Back

Poster Session D - Tuesday Morning
Category: General Endoscopy
D0288 - Mantle Cell Lymphoma Presenting as Multiple Lymphomatous Polyposis: A Case Report
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Sophia Pimpinelli, MD
Rutgers Robert Wood Johnson University Hospital
New Brunswick, New Jersey
Presenting Author(s)
Sophia Pimpinelli, MD1, Abhishek Bhurwal, MD2, Tae Yang Park, MD1, Mahmoud A. Ali, MBBCh2, Steven Brant, MD1, Anish Vinit Patel, MD2
1Rutgers Robert Wood Johnson University Hospital, New Brunswick, NJ; 2Rutgers Robert Wood Johnson University Hospital- New Brunswick, New Brunswick, NJ
Introduction: Mantle Cell Lymphoma (MCL) typically presents with extensive lymphadenopathy, fevers, night sweats and unintentional weight loss. However, Multiple Lymphomatous Polyposis (MLP), MCL arising from the gastrointestinal tract, is an aggressive malignancy and is infrequently described.
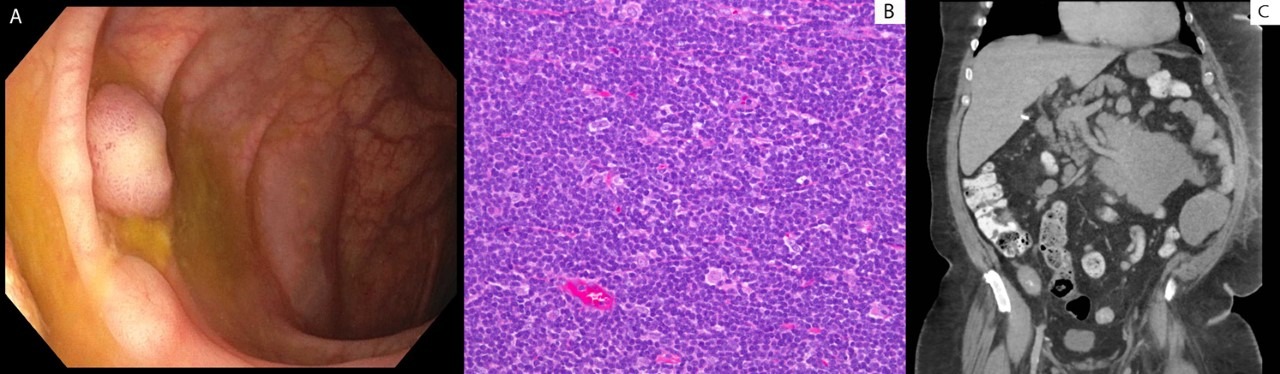
Case Description/Methods: A 68-year-old Caucasian man with atrial fibrillation and hypertension presented to the hospital with watery diarrhea, fatigue and intermittent epigastric pain for the past several weeks. He denied melena, hematochezia, heartburn, dysphagia, odynophagia, weight loss, loss of appetite, NSAID use, recent travel or sick contacts. There was no family history of gastrointestinal malignancy. No history of prior endoscopic evaluation. Physical exam was notable for brown stool on rectal exam. Further evaluation revealed Hgb 6.4, MCV 60.9, iron 43, TIBC 442 and iron saturation 10% consistent with iron deficiency anemia. Upper endoscopy was normal. Colonoscopy showed eight 6-16 mm polyps scattered throughout the colon, all of which were resected completely. Analysis showed a range of histology – 3 tubular adenomas, 1 serrated and 2 hyperplastic polyps. However, histology of 4 polypoid appearing lesions (Fig 1A) showed prominent nodular atypical submucosal lymphoid aggregates (Fig 1B) that were positive for CD20, cyclin D1, weak CD5, and negative for CD10 and CD23. This was consistent with the diagnosis of MCL. CT imaging showed diffuse lymphadenopathy, including bulky disease with a 16.6 x 10.6 cm small bowel mesenteric mass (Fig 1C), along with proximal small bowel and terminal ileal thickening. He was induced with 6 cycles of bendamustine-rituximab combination therapy and maintained on rituximab. A re-staging scan at 27 months showed no evidence of disease progression.
Discussion: We present a case of MCL presenting as MLP with symptoms of anemia, diarrhea and epigastric pain. MCL is a rare B-cell non-Hodgkin's lymphoma that portends a poor prognosis, making early identification and diagnosis critical. Obstruction, GI bleeding, and perforation are common complications for MCL presenting as MLP. It is important to keep MLP on the differential when multiple small nodular or polypoid lesions are identified on colonoscopy. All different types of polyps should be resected or sampled during colonoscopy, and each evaluated by the pathologist to avoid missing clinically significant conditions. Early diagnosis is key to prevent morbidity and mortality in MLP as described in our case.
Disclosures:
Sophia Pimpinelli, MD1, Abhishek Bhurwal, MD2, Tae Yang Park, MD1, Mahmoud A. Ali, MBBCh2, Steven Brant, MD1, Anish Vinit Patel, MD2. D0288 - Mantle Cell Lymphoma Presenting as Multiple Lymphomatous Polyposis: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Rutgers Robert Wood Johnson University Hospital, New Brunswick, NJ; 2Rutgers Robert Wood Johnson University Hospital- New Brunswick, New Brunswick, NJ
Introduction: Mantle Cell Lymphoma (MCL) typically presents with extensive lymphadenopathy, fevers, night sweats and unintentional weight loss. However, Multiple Lymphomatous Polyposis (MLP), MCL arising from the gastrointestinal tract, is an aggressive malignancy and is infrequently described.
Case Description/Methods: A 68-year-old Caucasian man with atrial fibrillation and hypertension presented to the hospital with watery diarrhea, fatigue and intermittent epigastric pain for the past several weeks. He denied melena, hematochezia, heartburn, dysphagia, odynophagia, weight loss, loss of appetite, NSAID use, recent travel or sick contacts. There was no family history of gastrointestinal malignancy. No history of prior endoscopic evaluation. Physical exam was notable for brown stool on rectal exam. Further evaluation revealed Hgb 6.4, MCV 60.9, iron 43, TIBC 442 and iron saturation 10% consistent with iron deficiency anemia. Upper endoscopy was normal. Colonoscopy showed eight 6-16 mm polyps scattered throughout the colon, all of which were resected completely. Analysis showed a range of histology – 3 tubular adenomas, 1 serrated and 2 hyperplastic polyps. However, histology of 4 polypoid appearing lesions (Fig 1A) showed prominent nodular atypical submucosal lymphoid aggregates (Fig 1B) that were positive for CD20, cyclin D1, weak CD5, and negative for CD10 and CD23. This was consistent with the diagnosis of MCL. CT imaging showed diffuse lymphadenopathy, including bulky disease with a 16.6 x 10.6 cm small bowel mesenteric mass (Fig 1C), along with proximal small bowel and terminal ileal thickening. He was induced with 6 cycles of bendamustine-rituximab combination therapy and maintained on rituximab. A re-staging scan at 27 months showed no evidence of disease progression.
Discussion: We present a case of MCL presenting as MLP with symptoms of anemia, diarrhea and epigastric pain. MCL is a rare B-cell non-Hodgkin's lymphoma that portends a poor prognosis, making early identification and diagnosis critical. Obstruction, GI bleeding, and perforation are common complications for MCL presenting as MLP. It is important to keep MLP on the differential when multiple small nodular or polypoid lesions are identified on colonoscopy. All different types of polyps should be resected or sampled during colonoscopy, and each evaluated by the pathologist to avoid missing clinically significant conditions. Early diagnosis is key to prevent morbidity and mortality in MLP as described in our case.
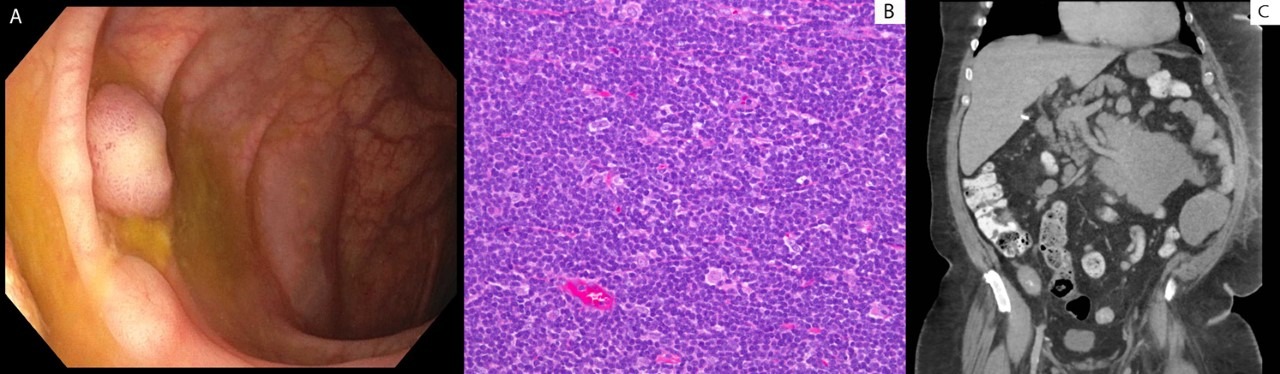
Figure: (Fig. 1A) polypoid lesion (Fig. 1B) nodular atypical submucosal lymphoid aggregates (Fig. 1C) 16.6 x 10.6 cm small bowel mesenteric mass
Disclosures:
Sophia Pimpinelli indicated no relevant financial relationships.
Abhishek Bhurwal indicated no relevant financial relationships.
Tae Yang Park indicated no relevant financial relationships.
Mahmoud Ali indicated no relevant financial relationships.
Steven Brant indicated no relevant financial relationships.
Anish Vinit Patel indicated no relevant financial relationships.
Sophia Pimpinelli, MD1, Abhishek Bhurwal, MD2, Tae Yang Park, MD1, Mahmoud A. Ali, MBBCh2, Steven Brant, MD1, Anish Vinit Patel, MD2. D0288 - Mantle Cell Lymphoma Presenting as Multiple Lymphomatous Polyposis: A Case Report, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
