Back

Poster Session D - Tuesday Morning
Category: General Endoscopy
D0292 - A Long and Dangerous Infection: Whipple’s Disease Presenting With Concurrent Candida Esophagitis and H. pylori Gastritis
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- RC
Ryan Choi, BA, MS
Edward Via College of Osteopathic Medicine
Roanoke, VA
Presenting Author(s)
Ryan Choi, BA, MS1, Alexander Pazevic, DO2, Kevin Pak, MD2, Michael Skaret, MD2, Angela Bachmann, MD2, Rashad C. Wilkerson, DO2
1Edward Via College of Osteopathic Medicine, Roanoke, VA; 2Naval Medical Center San Diego, San Diego, CA
Introduction: Whipple’s Disease (WD) is a rare condition which occurs from infection by Tropheryma whipplei. It is a debilitating illness and can lead to immunocompromise of the host. We present a case of a patient with WD who also had concomitant esophageal candidiasis and H. pylori gastritis.
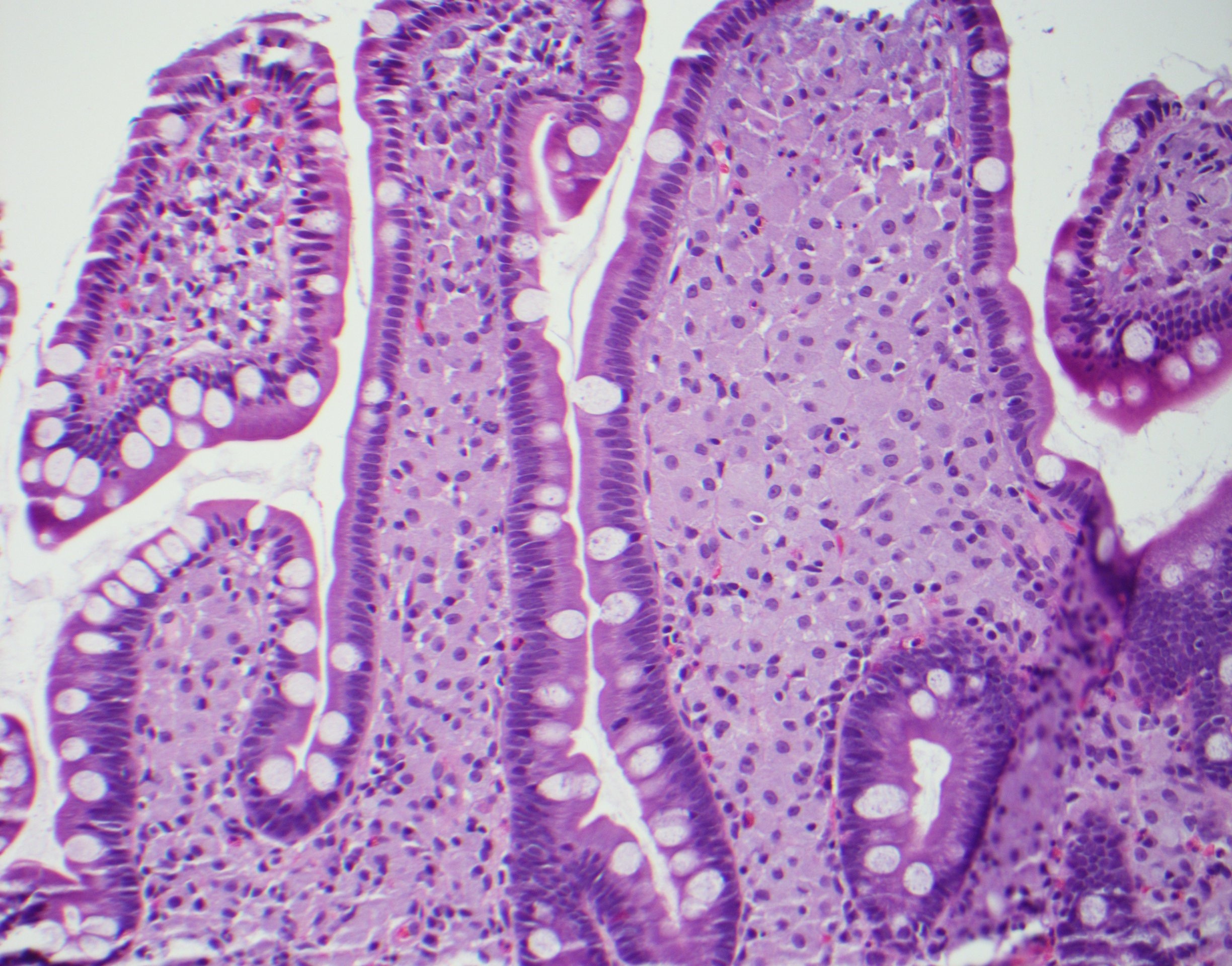
Case Description/Methods: A 36-year-old male presented with a three-month history of non-bloody diarrhea, nausea, migratory polyarthralgia, and weight-loss of 30 lbs. EGD and colonoscopy were performed. There were multiple, diminutive white plaques in the esophagus. Biopsies confirmed esophageal candidiasis. Gastric biopsies revealed H. pylori infection. The second portion of the duodenum displayed diffuse dilated lacteals with villous blunting. Similar findings were noted in the terminal ileum (TI). Biopsies of the duodenum, TI, and colon revealed foamy macrophage infiltration of the lamina propria that were intensely positive on PAS and PAS-D stains. Analysis for Tropheryma whipplei by DNA PCR was positive. He was started on ceftriaxone for WD with concurrent fluconazole for his esophageal candidiasis, which was presumed to be a complication of his immunocompromised state. Due to potential CNS and cardiac involvement, a lumbar puncture and a transthoracic echocardiogram were obtained, respectively, which were normal. After two weeks of receiving ceftriaxone, he was started on doxycycline and hydroxychloroquine with plans to continue treatment for at least one year with repeat endoscopy. His H. pylori infection was successfully treated with quadruple therapy. Three months after starting treatment, our patient had regained 20 lbs. and his other symptoms had completely resolved.
Discussion: A similar case of a patient with WD, concomitant esophageal candidiasis, and H. pylori gastritis has been reported in the literature. Both patients did not have specific risk factors for esophageal candidiasis, which supports a potential association between WD and esophageal candidiasis. The exact mechanism is unclear but may be related to the immunocompromised state of the host incurred from WD. The frequency of interval endoscopy is not defined in these patients and collaborating with infectious disease specialists to optimize follow-up is essential. Overall, WD is a rare condition that presents a diagnostic challenge, often resulting in an immunocompromised state with multisystem involvement. Long-term multidisciplinary follow-up is advisable after treatment with consideration for repeat endoscopic and histologic evaluation.
Disclosures:
Ryan Choi, BA, MS1, Alexander Pazevic, DO2, Kevin Pak, MD2, Michael Skaret, MD2, Angela Bachmann, MD2, Rashad C. Wilkerson, DO2. D0292 - A Long and Dangerous Infection: Whipple’s Disease Presenting With Concurrent Candida Esophagitis and H. pylori Gastritis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Edward Via College of Osteopathic Medicine, Roanoke, VA; 2Naval Medical Center San Diego, San Diego, CA
Introduction: Whipple’s Disease (WD) is a rare condition which occurs from infection by Tropheryma whipplei. It is a debilitating illness and can lead to immunocompromise of the host. We present a case of a patient with WD who also had concomitant esophageal candidiasis and H. pylori gastritis.
Case Description/Methods: A 36-year-old male presented with a three-month history of non-bloody diarrhea, nausea, migratory polyarthralgia, and weight-loss of 30 lbs. EGD and colonoscopy were performed. There were multiple, diminutive white plaques in the esophagus. Biopsies confirmed esophageal candidiasis. Gastric biopsies revealed H. pylori infection. The second portion of the duodenum displayed diffuse dilated lacteals with villous blunting. Similar findings were noted in the terminal ileum (TI). Biopsies of the duodenum, TI, and colon revealed foamy macrophage infiltration of the lamina propria that were intensely positive on PAS and PAS-D stains. Analysis for Tropheryma whipplei by DNA PCR was positive. He was started on ceftriaxone for WD with concurrent fluconazole for his esophageal candidiasis, which was presumed to be a complication of his immunocompromised state. Due to potential CNS and cardiac involvement, a lumbar puncture and a transthoracic echocardiogram were obtained, respectively, which were normal. After two weeks of receiving ceftriaxone, he was started on doxycycline and hydroxychloroquine with plans to continue treatment for at least one year with repeat endoscopy. His H. pylori infection was successfully treated with quadruple therapy. Three months after starting treatment, our patient had regained 20 lbs. and his other symptoms had completely resolved.
Discussion: A similar case of a patient with WD, concomitant esophageal candidiasis, and H. pylori gastritis has been reported in the literature. Both patients did not have specific risk factors for esophageal candidiasis, which supports a potential association between WD and esophageal candidiasis. The exact mechanism is unclear but may be related to the immunocompromised state of the host incurred from WD. The frequency of interval endoscopy is not defined in these patients and collaborating with infectious disease specialists to optimize follow-up is essential. Overall, WD is a rare condition that presents a diagnostic challenge, often resulting in an immunocompromised state with multisystem involvement. Long-term multidisciplinary follow-up is advisable after treatment with consideration for repeat endoscopic and histologic evaluation.
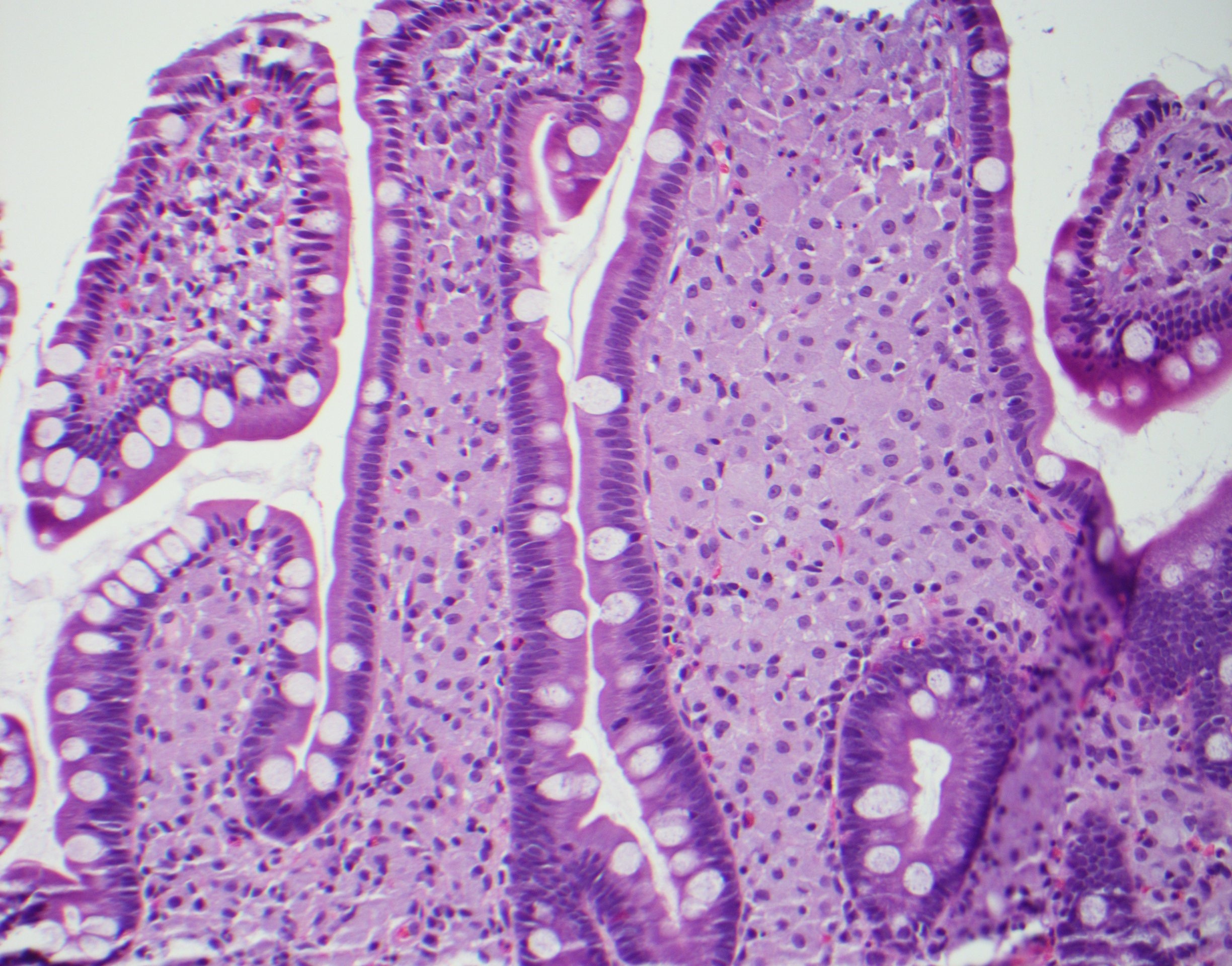
Figure: Foamy macrophages in the lamina propria, duodenum (20x)
Disclosures:
Ryan Choi indicated no relevant financial relationships.
Alexander Pazevic indicated no relevant financial relationships.
Kevin Pak indicated no relevant financial relationships.
Michael Skaret indicated no relevant financial relationships.
Angela Bachmann indicated no relevant financial relationships.
Rashad Wilkerson indicated no relevant financial relationships.
Ryan Choi, BA, MS1, Alexander Pazevic, DO2, Kevin Pak, MD2, Michael Skaret, MD2, Angela Bachmann, MD2, Rashad C. Wilkerson, DO2. D0292 - A Long and Dangerous Infection: Whipple’s Disease Presenting With Concurrent Candida Esophagitis and H. pylori Gastritis, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
