Back

Poster Session B - Monday Morning
Category: IBD
B0419 - Merging the Evidence and the Art: Diagnosing Crohn’s Disease From Pyoderma Gangrenosum
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Saeed Graham, MD
East Carolina University Brody School of Medicine
Greenville, NC
Presenting Author(s)
Saeed Graham, MD1, Mary-Jane Williams, MD2, Danielle Hoo-Fatt, MD3
1East Carolina University Brody School of Medicine, Greenville, NC; 2East Carolina University/Vidant Medical Center, Greenville, NC; 3Brody School of Medicine at East Carolina University, Greenville, NC
Introduction: The dermatologic exam is essential in evaluating cases of suspected inflammatory bowel disease (IBD). Pyoderma gangrenosum (PG) is a potential cutaneous finding, characterized by dermal neutrophilic inflammation; classically presenting as skin ulceration. When encountered before an established diagnosis of IBD, the finding may be mistaken for other causes of ulceration such as vascular insufficiency, diabetic foot ulcer, cancer etc. We detail an 8th decade patient with no prior history of IBD who presented with a large leg ulcer and new onset bloody stools, later diagnosed with Crohn’s disease.
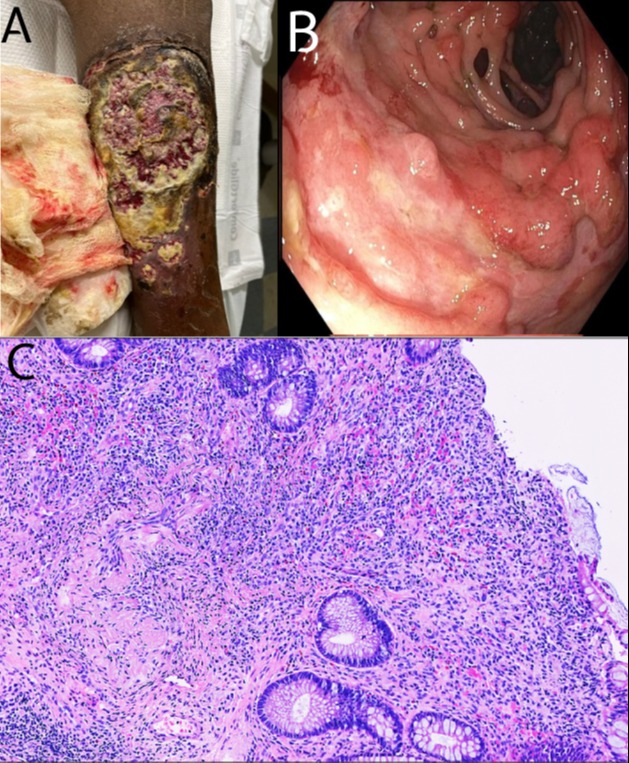
Case Description/Methods: A 73 year old African American male with history of diabetes mellitus and hypertension presented with painful ulcerative leg lesions, noted initially as a “scab” with rapid 2 week progression to that shown (fig 1-A). Additional history was pertinent for intermittent bloody stools of similar duration. He denied past similar symptoms and review of systems was otherwise negative. Serology was notable for severe iron deficiency anemia with hemoglobin of 2.7 g/dl, MCV of 69.2 fL, iron of 16 ug/dL and transferrin saturation of 6%. After 4-units blood transfusion and empiric IV antibiotics, the admitting service requested consults for endoscopic evaluation and skin biopsy. Colonic mucosa was notable for multiple ulcers and skip lesions throughout the colon, sparing the rectum (fig 1-B). Pathology report of colonic biopsy samples noted chronic inflammatory changes consistent with Crohn’s colitis (fig 1-C). Peripheral leg lesion biopsy showed perivascular lymphocytic infiltrate. Ultimately patient was discharged with gastroenterology follow-up and scheduled re-biopsy.
Discussion:PG is a rare skin finding which may be seen in IBD. The classic variant displays salient ulceration, often of the lower extremities. This patient was advanced in age, and his only gastrointestinal complaint was that of bloody stools — features for what would be diagnosed as Crohn’s. His ulcer may have erroneously been attributed to diabetes or vascular disease and anemia to causes other than IBD. The rapidity of lesion development, well-defined appearance and violaceous borders were consistent with PG. Although histologically defined by neutrophilic infiltration, peripheral biopsy tends to show chronic inflammatory infiltrate with features suggestive of vasculitis as was the case in our patient. Physicians should maintain suspicion for IBD despite few colitis symptoms in patients with ulcerative skin lesions.
1East Carolina University Brody School of Medicine, Greenville, NC; 2East Carolina University/Vidant Medical Center, Greenville, NC; 3Brody School of Medicine at East Carolina University, Greenville, NC
Introduction: The dermatologic exam is essential in evaluating cases of suspected inflammatory bowel disease (IBD). Pyoderma gangrenosum (PG) is a potential cutaneous finding, characterized by dermal neutrophilic inflammation; classically presenting as skin ulceration. When encountered before an established diagnosis of IBD, the finding may be mistaken for other causes of ulceration such as vascular insufficiency, diabetic foot ulcer, cancer etc. We detail an 8th decade patient with no prior history of IBD who presented with a large leg ulcer and new onset bloody stools, later diagnosed with Crohn’s disease.
Case Description/Methods: A 73 year old African American male with history of diabetes mellitus and hypertension presented with painful ulcerative leg lesions, noted initially as a “scab” with rapid 2 week progression to that shown (fig 1-A). Additional history was pertinent for intermittent bloody stools of similar duration. He denied past similar symptoms and review of systems was otherwise negative. Serology was notable for severe iron deficiency anemia with hemoglobin of 2.7 g/dl, MCV of 69.2 fL, iron of 16 ug/dL and transferrin saturation of 6%. After 4-units blood transfusion and empiric IV antibiotics, the admitting service requested consults for endoscopic evaluation and skin biopsy. Colonic mucosa was notable for multiple ulcers and skip lesions throughout the colon, sparing the rectum (fig 1-B). Pathology report of colonic biopsy samples noted chronic inflammatory changes consistent with Crohn’s colitis (fig 1-C). Peripheral leg lesion biopsy showed perivascular lymphocytic infiltrate. Ultimately patient was discharged with gastroenterology follow-up and scheduled re-biopsy.
Discussion:
PG is a rare skin finding which may be seen in IBD. The classic variant displays salient ulceration, often of the lower extremities. This patient was advanced in age, and his only gastrointestinal complaint was that of bloody stools — features for what would be diagnosed as Crohn’s. His ulcer may have erroneously been attributed to diabetes or vascular disease and anemia to causes other than IBD. The rapidity of lesion development, well-defined appearance and violaceous borders were consistent with PG. Although histologically defined by neutrophilic infiltration, peripheral biopsy tends to show chronic inflammatory infiltrate with features suggestive of vasculitis as was the case in our patient. Physicians should maintain suspicion for IBD despite few colitis symptoms in patients with ulcerative skin lesions.
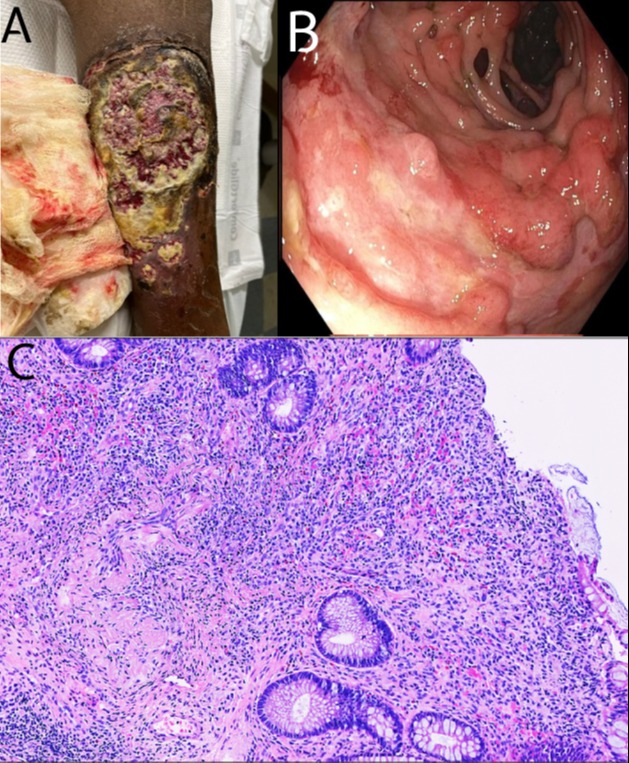
Figure: Fig 1 - A: left lower extremity demonstrating a large well-circumscribed central ulcerative lesion with violaceous border. Similar but smaller lesions seen inferiorly. B: Photograph taken during colonoscopy showing mucosal ulceration and inflammation of the ascending colon.
C: (x200) Photomicrograph of hematoxylin and eosin-stained section of the right colonic biopsy, showing inflamed granulation tissue with an ulcerative process, areas of lamina propria fibrosis, granulation tissue, mixed acute and chronic inflammation, and crypt architectural distortion
Disclosures:
Saeed Graham indicated no relevant financial relationships. Mary-Jane Williams indicated no relevant financial relationships. Danielle Hoo-Fatt indicated no relevant financial relationships.
Saeed Graham, MD1, Mary-Jane Williams, MD2, Danielle Hoo-Fatt, MD3. B0419 - Merging the Evidence and the Art: Diagnosing Crohn’s Disease From Pyoderma Gangrenosum, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
C: (x200) Photomicrograph of hematoxylin and eosin-stained section of the right colonic biopsy, showing inflamed granulation tissue with an ulcerative process, areas of lamina propria fibrosis, granulation tissue, mixed acute and chronic inflammation, and crypt architectural distortion
