Back


Poster Session B - Monday Morning
Category: Colon
B0123 - Idiopathic AA Amyloidosis Presenting With Rectal Involvement and Intractable Hematochezia
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom

Has Audio
.jpg)
Gurasees S. Chawla, MD
Montefiore Medical Center
Bronx, NY
Presenting Author(s)
Gurasees S. Chawla, MD, Nicholas Forelli, BS, Pooja Kothari, MD, Lawrence Brandt, MD, MACG
Montefiore Medical Center, Bronx, NY
Introduction: Amyloidosis is a group of complex diseases caused by the misfolding, aggregation, and deposition of proteins as insoluble fibrils within tissues leading to progressive organ damage. Secondary amyloidosis is often associated with chronic inflammatory diseases and affects the GI tract in an estimated 60% of cases. The vast majority involve the upper GI tract, especially the duodenum, with only a small subset affecting the colon or rectum.
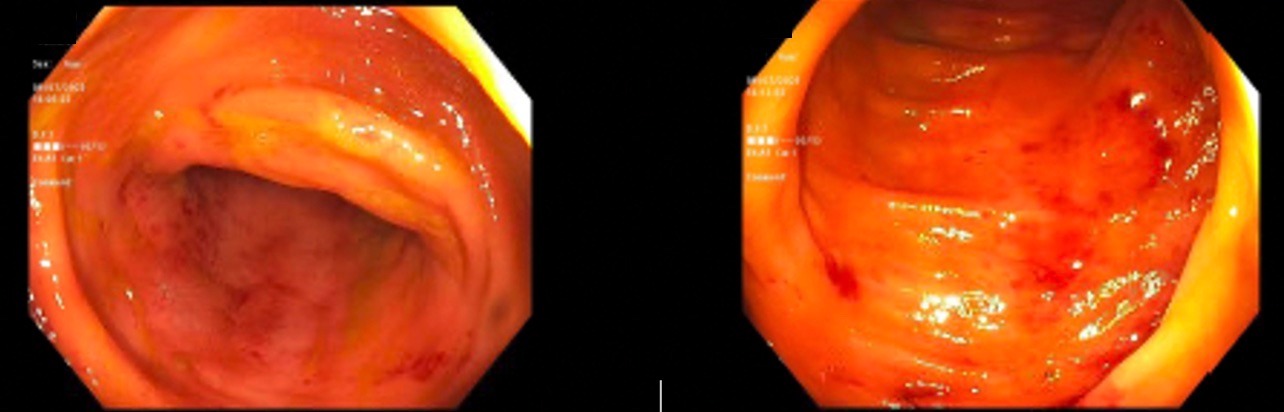
Case Description/Methods: A 47-year-old man with PMH of ESRD on HD and HTN presented with several episodes of hematochezia for the past 1 day. His abdomen was diffusely tender. Laboratory findings revealed a hemoglobin of 7.6 g/dL and a leukocyte count of 14.9 k/uL. Patient had several previous admissions over the past two years for hematochezia with no clear etiologies found with multiple unremarkable EGD and colonoscopies. Rheumatology was consulted given concern for an underlying autoimmune process. Serology was negative for RF, ANA, dsDNA, RNP, SSA/SSB, SCL-70, JO-1, Smith, TPO, CCP, and Centromere antibody. Colonoscopy revealed erythematous mucosa throughout the length of the colon. Biopsies taken from the duodenum, ileum, right and left colon, and the rectum revealed deposition of amorphous eosinophilic consistent with amyloid. Specimens analyzed LM-MS detected peptide fragments consistent with AA amyloidosis. The ileum, jejunum, transverse and descending colon had preserved architecture without signs of amyloid deposition. Of note, upper GI endoscopy from the year prior showed no signs of disease, suggesting a rapid progression of amyloidosis throughout the GI tract.
Discussion: The clinical manifestations of secondary amyloidosis vary depending on the organs affected. Involvement of the GI tract is more common in AL amyloidosis than in AA amyloidosis, and both diseases preferentially affect the upper GI tract, most commonly the duodenum. GI amyloidosis often presents with non-specific clinical findings such as diarrhea, obstruction, malabsorption, bleeding, erosion, or ischemia, and may represent a significant clinical challenge in its differentiation from other intestinal diseases such as IBD or malignancy. Although uncommon, GI manifestations of amyloidosis should be considered as a differential for patients in which standard therapies for intestinal disorders have not yielded clinical improvement.
Disclosures:
Gurasees S. Chawla, MD, Nicholas Forelli, BS, Pooja Kothari, MD, Lawrence Brandt, MD, MACG. B0123 - Idiopathic AA Amyloidosis Presenting With Rectal Involvement and Intractable Hematochezia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
Montefiore Medical Center, Bronx, NY
Introduction: Amyloidosis is a group of complex diseases caused by the misfolding, aggregation, and deposition of proteins as insoluble fibrils within tissues leading to progressive organ damage. Secondary amyloidosis is often associated with chronic inflammatory diseases and affects the GI tract in an estimated 60% of cases. The vast majority involve the upper GI tract, especially the duodenum, with only a small subset affecting the colon or rectum.
Case Description/Methods: A 47-year-old man with PMH of ESRD on HD and HTN presented with several episodes of hematochezia for the past 1 day. His abdomen was diffusely tender. Laboratory findings revealed a hemoglobin of 7.6 g/dL and a leukocyte count of 14.9 k/uL. Patient had several previous admissions over the past two years for hematochezia with no clear etiologies found with multiple unremarkable EGD and colonoscopies. Rheumatology was consulted given concern for an underlying autoimmune process. Serology was negative for RF, ANA, dsDNA, RNP, SSA/SSB, SCL-70, JO-1, Smith, TPO, CCP, and Centromere antibody. Colonoscopy revealed erythematous mucosa throughout the length of the colon. Biopsies taken from the duodenum, ileum, right and left colon, and the rectum revealed deposition of amorphous eosinophilic consistent with amyloid. Specimens analyzed LM-MS detected peptide fragments consistent with AA amyloidosis. The ileum, jejunum, transverse and descending colon had preserved architecture without signs of amyloid deposition. Of note, upper GI endoscopy from the year prior showed no signs of disease, suggesting a rapid progression of amyloidosis throughout the GI tract.
Discussion: The clinical manifestations of secondary amyloidosis vary depending on the organs affected. Involvement of the GI tract is more common in AL amyloidosis than in AA amyloidosis, and both diseases preferentially affect the upper GI tract, most commonly the duodenum. GI amyloidosis often presents with non-specific clinical findings such as diarrhea, obstruction, malabsorption, bleeding, erosion, or ischemia, and may represent a significant clinical challenge in its differentiation from other intestinal diseases such as IBD or malignancy. Although uncommon, GI manifestations of amyloidosis should be considered as a differential for patients in which standard therapies for intestinal disorders have not yielded clinical improvement.
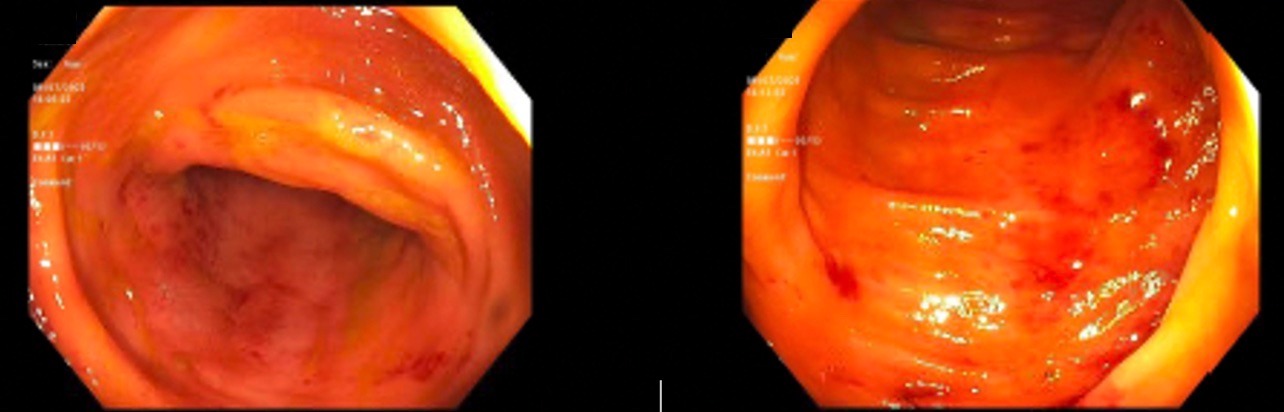
Figure: Rectum (left) and rectosigmoid junction (right) with friable mucosa.
Disclosures:
Gurasees Chawla indicated no relevant financial relationships.
Nicholas Forelli indicated no relevant financial relationships.
Pooja Kothari indicated no relevant financial relationships.
Lawrence Brandt indicated no relevant financial relationships.
Gurasees S. Chawla, MD, Nicholas Forelli, BS, Pooja Kothari, MD, Lawrence Brandt, MD, MACG. B0123 - Idiopathic AA Amyloidosis Presenting With Rectal Involvement and Intractable Hematochezia, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
