Back
Poster Session B - Monday Morning
Category: GI Bleeding
B0330 - Where's That Bleed?! A Case of Intermittent Ectopic Jejunal Variceal Bleeding
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Aaron Fein, DO
University of Kentucky
Lexington, KY
Presenting Author(s)
Aaron Fein, DO1, Naba Saeed, MD2, Hammad Qureshi, MD1, Steven I. Shedlofsky, MD3
1University of Kentucky, Lexington, KY; 2The University of Kentucky, Lexington, KY; 3University of Kentucky College of Medicine, Lexington, KY
Introduction: Variceal bleeding is a potentially life-threatening complication of cirrhosis. Although most often found in the esophagus and stomach, collateral pathways can develop throughout the abdomen in the setting of portal hypertension leading to “ectopic” varices eg retro/intra-peritoneal, small bowel, rectal, urinary bladder and biliary tract varices. They demonstrate hepatofugal flow on imaging, but are difficult to find, which may delay therapeutic interventions. Here, we present a patient with recurrent hematochezia secondary to ectopic jejunal variceal bleeding.
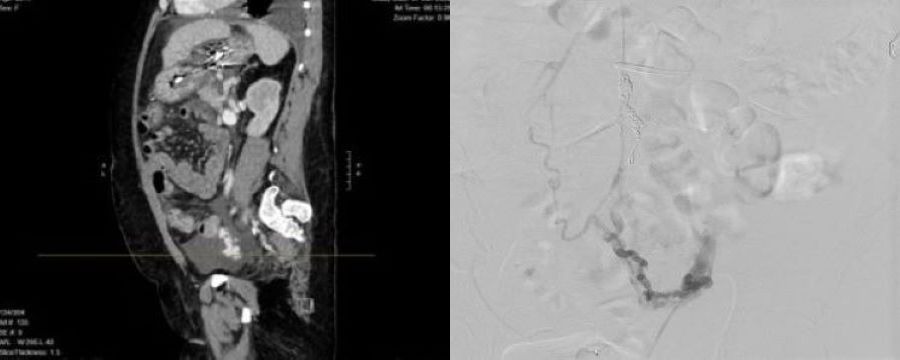
Case Description/Methods: A 51-year-old female with hepatitis C/alcohol related cirrhosis, decompensated by variceal bleeding s/p TIPS, ascites and HE, presented with melena. EGD: superficial esophageal tears, as well as a clot overlying a varix, for which three bands were placed. Her hemoglobin declined from 11.6 to 6.1 g/dL with worsening encephalopathy, vital instability, intermittent hematochezia, and fever. Repeat EGD: healing post-banding ulcers without active bleeding. Colonoscopy: numerous superficial ulcers with adherent clots, but no active bleeding; biopsies consistent with ischemic colitis. CTA was done without active extravasation identified. US abdomen showed distal TIPS stenosis, so IR was consulted for TIPS revision. The volume of hematochezia then became profuse. STAT CTA found an area of jejunal blush and angiography revealed an ectopic SMV branch varix to the jejunum with aberrant connection to the left ovarian vein, which was embolized. Her TIPS was also revised, with a decrease in porto-systemic pressure gradient from 16 to 7 mmHg. Subsequently, her bleeding resolved, hemodynamics and encephalopathy improved, and she was ultimately extubated and transferred to the floor.
Discussion: Ectopic varices account for up to 5% of variceal bleeds with a bleeding rate thought to be 4 times higher than esophageal varices and a reported mortality up to 40%. About 17% are jejunal/ileal varices. Rapid detection and treatment by embolization and reduction in portal pressures via TIPS, BRTO or portal vein stenting are key. In our patient, despite delay in diagnosis due to intermittent bleeding, hemostasis was finally achieved with direct embolization and reduction in portal pressure. It is imperative that a high suspicion be maintained for ectopic varices in any patient with portal hypertension and intra/extraluminal signs of bleeding, and other modalities such as MRA or CT enterography be utilized if endoscopy/CTA are non-revealing.
Disclosures:
Aaron Fein, DO1, Naba Saeed, MD2, Hammad Qureshi, MD1, Steven I. Shedlofsky, MD3. B0330 - Where's That Bleed?! A Case of Intermittent Ectopic Jejunal Variceal Bleeding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Kentucky, Lexington, KY; 2The University of Kentucky, Lexington, KY; 3University of Kentucky College of Medicine, Lexington, KY
Introduction: Variceal bleeding is a potentially life-threatening complication of cirrhosis. Although most often found in the esophagus and stomach, collateral pathways can develop throughout the abdomen in the setting of portal hypertension leading to “ectopic” varices eg retro/intra-peritoneal, small bowel, rectal, urinary bladder and biliary tract varices. They demonstrate hepatofugal flow on imaging, but are difficult to find, which may delay therapeutic interventions. Here, we present a patient with recurrent hematochezia secondary to ectopic jejunal variceal bleeding.
Case Description/Methods: A 51-year-old female with hepatitis C/alcohol related cirrhosis, decompensated by variceal bleeding s/p TIPS, ascites and HE, presented with melena. EGD: superficial esophageal tears, as well as a clot overlying a varix, for which three bands were placed. Her hemoglobin declined from 11.6 to 6.1 g/dL with worsening encephalopathy, vital instability, intermittent hematochezia, and fever. Repeat EGD: healing post-banding ulcers without active bleeding. Colonoscopy: numerous superficial ulcers with adherent clots, but no active bleeding; biopsies consistent with ischemic colitis. CTA was done without active extravasation identified. US abdomen showed distal TIPS stenosis, so IR was consulted for TIPS revision. The volume of hematochezia then became profuse. STAT CTA found an area of jejunal blush and angiography revealed an ectopic SMV branch varix to the jejunum with aberrant connection to the left ovarian vein, which was embolized. Her TIPS was also revised, with a decrease in porto-systemic pressure gradient from 16 to 7 mmHg. Subsequently, her bleeding resolved, hemodynamics and encephalopathy improved, and she was ultimately extubated and transferred to the floor.
Discussion: Ectopic varices account for up to 5% of variceal bleeds with a bleeding rate thought to be 4 times higher than esophageal varices and a reported mortality up to 40%. About 17% are jejunal/ileal varices. Rapid detection and treatment by embolization and reduction in portal pressures via TIPS, BRTO or portal vein stenting are key. In our patient, despite delay in diagnosis due to intermittent bleeding, hemostasis was finally achieved with direct embolization and reduction in portal pressure. It is imperative that a high suspicion be maintained for ectopic varices in any patient with portal hypertension and intra/extraluminal signs of bleeding, and other modalities such as MRA or CT enterography be utilized if endoscopy/CTA are non-revealing.
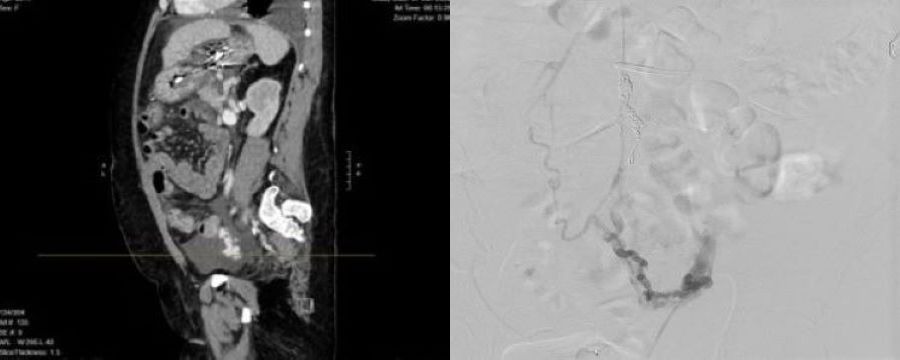
Figure: Figure 1: (a) Sagittal view of computed tomography angiography (CTA) and (b) angiogram evidence of jejunal blush and ectopic jejunal varix with aberrant connection to the left ovarian vein, respectively.
Disclosures:
Aaron Fein indicated no relevant financial relationships.
Naba Saeed indicated no relevant financial relationships.
Hammad Qureshi indicated no relevant financial relationships.
Steven Shedlofsky indicated no relevant financial relationships.
Aaron Fein, DO1, Naba Saeed, MD2, Hammad Qureshi, MD1, Steven I. Shedlofsky, MD3. B0330 - Where's That Bleed?! A Case of Intermittent Ectopic Jejunal Variceal Bleeding, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
