Back

Poster Session D - Tuesday Morning
Category: Esophagus
D0255 - Managing Complications Following Endoscopic Myotomy as a Treatment for Upper Esophageal Sphincter Achalasia: A Case Report
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Pierce L. Claassen, BS
Washington State University Elson S. Floyd College of Medicine
Clarkston, WA
Presenting Author(s)
Pierce L. Claassen, BS1, Connor J. Eggleston, BS2, Nicolas A. Villa, MD3
1Washington State University Elson S. Floyd College of Medicine, Clarkston, WA; 2Creighton University School of Medicine, Omaha, NE; 3Washington State University Elson S. Floyd College of Medicine, MultiCare Valley Hospital, Spokane Valley, WA
Introduction: Achalasia is a chronic gastrointestinal disorder characterized by increased esophageal sphincter tone that is initially asymptomatic but eventually causes dysphagia. While this condition usually affects the lower esophageal sphincter, we present a rare case of upper esophageal sphincter (UES) achalasia of unknown etiology in a female in her sixth decade of life. The patient underwent a UES endoscopic myotomy by otorhinolaryngology that was complicated by perforation and subsequent severe esophageal stenosis. Consequently, she was referred to an advanced endoscopy-trained gastroenterologist (GI) for further evaluation. She was treated over the course of three months with six endoscopic dilatations and glucocorticoid injections. Few cases of idiopathic UES achalasia have been described to date.
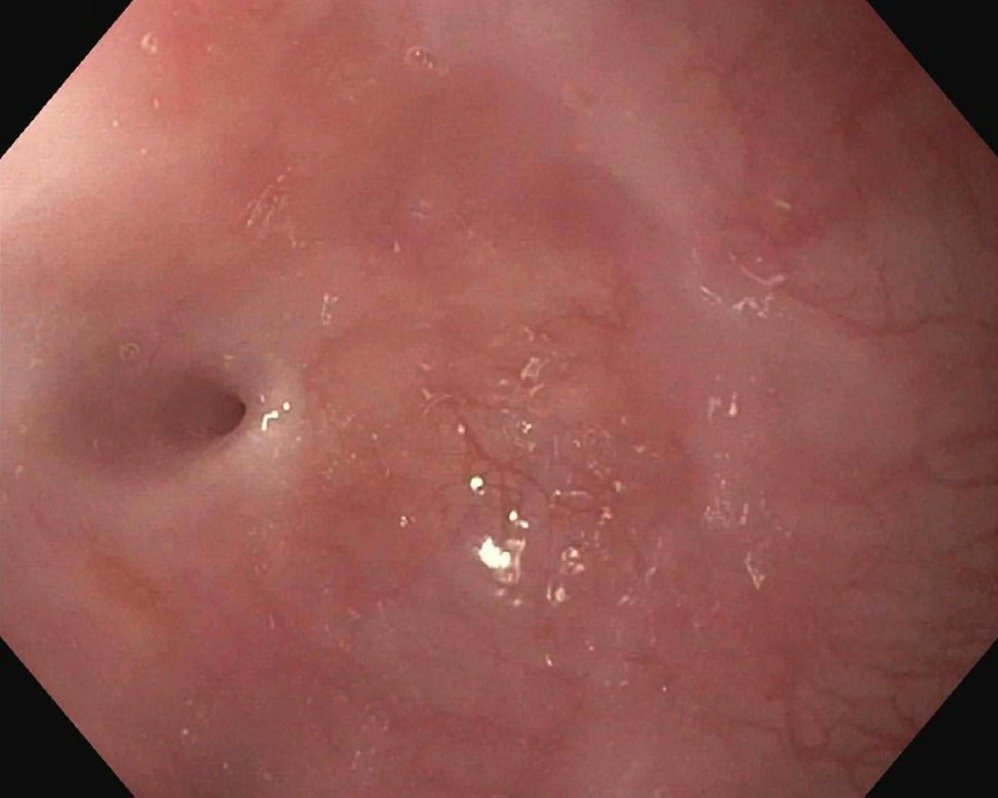
Case Description/Methods: Upon presentation, the patient was profoundly dysphagic to solids and liquids, noting a 50-pound weight loss in the past two months since the UES endoscopic myotomy. During the first esophagogastroduodenoscopy (EGD), the esophagus was found to be severely stenotic (15cm distal to the upper incisors at the level of the UES) reducing the lumen to 2mm in diameter at its narrowest point. Under fluoroscopic guidance, a guidewire was passed through the UES, and a 6mm balloon biliary dilator was inflated. A 24 French Savary dilator was then passed, successfully enlarging the lumen to 8mm without perforation. Due to the patient’s poor nutrition status and necessity of additional dilations, she was referred to interventional radiology for percutaneous endogastric (PEG) tube placement.
During subsequent EGDs, through-the-scope balloon and Savary dilators were used to increase the luminal diameter to a desirable size of 20mm. Local triamcinolone injections (2mL at 40mg/mL) were administered at the level of the UES during each EGD to reduce this risk of fibrosis and consequential stricture formation. After the sixth and final dilation, the patient was non-dysphagic, so the PEG tube was removed. She was instructed to resume her usual diet and contact GI as needed.
Discussion: This case of idiopathic UES achalasia represents an uncommon cause of severe dysphagia in an otherwise healthy adult without a history of stroke, radiation therapy, or a known congenital predisposition for pharyngoesophageal dysfunction. Complications following UES endoscopic myotomy must be diagnosed and treated urgently, as esophageal stenosis can increase the risk of aspiration and cause profound weight loss.
Disclosures:
Pierce L. Claassen, BS1, Connor J. Eggleston, BS2, Nicolas A. Villa, MD3. D0255 - Managing Complications Following Endoscopic Myotomy as a Treatment for Upper Esophageal Sphincter Achalasia: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Washington State University Elson S. Floyd College of Medicine, Clarkston, WA; 2Creighton University School of Medicine, Omaha, NE; 3Washington State University Elson S. Floyd College of Medicine, MultiCare Valley Hospital, Spokane Valley, WA
Introduction: Achalasia is a chronic gastrointestinal disorder characterized by increased esophageal sphincter tone that is initially asymptomatic but eventually causes dysphagia. While this condition usually affects the lower esophageal sphincter, we present a rare case of upper esophageal sphincter (UES) achalasia of unknown etiology in a female in her sixth decade of life. The patient underwent a UES endoscopic myotomy by otorhinolaryngology that was complicated by perforation and subsequent severe esophageal stenosis. Consequently, she was referred to an advanced endoscopy-trained gastroenterologist (GI) for further evaluation. She was treated over the course of three months with six endoscopic dilatations and glucocorticoid injections. Few cases of idiopathic UES achalasia have been described to date.
Case Description/Methods: Upon presentation, the patient was profoundly dysphagic to solids and liquids, noting a 50-pound weight loss in the past two months since the UES endoscopic myotomy. During the first esophagogastroduodenoscopy (EGD), the esophagus was found to be severely stenotic (15cm distal to the upper incisors at the level of the UES) reducing the lumen to 2mm in diameter at its narrowest point. Under fluoroscopic guidance, a guidewire was passed through the UES, and a 6mm balloon biliary dilator was inflated. A 24 French Savary dilator was then passed, successfully enlarging the lumen to 8mm without perforation. Due to the patient’s poor nutrition status and necessity of additional dilations, she was referred to interventional radiology for percutaneous endogastric (PEG) tube placement.
During subsequent EGDs, through-the-scope balloon and Savary dilators were used to increase the luminal diameter to a desirable size of 20mm. Local triamcinolone injections (2mL at 40mg/mL) were administered at the level of the UES during each EGD to reduce this risk of fibrosis and consequential stricture formation. After the sixth and final dilation, the patient was non-dysphagic, so the PEG tube was removed. She was instructed to resume her usual diet and contact GI as needed.
Discussion: This case of idiopathic UES achalasia represents an uncommon cause of severe dysphagia in an otherwise healthy adult without a history of stroke, radiation therapy, or a known congenital predisposition for pharyngoesophageal dysfunction. Complications following UES endoscopic myotomy must be diagnosed and treated urgently, as esophageal stenosis can increase the risk of aspiration and cause profound weight loss.
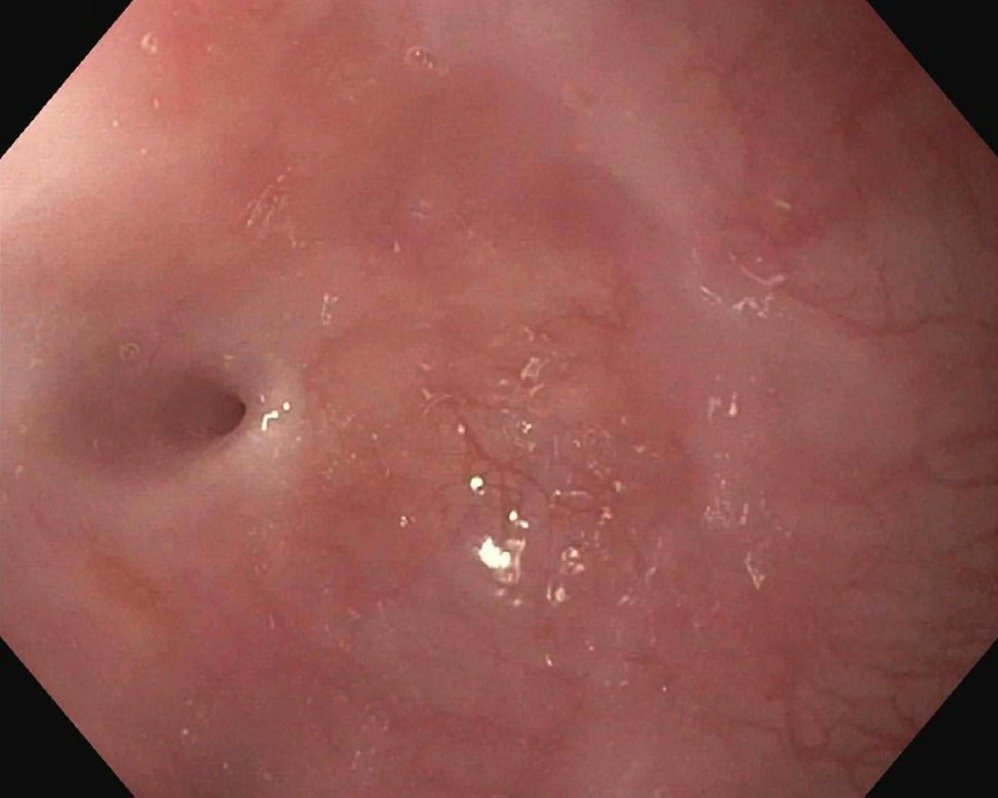
Figure: Anterograde view of the esophageal lumen proximal to the upper esophageal sphincter. Circumferential constriction at 15cm distal to the upper incisors reduced the luminal diameter to 2mm at the narrowest point. The image was taken with an esophagogastroduodenoscope during the patient’s first visit to the advanced endoscopy gastroenterology clinic.
Disclosures:
Pierce Claassen indicated no relevant financial relationships.
Connor Eggleston indicated no relevant financial relationships.
Nicolas Villa indicated no relevant financial relationships.
Pierce L. Claassen, BS1, Connor J. Eggleston, BS2, Nicolas A. Villa, MD3. D0255 - Managing Complications Following Endoscopic Myotomy as a Treatment for Upper Esophageal Sphincter Achalasia: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.

