Back

Poster Session B - Monday Morning
Category: GI Bleeding
B0321 - Hematochezia and a Messy Malignant Melanoma
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Sylvia Keiser, DO
University of Texas Health San Antonio
San Antonio, TX
Presenting Author(s)
Sylvia Keiser, DO, Juan Echavarria, MS, MD
University of Texas Health San Antonio, San Antonio, TX
Introduction: Lower gastrointestinal bleeding is a common complaint amongst patients seen in the outpatient setting and carries a wide differential diagnosis. This ranges from benign conditions such as hemorrhoids, angioectasia, diverticulosis, anal fissures, etc., to serious, life-threatening conditions including malignancy. We present a unique case of rectal bleeding caused by anorectal melanoma.
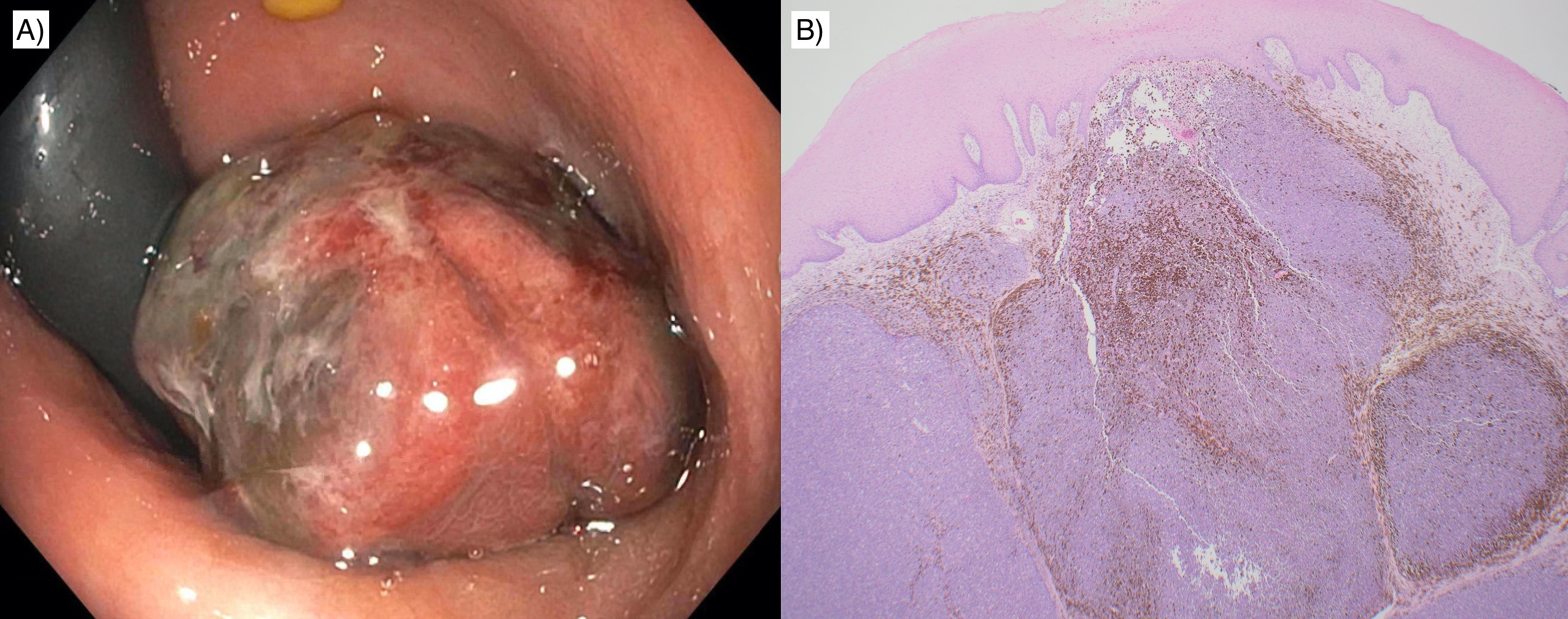
Case Description/Methods: A 50-year-old Hispanic female with history of hypertension presented to her primary care physician for rectal bleeding. She endorsed two months of constipation, decreased caliber of stools, and intermittent hematochezia. Her physical exam revealed a rectal prolapsing mass, and laboratory results revealed a hemoglobin of 12.3 g/dL, unchanged from prior. Due to these findings, she was referred to gastroenterology for evaluation. The patient underwent a colonoscopy which demonstrated a large, non-circumferential, three centimeter, partially obstructing mass in the rectum. The mass appeared to originate from the dentate line. No bleeding was present, however the mass appeared vascular in nature with dark purple areas, suggestive of a large thrombosed hemorrhoid. She was referred to the advanced endoscopists for an endoscopic ultrasound, which showed a hyperechoic mass with internal hypoechoic regions suggestive of necrosis. The endosonographic borders were well defined and the mass appeared confined to the mucosa. Biopsies were obtained and histopathology demonstrated atypical cells with prominent nucleoli and melanin pigment. The cells were positive for MART-1 and SOX10, confirming the diagnosis of malignant melanoma. A CT of the chest, abdomen, and pelvis was negative for lymphadenopathy or metastatic disease. She was referred to colorectal surgery and underwent local excision.
Discussion: Melanoma can arise from the mucosal epithelium of the respiratory, gastrointestinal, or genitourinary tracts in addition to the skin. Mucosal melanoma accounts for approximately 1.3% of all melanoma and usually carries a worse prognosis. Anorectal melanoma accounts for 1% of all anal canal malignancies. Symptoms can include rectal bleeding, anal pain, and change in bowel habits. The diagnosis is often missed as the signs and symptoms can be mistaken for hemorrhoids or polyps. Anorectal melanoma can even appear amelanotic, making the diagnosis more difficult. It is important for endoscopists to consider anorectal melanoma as a diagnosis as early detection and treatment is associated with improved prognosis.
Disclosures:
Sylvia Keiser, DO, Juan Echavarria, MS, MD. B0321 - Hematochezia and a Messy Malignant Melanoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Texas Health San Antonio, San Antonio, TX
Introduction: Lower gastrointestinal bleeding is a common complaint amongst patients seen in the outpatient setting and carries a wide differential diagnosis. This ranges from benign conditions such as hemorrhoids, angioectasia, diverticulosis, anal fissures, etc., to serious, life-threatening conditions including malignancy. We present a unique case of rectal bleeding caused by anorectal melanoma.
Case Description/Methods: A 50-year-old Hispanic female with history of hypertension presented to her primary care physician for rectal bleeding. She endorsed two months of constipation, decreased caliber of stools, and intermittent hematochezia. Her physical exam revealed a rectal prolapsing mass, and laboratory results revealed a hemoglobin of 12.3 g/dL, unchanged from prior. Due to these findings, she was referred to gastroenterology for evaluation. The patient underwent a colonoscopy which demonstrated a large, non-circumferential, three centimeter, partially obstructing mass in the rectum. The mass appeared to originate from the dentate line. No bleeding was present, however the mass appeared vascular in nature with dark purple areas, suggestive of a large thrombosed hemorrhoid. She was referred to the advanced endoscopists for an endoscopic ultrasound, which showed a hyperechoic mass with internal hypoechoic regions suggestive of necrosis. The endosonographic borders were well defined and the mass appeared confined to the mucosa. Biopsies were obtained and histopathology demonstrated atypical cells with prominent nucleoli and melanin pigment. The cells were positive for MART-1 and SOX10, confirming the diagnosis of malignant melanoma. A CT of the chest, abdomen, and pelvis was negative for lymphadenopathy or metastatic disease. She was referred to colorectal surgery and underwent local excision.
Discussion: Melanoma can arise from the mucosal epithelium of the respiratory, gastrointestinal, or genitourinary tracts in addition to the skin. Mucosal melanoma accounts for approximately 1.3% of all melanoma and usually carries a worse prognosis. Anorectal melanoma accounts for 1% of all anal canal malignancies. Symptoms can include rectal bleeding, anal pain, and change in bowel habits. The diagnosis is often missed as the signs and symptoms can be mistaken for hemorrhoids or polyps. Anorectal melanoma can even appear amelanotic, making the diagnosis more difficult. It is important for endoscopists to consider anorectal melanoma as a diagnosis as early detection and treatment is associated with improved prognosis.
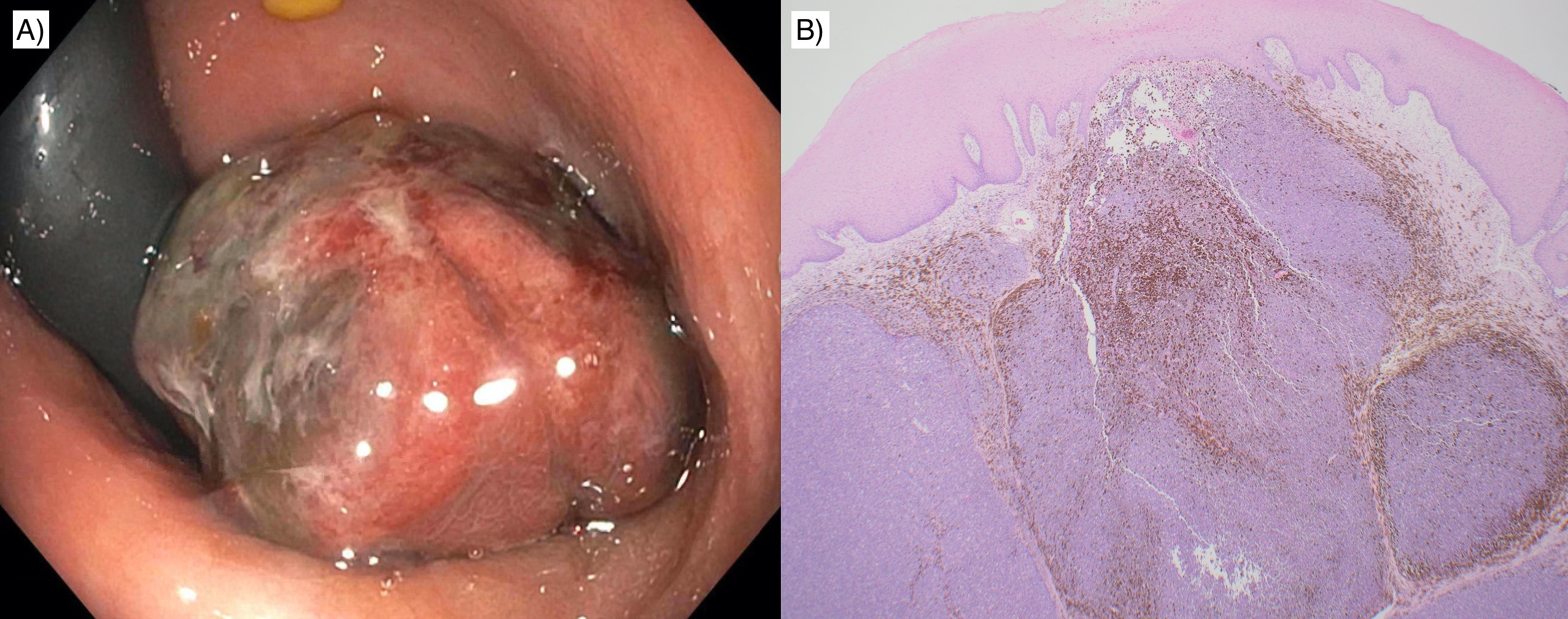
Figure: A) Large rectal mass visualized during colonoscopy
B) Tumor with melanin pigment undermining squamous mucosa (H&E, 20x)
B) Tumor with melanin pigment undermining squamous mucosa (H&E, 20x)
Disclosures:
Sylvia Keiser indicated no relevant financial relationships.
Juan Echavarria indicated no relevant financial relationships.
Sylvia Keiser, DO, Juan Echavarria, MS, MD. B0321 - Hematochezia and a Messy Malignant Melanoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
