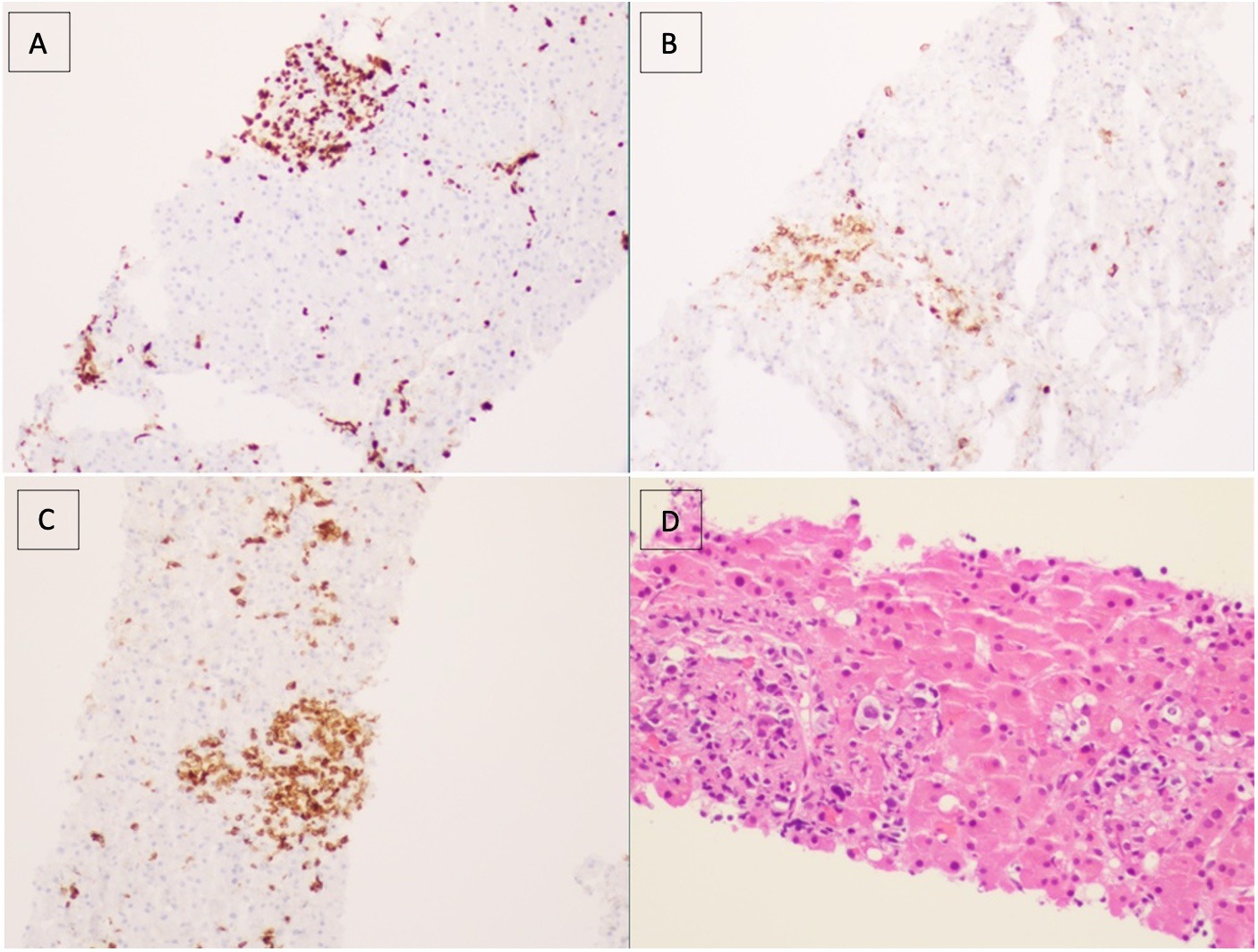
Figure: Image 1: Random Liver Needle Biopsy Staining- Ki-67(A), CD30(B), CD3(C), and H&E(D)
Disclosures:
Lyndie Wilkins Parker indicated no relevant financial relationships.
Idrees Suliman indicated no relevant financial relationships.
Spogmai Khan indicated no relevant financial relationships.
Abdul Nadir indicated no relevant financial relationships.
Lyndie R. Wilkins Parker, DO, Idrees Suliman, MD, Spogmai R. Khan, MD, Abdul Nadir, MD. C0602 - An Unusual Case of Jaundice, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

