Back

Poster Session D - Tuesday Morning
Category: Esophagus
D0221 - Treatment of Achalasia With Endoscopic Ultrasound-Guided Botulinum Injection in the Setting of Esophageal Varices
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

R. Christopher Chase, MD
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Award: Presidential Poster Award
R. Christopher Chase, MD1, Liu Yang, MBBS1, Victoria Gomez, MD1, Maoyin Pang, MD, PhD2
1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic Florida, Jacksonville, FL
Introduction: Achalasia in the setting of esophageal varices prompts difficult decisions in management given potential complications from liver disease and increased risk of variceal bleeding from stagnant food causing esophageal inflammation. Considering treatment options like pneumatic dilation, botulinum toxin injection, peroral endoscopic myotomy, or heller myotomy presents a challenging dilemma. We describe a case of achalasia treated with endoscopic ultrasound (EUS) guided botulinum toxin injection in a patient with esophageal varices.
Case Description/Methods: A 69-year-old man with cirrhosis secondary to non-alcoholic steatohepatitis complicated by esophageal varices, portal hypertensive gastropathy, and portal vein thrombosis presented with dysphagia and malnourishment. Grade 2 large middle and lower esophageal varices and a Schatzki ring were found during esophagogastroduodenoscopy (EGD) and dilated with a through-the-scope balloon to 18mm. His dysphagia partially improved. Esophageal manometry showed pan-pressurization consistent with type 2 achalasia. Given his varices and 30 day post operative mortality risk of 34%, surgical management such as Heller myotomy was excluded. Co-existing achalasia with dysphagia made it more challenging to treat the esophageal varices in 3 separate EGD’s.
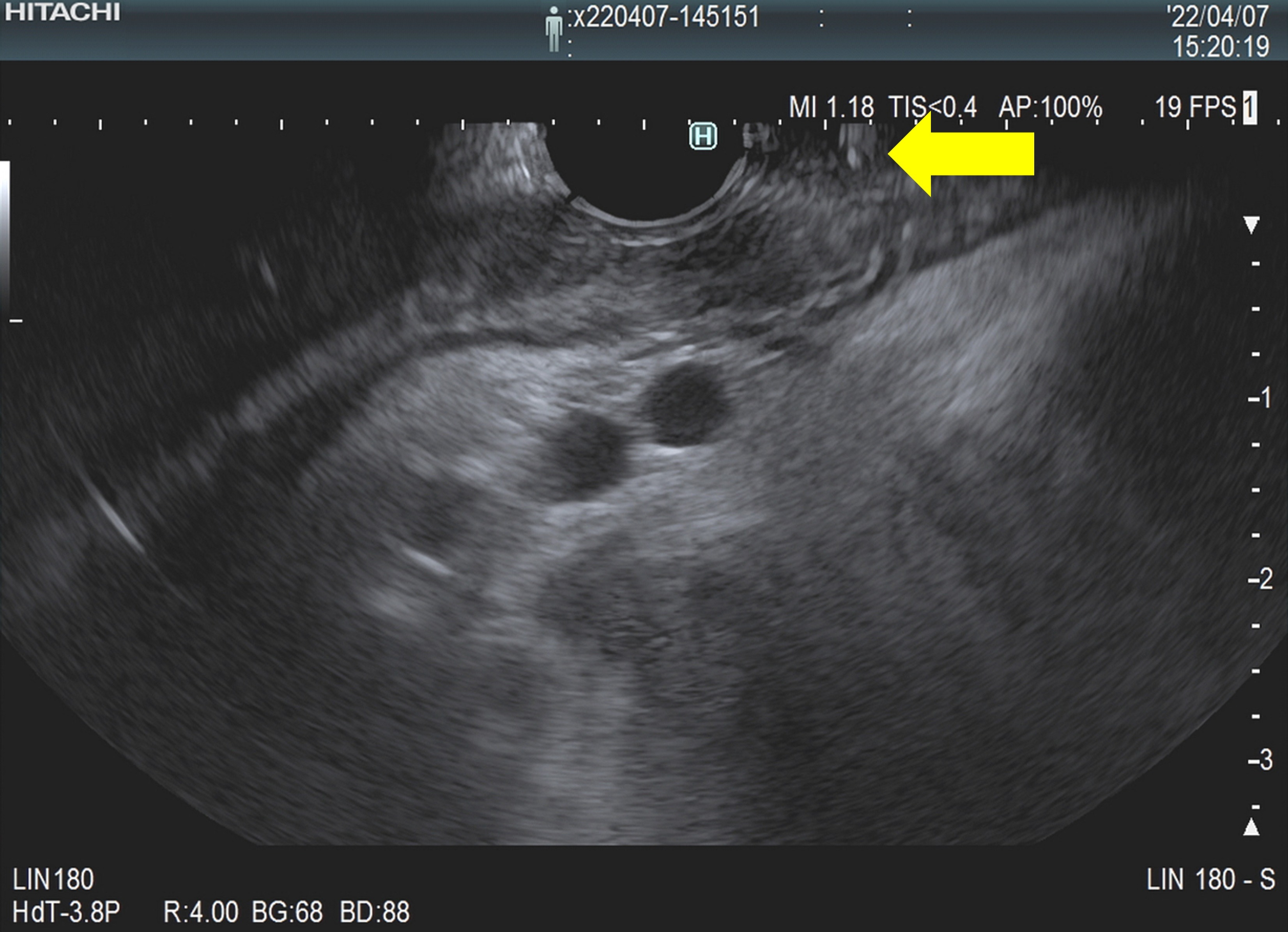
After multidisciplinary discussion, it was decided to proceed with an EUS-guided Botulinum toxin (Botox) injection for the treatment of achalasia. The muscularis propia (MP) of the lower esophageal sphincter (LES) was identified by EUS, which was used to guide an endoscopic needle into this layer for injection of 100 units of botulinum toxin while avoiding intervening vessels and varices. Varices were subsequently ligated. On follow-up, the patient was able to eat and drink normally.
Discussion: In patients with liver cirrhosis, achalasia worsens nutritional status which could prevent candidacy for transplant. Botox injections can temporarily counteract the loss of inhibitory neuron function in achalasia by inhibiting acetylcholine release in the excitatory neurons that stimulate the LES. This provides an important window to improve nutritional status and likelihood of transplant candidacy. EUS-guided Botox injection to avoid varices followed by variceal ligation is potentially a safer method for delivering botulinum toxin to the LES. EUS allows identification of the MP and identifies an endoscopic needle trajectory that will not course through any potential vessels, such as varices as demonstrated in this case.
Disclosures:
R. Christopher Chase, MD1, Liu Yang, MBBS1, Victoria Gomez, MD1, Maoyin Pang, MD, PhD2. D0221 - Treatment of Achalasia With Endoscopic Ultrasound-Guided Botulinum Injection in the Setting of Esophageal Varices, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
R. Christopher Chase, MD1, Liu Yang, MBBS1, Victoria Gomez, MD1, Maoyin Pang, MD, PhD2
1Mayo Clinic, Jacksonville, FL; 2Mayo Clinic Florida, Jacksonville, FL
Introduction: Achalasia in the setting of esophageal varices prompts difficult decisions in management given potential complications from liver disease and increased risk of variceal bleeding from stagnant food causing esophageal inflammation. Considering treatment options like pneumatic dilation, botulinum toxin injection, peroral endoscopic myotomy, or heller myotomy presents a challenging dilemma. We describe a case of achalasia treated with endoscopic ultrasound (EUS) guided botulinum toxin injection in a patient with esophageal varices.
Case Description/Methods: A 69-year-old man with cirrhosis secondary to non-alcoholic steatohepatitis complicated by esophageal varices, portal hypertensive gastropathy, and portal vein thrombosis presented with dysphagia and malnourishment. Grade 2 large middle and lower esophageal varices and a Schatzki ring were found during esophagogastroduodenoscopy (EGD) and dilated with a through-the-scope balloon to 18mm. His dysphagia partially improved. Esophageal manometry showed pan-pressurization consistent with type 2 achalasia. Given his varices and 30 day post operative mortality risk of 34%, surgical management such as Heller myotomy was excluded. Co-existing achalasia with dysphagia made it more challenging to treat the esophageal varices in 3 separate EGD’s.
After multidisciplinary discussion, it was decided to proceed with an EUS-guided Botulinum toxin (Botox) injection for the treatment of achalasia. The muscularis propia (MP) of the lower esophageal sphincter (LES) was identified by EUS, which was used to guide an endoscopic needle into this layer for injection of 100 units of botulinum toxin while avoiding intervening vessels and varices. Varices were subsequently ligated. On follow-up, the patient was able to eat and drink normally.
Discussion: In patients with liver cirrhosis, achalasia worsens nutritional status which could prevent candidacy for transplant. Botox injections can temporarily counteract the loss of inhibitory neuron function in achalasia by inhibiting acetylcholine release in the excitatory neurons that stimulate the LES. This provides an important window to improve nutritional status and likelihood of transplant candidacy. EUS-guided Botox injection to avoid varices followed by variceal ligation is potentially a safer method for delivering botulinum toxin to the LES. EUS allows identification of the MP and identifies an endoscopic needle trajectory that will not course through any potential vessels, such as varices as demonstrated in this case.
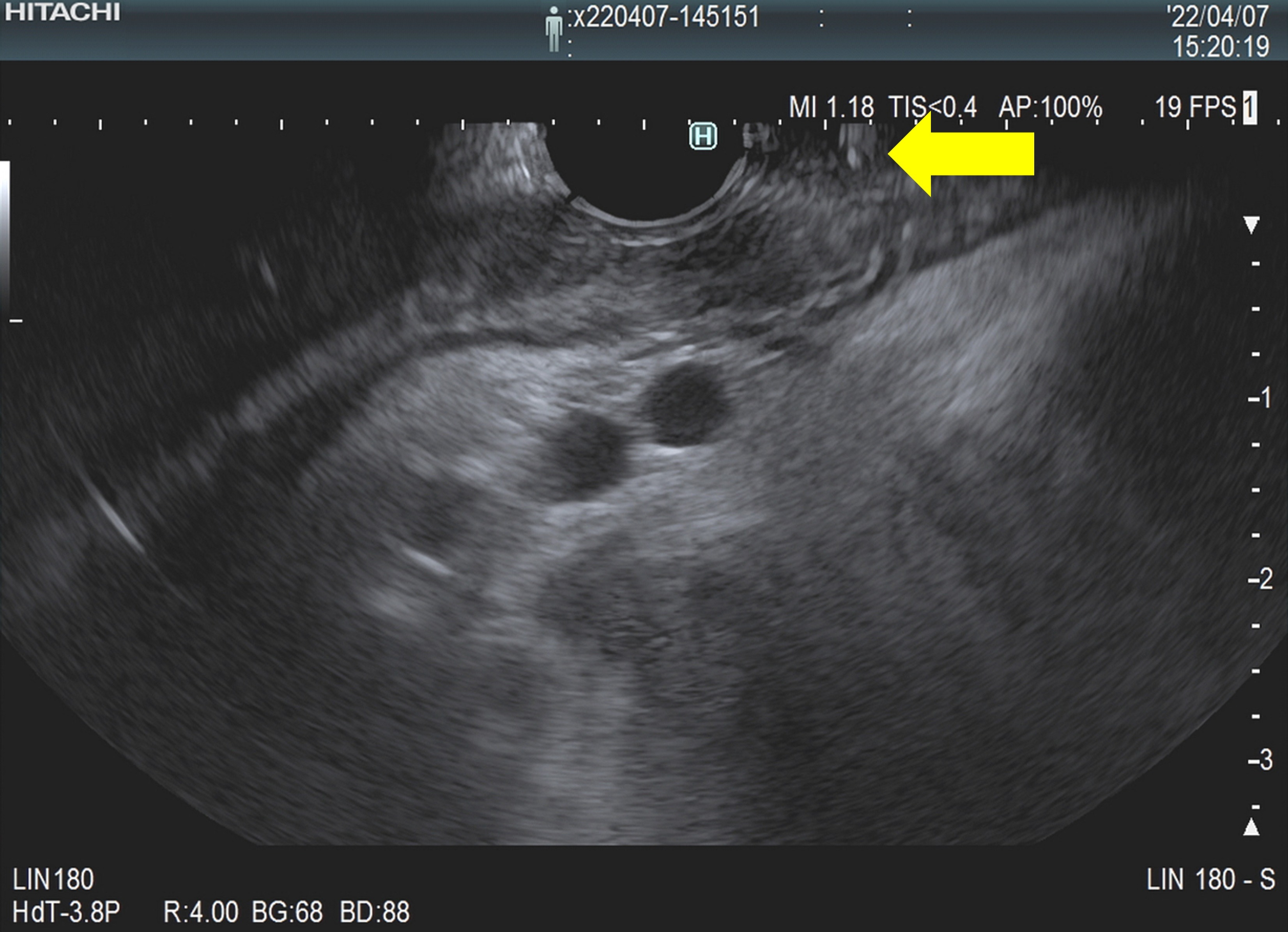
Figure: EUS demonstrating avoidance of esophageal varices as the endoscopic needle advanced towards the muscularis propia for botulinum toxin injection at the lower esophageal sphincter.
Disclosures:
R. Christopher Chase indicated no relevant financial relationships.
Liu Yang indicated no relevant financial relationships.
Victoria Gomez indicated no relevant financial relationships.
Maoyin Pang indicated no relevant financial relationships.
R. Christopher Chase, MD1, Liu Yang, MBBS1, Victoria Gomez, MD1, Maoyin Pang, MD, PhD2. D0221 - Treatment of Achalasia With Endoscopic Ultrasound-Guided Botulinum Injection in the Setting of Esophageal Varices, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

