Back

Poster Session D - Tuesday Morning
Category: Colon
D0133 - Persistent Abdominal Pain Linked to Tuberculous Colitis
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Scott Fraser, MD
IUSM Southwest Indiana Internal Medicine Residency
Vincennes, IN
Presenting Author(s)
Scott Fraser, MD1, Kengo Soghoyan, MBBCh,1, Jared Micho, MD2, Michael Rusche, MD3
1IUSM Southwest Indiana Internal Medicine Residency, Vincennes, IN; 2IUSM Southwest Indiana Internal Medicine Residency, Evansville, IN; 3Digestive Care Center, Evansville, IN
Introduction: Tuberculous colitis is a rare form of tuberculosis (TB) and often presents with non-specific gastrointestinal (GI) complaints. Roughly 2% of TB cases are related to the GI tract. Diagnosis is challenging as its non-specific presentation mimics other GI disease processes. This case report highlights how a thorough patient history and work-up are crucial for timely diagnosis and treatment of TB colitis.
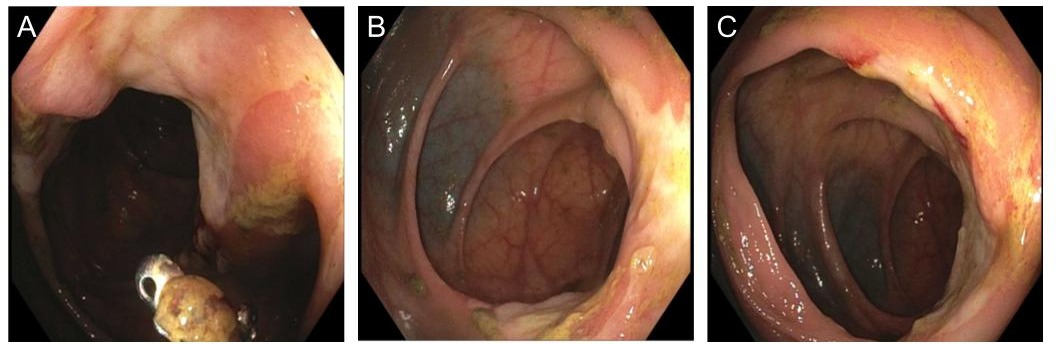
Case Description/Methods: A 70-year-old male with a history of missionary work in Haiti presented to our clinic with abdominal pain and iron deficiency anemia (IDA). His abdominal pain was right-sided, non-radiating, with associated night sweats and a 25-pound weight loss. While in Haiti, he was exposed to TB but purified protein derivative skin testing was negative at that time. Laboratory values were significant for IDA and elevated ESR. Upper and lower endoscopies were notable for deep ulcerations at the ileocecal valve and hepatic flexure, as well as severe terminal ileum stenosis. Biopsies revealed granulomatous inflammation without crypt architectural distortion. A computed tomography scan of the abdomen revealed colonic thickening extending to the splenic flexure. Repeat colonoscopy revealed deep ulcerations at the hepatic flexure and biopsies demonstrated non-specific inflammation. Samples sent for acid fast bacilli and culture reported growth on the AFB medium, but due to bacterial contamination, a final identification was unobtainable. He was referred to infectious disease and began a four-drug regimen for Mycobacterium tuberculosis. However, due to persistent symptoms, he was referred to general surgery and underwent right hemicolectomy. Following surgery, he had improvement in symptoms.
Discussion: Tuberculous colitis is a rare form of TB and often presents with non-specific GI complaints. There are no clear diagnostic algorithms, although biopsy is one of the first recommended interventions. Other reports suggest monitoring CD4 counts and polymerase chain reaction—both require validation. Due to its generalized presentation, TB colitis can be mistaken for inflammatory bowel disease, as seen in our patient with ileocecal involvement. Our case is unique in that symptoms persisted and the disease progressed, despite antituberculin therapy. Studies report resolution of TB colitis following secondary rescue regimen; however, our patient’s disease process was more extensive. As with our patient, if antituberculin therapy is ineffective, surgery may be the only definitive therapy.
Disclosures:
Scott Fraser, MD1, Kengo Soghoyan, MBBCh,1, Jared Micho, MD2, Michael Rusche, MD3. D0133 - Persistent Abdominal Pain Linked to Tuberculous Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1IUSM Southwest Indiana Internal Medicine Residency, Vincennes, IN; 2IUSM Southwest Indiana Internal Medicine Residency, Evansville, IN; 3Digestive Care Center, Evansville, IN
Introduction: Tuberculous colitis is a rare form of tuberculosis (TB) and often presents with non-specific gastrointestinal (GI) complaints. Roughly 2% of TB cases are related to the GI tract. Diagnosis is challenging as its non-specific presentation mimics other GI disease processes. This case report highlights how a thorough patient history and work-up are crucial for timely diagnosis and treatment of TB colitis.
Case Description/Methods: A 70-year-old male with a history of missionary work in Haiti presented to our clinic with abdominal pain and iron deficiency anemia (IDA). His abdominal pain was right-sided, non-radiating, with associated night sweats and a 25-pound weight loss. While in Haiti, he was exposed to TB but purified protein derivative skin testing was negative at that time. Laboratory values were significant for IDA and elevated ESR. Upper and lower endoscopies were notable for deep ulcerations at the ileocecal valve and hepatic flexure, as well as severe terminal ileum stenosis. Biopsies revealed granulomatous inflammation without crypt architectural distortion. A computed tomography scan of the abdomen revealed colonic thickening extending to the splenic flexure. Repeat colonoscopy revealed deep ulcerations at the hepatic flexure and biopsies demonstrated non-specific inflammation. Samples sent for acid fast bacilli and culture reported growth on the AFB medium, but due to bacterial contamination, a final identification was unobtainable. He was referred to infectious disease and began a four-drug regimen for Mycobacterium tuberculosis. However, due to persistent symptoms, he was referred to general surgery and underwent right hemicolectomy. Following surgery, he had improvement in symptoms.
Discussion: Tuberculous colitis is a rare form of TB and often presents with non-specific GI complaints. There are no clear diagnostic algorithms, although biopsy is one of the first recommended interventions. Other reports suggest monitoring CD4 counts and polymerase chain reaction—both require validation. Due to its generalized presentation, TB colitis can be mistaken for inflammatory bowel disease, as seen in our patient with ileocecal involvement. Our case is unique in that symptoms persisted and the disease progressed, despite antituberculin therapy. Studies report resolution of TB colitis following secondary rescue regimen; however, our patient’s disease process was more extensive. As with our patient, if antituberculin therapy is ineffective, surgery may be the only definitive therapy.
Figure: Figure 1.
A & B) Lesion with inflammation prior to biopsy.
C) Lesion post-biopsy.
A & B) Lesion with inflammation prior to biopsy.
C) Lesion post-biopsy.
Disclosures:
Scott Fraser indicated no relevant financial relationships.
Kengo Soghoyan indicated no relevant financial relationships.
Jared Micho indicated no relevant financial relationships.
Michael Rusche indicated no relevant financial relationships.
Scott Fraser, MD1, Kengo Soghoyan, MBBCh,1, Jared Micho, MD2, Michael Rusche, MD3. D0133 - Persistent Abdominal Pain Linked to Tuberculous Colitis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
