Back

Poster Session D - Tuesday Morning
Category: General Endoscopy
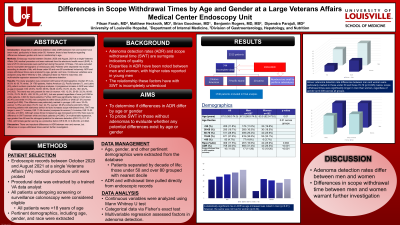
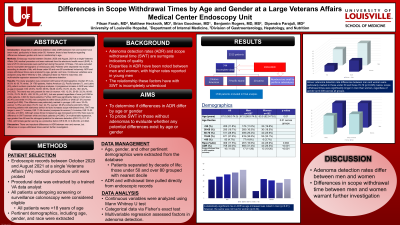
D0284 - Differences in Scope Withdrawal Times by Age and Gender at a Large Veterans Affairs Medical Center Endoscopy Unit
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- FF
Filsan Farah, MD
University of Louisville
Louisville, KY
Presenting Author(s)
Filsan Farah, MD1, Matthew Heckroth, MD2, Brian Goodman, DO1, Benjamin Rogers, MD1, Dipendra Parajuli, MD1
1University of Louisville, Louisville, KY; 2University of Louisville School of Medicine, Louisville, KY
Introduction: Disparities in adenoma detection rates (ADR) between men and women have been noted, particularly in those under 50. However, there is less literature regarding differences between gender and race in relationship to age.
Methods: Endoscopy records between October, 2020 and August, 2021 at a single Veterans Affairs (VA) medical procedure unit were retrieved from the electronic health record (EHR). A total of 2513 colonoscopies were performed during this period. Of these, 744 were excluded due to incomplete demographic or endoscopic data. Patients were separated into deciles according to decade of life, with those under 50 and over 80 considered inclusively. ADR and scope withdrawal times were analyzed by age, gender, and race. Continuous variables were analyzed using Mann Whitney U test, categorical data via Fisher’s exact test, and multivariable regression assessed factors in adenoma detection.
Results: The study population was consistent with typical VA demographics (median 67.0 yrs, 90.8% M, 80.7% white). Of 1769 patients, Native American (2), Pacific Islander (7), and Latino (20) patient numbers precluded subgroup analyses. A progressive increase in ADR was noted as age increased (< 50: 29.3%; 50-59: 36.9%; 60-69: 40.5%; 70-79: 43.4%; >80: 48.2%, p=0.002). This trend was only present for men (in women: < 50: 12.5%, 50-59: 33.3%; 60-69: 31.0%; 70-79: 26.9%, >80: 33.3%, p=0.341), but was present regardless of race (p=0.038 for white patients, 0.046 for black patients). Further, ADR was significantly higher in both black (43.4%) and white (41.0%) men compared to either black (28.6%) or white (27.0%) women overall (p=0.008). This difference was particularly marked in younger (< 50: men: 32.4%; women: 12.5%) and older (70-79: men: 44.7%; women: 26.9%) cohorts (p≤0.023). When removing patients with adenomas (which de facto increases scope withdrawal time), SWT was longer in men (17 minutes, IQR 11-26 minutes) compared to women (14 minutes, IQR 10-20 minutes, p< 0.001). Although scope times increased as age increased (p=0.018), there was no difference in SWT between white and black patients (p=0.990). On multivariable regression, age greater than 80 was the strongest predictor for adenoma detection (OR 2.15, CI 1.27-3.64), with female gender serving as a protective factor (OR 0.55, CI 0.38-0.80, p=0.002).
Discussion: There are important differences in ADR between men and women, but differences in scope withdrawal times warrant further investigation.
Disclosures:
Filsan Farah, MD1, Matthew Heckroth, MD2, Brian Goodman, DO1, Benjamin Rogers, MD1, Dipendra Parajuli, MD1. D0284 - Differences in Scope Withdrawal Times by Age and Gender at a Large Veterans Affairs Medical Center Endoscopy Unit, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Louisville, Louisville, KY; 2University of Louisville School of Medicine, Louisville, KY
Introduction: Disparities in adenoma detection rates (ADR) between men and women have been noted, particularly in those under 50. However, there is less literature regarding differences between gender and race in relationship to age.
Methods: Endoscopy records between October, 2020 and August, 2021 at a single Veterans Affairs (VA) medical procedure unit were retrieved from the electronic health record (EHR). A total of 2513 colonoscopies were performed during this period. Of these, 744 were excluded due to incomplete demographic or endoscopic data. Patients were separated into deciles according to decade of life, with those under 50 and over 80 considered inclusively. ADR and scope withdrawal times were analyzed by age, gender, and race. Continuous variables were analyzed using Mann Whitney U test, categorical data via Fisher’s exact test, and multivariable regression assessed factors in adenoma detection.
Results: The study population was consistent with typical VA demographics (median 67.0 yrs, 90.8% M, 80.7% white). Of 1769 patients, Native American (2), Pacific Islander (7), and Latino (20) patient numbers precluded subgroup analyses. A progressive increase in ADR was noted as age increased (< 50: 29.3%; 50-59: 36.9%; 60-69: 40.5%; 70-79: 43.4%; >80: 48.2%, p=0.002). This trend was only present for men (in women: < 50: 12.5%, 50-59: 33.3%; 60-69: 31.0%; 70-79: 26.9%, >80: 33.3%, p=0.341), but was present regardless of race (p=0.038 for white patients, 0.046 for black patients). Further, ADR was significantly higher in both black (43.4%) and white (41.0%) men compared to either black (28.6%) or white (27.0%) women overall (p=0.008). This difference was particularly marked in younger (< 50: men: 32.4%; women: 12.5%) and older (70-79: men: 44.7%; women: 26.9%) cohorts (p≤0.023). When removing patients with adenomas (which de facto increases scope withdrawal time), SWT was longer in men (17 minutes, IQR 11-26 minutes) compared to women (14 minutes, IQR 10-20 minutes, p< 0.001). Although scope times increased as age increased (p=0.018), there was no difference in SWT between white and black patients (p=0.990). On multivariable regression, age greater than 80 was the strongest predictor for adenoma detection (OR 2.15, CI 1.27-3.64), with female gender serving as a protective factor (OR 0.55, CI 0.38-0.80, p=0.002).
Discussion: There are important differences in ADR between men and women, but differences in scope withdrawal times warrant further investigation.
Disclosures:
Filsan Farah indicated no relevant financial relationships.
Matthew Heckroth indicated no relevant financial relationships.
Brian Goodman indicated no relevant financial relationships.
Benjamin Rogers indicated no relevant financial relationships.
Dipendra Parajuli indicated no relevant financial relationships.
Filsan Farah, MD1, Matthew Heckroth, MD2, Brian Goodman, DO1, Benjamin Rogers, MD1, Dipendra Parajuli, MD1. D0284 - Differences in Scope Withdrawal Times by Age and Gender at a Large Veterans Affairs Medical Center Endoscopy Unit, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
