Back

Poster Session D - Tuesday Morning
Category: Esophagus
D0223 - Benign Bronchoesophageal Fistula Recalcitrant to Endoscopic Management
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Thomas Fredrick, MD
Mayo Clinic Rochester
Rochester, MN
Presenting Author(s)
Ye Zhu, MD, PhD1, Thomas Fredrick, MD2, Louis Wong Kee Song, MD1, Xiao Jing (Iris) Wang, MD1
1Mayo Clinic, Rochester, MN; 2Mayo Clinic Rochester, Rochester, MN
Introduction: The management of bronchoesophageal fistulas (BEFs) can be challenging and often requires a multidisciplinary approach. We present the case of a spontaneous BEF that defied multiple endoscopic attempts at closure.
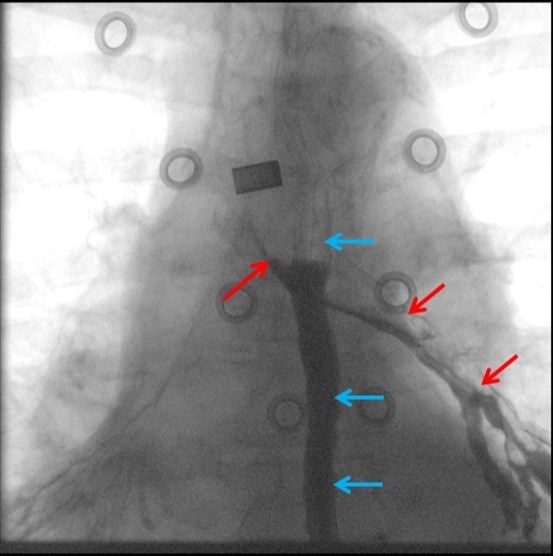
Case Description/Methods: A 69-year-old malnourished woman with heavy tobacco use and chronic obstructive pulmonary disease presented with cough incited by food intake and pneumonia. Fluoroscopic contrast study highlighted a bronchoesophageal fistula with opacification of the left mainstem bronchus (Figure 1). An initial upper endoscopy demonstrated a small recess but without an obvious fistulous opening at 29 cm from the incisors and without malignancy on biopsy. A subcarinal 2.3 cm broncholith seen on a chest CT performed 2 years prior was now noticeably absent, suggesting broncholith erosion as the cause of the BEF. An attempt at endoscopic closure was recommended by multidisciplinary consensus. Since the fistulous opening was not readily identifiable at initial endoscopy, a combined bronchoscopic-endoscopic procedure was performed with bronchoscopic passage of a guidewire through the fistula tract into the esophagus. Once localized, abrasion of the fistula orifice with argon plasma coagulation followed by over-the-scope clip (OTSC) closure was performed. Symptom and radiographic recurrence at 2 weeks from migration of the OTSC resulted in uneventful endoscopic removal of the OTSC. Subsequent placement of a fully covered self-expandable metal stent with endoscopic suture fixation resulted in intolerable chest pain despite narcotic administration and incomplete sealing of the fistula on radiographic imaging, necessitating stent removal one week later. A third attempt at endoscopic suture closure of the fistula was unsuccessful. A PEG-J feeding tube was placed for enteral nutrition as well as a retrograde pigtail drainage catheter fitted through the PEG to manage secretions at and above the BEF. Definitive surgical repair will be considered once her nutritional status is optimized.
Discussion: Despite publications of successful endoscopic closure of benign BEFs, a significant proportion of these cases do not respond to endoscopic interventions and are not likely to be reported in the literature (reporting bias). Benign BEFs should be managed in a multidisciplinary fashion and alternative treatment strategies pursued when endoscopic therapies are deemed unsuitable or fail at closing the fistula.
Disclosures:
Ye Zhu, MD, PhD1, Thomas Fredrick, MD2, Louis Wong Kee Song, MD1, Xiao Jing (Iris) Wang, MD1. D0223 - Benign Bronchoesophageal Fistula Recalcitrant to Endoscopic Management, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Mayo Clinic, Rochester, MN; 2Mayo Clinic Rochester, Rochester, MN
Introduction: The management of bronchoesophageal fistulas (BEFs) can be challenging and often requires a multidisciplinary approach. We present the case of a spontaneous BEF that defied multiple endoscopic attempts at closure.
Case Description/Methods: A 69-year-old malnourished woman with heavy tobacco use and chronic obstructive pulmonary disease presented with cough incited by food intake and pneumonia. Fluoroscopic contrast study highlighted a bronchoesophageal fistula with opacification of the left mainstem bronchus (Figure 1). An initial upper endoscopy demonstrated a small recess but without an obvious fistulous opening at 29 cm from the incisors and without malignancy on biopsy. A subcarinal 2.3 cm broncholith seen on a chest CT performed 2 years prior was now noticeably absent, suggesting broncholith erosion as the cause of the BEF. An attempt at endoscopic closure was recommended by multidisciplinary consensus. Since the fistulous opening was not readily identifiable at initial endoscopy, a combined bronchoscopic-endoscopic procedure was performed with bronchoscopic passage of a guidewire through the fistula tract into the esophagus. Once localized, abrasion of the fistula orifice with argon plasma coagulation followed by over-the-scope clip (OTSC) closure was performed. Symptom and radiographic recurrence at 2 weeks from migration of the OTSC resulted in uneventful endoscopic removal of the OTSC. Subsequent placement of a fully covered self-expandable metal stent with endoscopic suture fixation resulted in intolerable chest pain despite narcotic administration and incomplete sealing of the fistula on radiographic imaging, necessitating stent removal one week later. A third attempt at endoscopic suture closure of the fistula was unsuccessful. A PEG-J feeding tube was placed for enteral nutrition as well as a retrograde pigtail drainage catheter fitted through the PEG to manage secretions at and above the BEF. Definitive surgical repair will be considered once her nutritional status is optimized.
Discussion: Despite publications of successful endoscopic closure of benign BEFs, a significant proportion of these cases do not respond to endoscopic interventions and are not likely to be reported in the literature (reporting bias). Benign BEFs should be managed in a multidisciplinary fashion and alternative treatment strategies pursued when endoscopic therapies are deemed unsuitable or fail at closing the fistula.
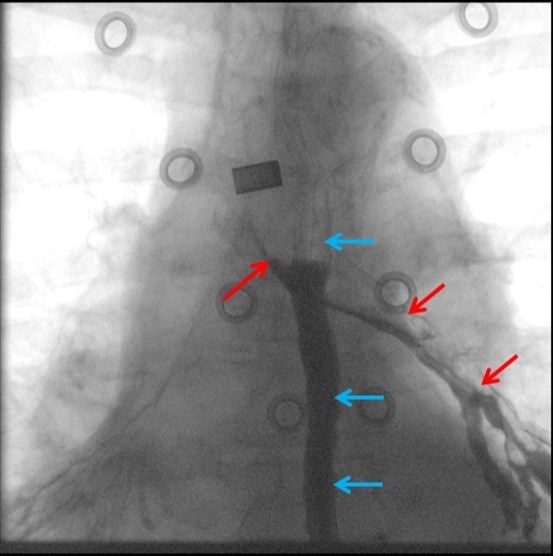
Figure: Figure 1. Esophagram highlighting bronchoesophageal fistula. Esophagus (blue arrows); left mainstem bronchi (red arrows).
Disclosures:
Ye Zhu indicated no relevant financial relationships.
Thomas Fredrick indicated no relevant financial relationships.
Louis Wong Kee Song: Intuitive Surgical – Consultant. Intuitive Surgical, Inc. – Consultant. Steris – Consultant. Steris Inc. – Consultant.
Xiao Jing (Iris) Wang indicated no relevant financial relationships.
Ye Zhu, MD, PhD1, Thomas Fredrick, MD2, Louis Wong Kee Song, MD1, Xiao Jing (Iris) Wang, MD1. D0223 - Benign Bronchoesophageal Fistula Recalcitrant to Endoscopic Management, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
