Back

Poster Session B - Monday Morning
Category: Biliary/Pancreas
B0029 - A Case of Pancreaticobiliary Actinomycosis Mimicking a Mass
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Sylvia Keiser, DO
University of Texas Health San Antonio
San Antonio, TX
Presenting Author(s)
Sylvia Keiser, DO, Laura Rosenkranz, MD
University of Texas Health San Antonio, San Antonio, TX
Introduction: Actinomyces are gram-positive anaerobic bacteria habitually found in the oral cavity, gastrointestinal and female genital tract. In rare cases, these bacteria may disrupt mucosal integrity and cause actinomycosis, a disease characterized by abscess and sinus tract formation, and fibrosis. We present a case of pancreaticobiliary actinomycosis.
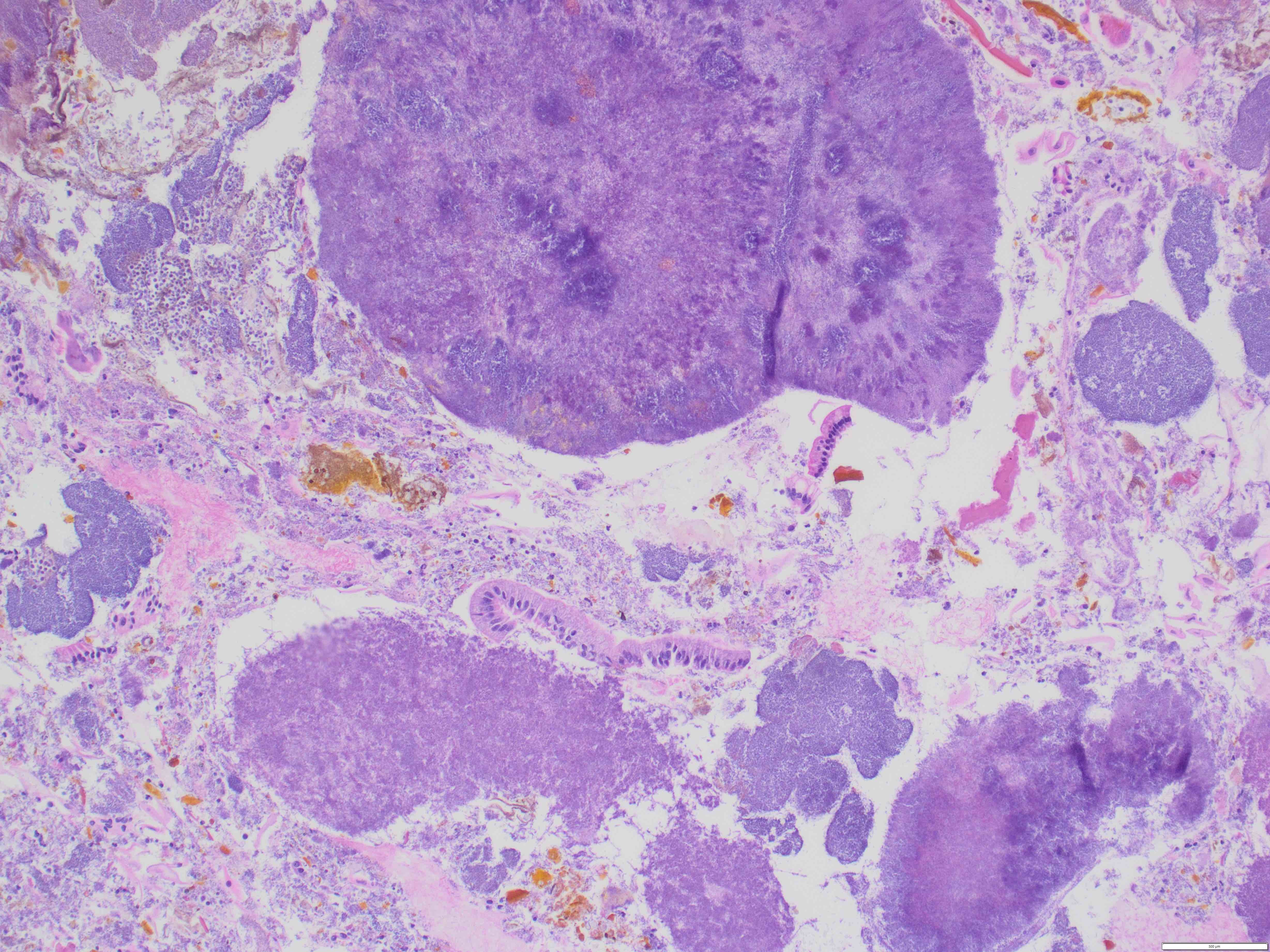
Case Description/Methods: 50-year-old male with history of chronic pancreatitis complicated by biliary stricture requiring serial biliary stenting presented to the hospital with abdominal pain, decreased appetite, weight loss, and low-grade fevers. On exam the patient was hemodynamically stable and had mild epigastric abdominal tenderness. Labs revealed a lipase of 105 U/L, AST 20 U/L, ALT 18 U/L and total bilirubin of 0.7 mg/dL. Cross sectional imaging (CT scan) of the abdomen demonstrated a liver and pancreatic head mass at an outside institution two weeks prior to admission. Magnetic resonance cholangiopancreatography (MRCP) demonstrated dilated intrahepatic biliary ducts, bile duct of 11 mm with a stent in place, and intraluminal filling defects consistent of choledocholithiasis. Pancreatic head and body appeared bulky and heterogenous, whereas the pancreatic tail was atrophic. No focal liver lesions were seen. The patient underwent an endoscopic ultrasound which revealed calcific pancreatitis without solid masses. Endoscopic retrograde cholangiopancreatography (ERCP) was performed and the biliary stent was removed and sent for cytology. Cytology was negative for malignancy, however bacterial colonies consistent with actinomyces were found. Infectious disease service recommended the patient complete six weeks of ceftriaxone. After completion of treatment, his appetite returned, weight loss improved, and fevers resolved. Amoxicillin followed as maintenance therapy for approximately twelve months.
Discussion: The symptoms of pancreaticobiliary actinomycosis are non-specific, making the diagnosis difficult. Actinomycosis should be included in the differential diagnosis when a pancreatic or liver mass is found, especially in a patient with a history of pancreatic or biliary stenting. In these patients, we suspect that the repeat cannulation of the bile duct during an ERCP may lead to mucosal disruption, allowing bacteria to infect the tissue. It is important for endoscopists to consider actinomycosis and pursue histopathological confirmation to prevent unnecessary surgical intervention.
Disclosures:
Sylvia Keiser, DO, Laura Rosenkranz, MD. B0029 - A Case of Pancreaticobiliary Actinomycosis Mimicking a Mass, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Texas Health San Antonio, San Antonio, TX
Introduction: Actinomyces are gram-positive anaerobic bacteria habitually found in the oral cavity, gastrointestinal and female genital tract. In rare cases, these bacteria may disrupt mucosal integrity and cause actinomycosis, a disease characterized by abscess and sinus tract formation, and fibrosis. We present a case of pancreaticobiliary actinomycosis.
Case Description/Methods: 50-year-old male with history of chronic pancreatitis complicated by biliary stricture requiring serial biliary stenting presented to the hospital with abdominal pain, decreased appetite, weight loss, and low-grade fevers. On exam the patient was hemodynamically stable and had mild epigastric abdominal tenderness. Labs revealed a lipase of 105 U/L, AST 20 U/L, ALT 18 U/L and total bilirubin of 0.7 mg/dL. Cross sectional imaging (CT scan) of the abdomen demonstrated a liver and pancreatic head mass at an outside institution two weeks prior to admission. Magnetic resonance cholangiopancreatography (MRCP) demonstrated dilated intrahepatic biliary ducts, bile duct of 11 mm with a stent in place, and intraluminal filling defects consistent of choledocholithiasis. Pancreatic head and body appeared bulky and heterogenous, whereas the pancreatic tail was atrophic. No focal liver lesions were seen. The patient underwent an endoscopic ultrasound which revealed calcific pancreatitis without solid masses. Endoscopic retrograde cholangiopancreatography (ERCP) was performed and the biliary stent was removed and sent for cytology. Cytology was negative for malignancy, however bacterial colonies consistent with actinomyces were found. Infectious disease service recommended the patient complete six weeks of ceftriaxone. After completion of treatment, his appetite returned, weight loss improved, and fevers resolved. Amoxicillin followed as maintenance therapy for approximately twelve months.
Discussion: The symptoms of pancreaticobiliary actinomycosis are non-specific, making the diagnosis difficult. Actinomycosis should be included in the differential diagnosis when a pancreatic or liver mass is found, especially in a patient with a history of pancreatic or biliary stenting. In these patients, we suspect that the repeat cannulation of the bile duct during an ERCP may lead to mucosal disruption, allowing bacteria to infect the tissue. It is important for endoscopists to consider actinomycosis and pursue histopathological confirmation to prevent unnecessary surgical intervention.
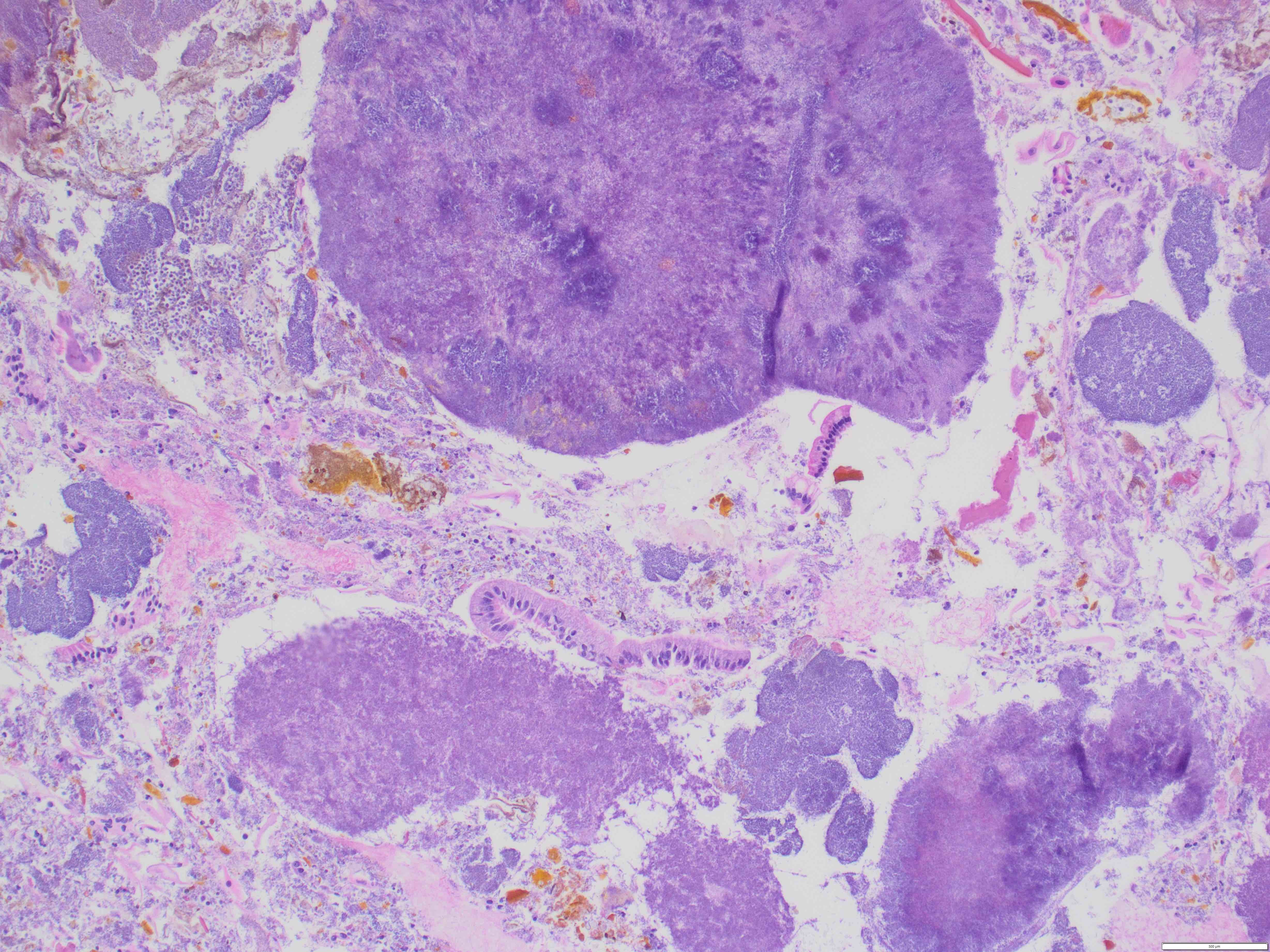
Figure: Cell block preparation of bile duct brushing (H&E stain, 100x) showing benign-appearing columnar/ductal epithelium with filamentous bacterial colonies, consistent with Actinomyces.
Disclosures:
Sylvia Keiser indicated no relevant financial relationships.
Laura Rosenkranz indicated no relevant financial relationships.
Sylvia Keiser, DO, Laura Rosenkranz, MD. B0029 - A Case of Pancreaticobiliary Actinomycosis Mimicking a Mass, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

