Back

Poster Session D - Tuesday Morning
Category: Esophagus
D0234 - Esophageal Epidermoid Metaplasia: A Case of a Rare Premalignant Condition
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- YR
Yasir Rajwana, MD
Jersey City Medical Center
Palo Alto, CA
Presenting Author(s)
Yasir Rajwana, MD1, Ahmed M. Ahmed, DO2, Kosisochukwu J. Ezeh, MD1, Shima Ghavimi, MD3, Etan Spira, MD1
1Jersey City Medical Center, Jersey City, NJ; 2Rutgers New Jersey Medical School, Newark, NJ; 3Marshall University, Ona, WV
Introduction: Esophageal epidermoid metaplasia (EEM) also known as esophageal leukoplakia is a rare condition with potential for malignant transformation to in-situ and invasive squamous esophageal carcinoma. It can present with symptoms of dysphagia and gastroesophageal reflux or can be found incidentally on endoscopy. Due to the relative rarity of the condition the consensus on interval for screening and modality of choice for treatment remains elusive.
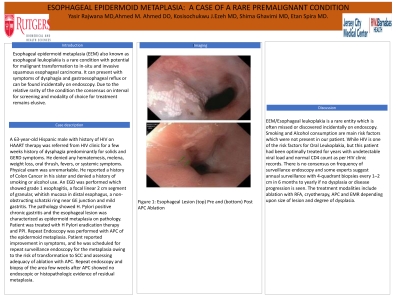
Case Description/Methods: A 63-year-old Hispanic male with history of HIV on HAART therapy was referred from HIV clinic for a few weeks history of dysphagia predominantly for solids and GERD symptoms. He denied any hematemesis, melena, weight loss, oral thrush, fevers, or systemic symptoms. Physical exam was unremarkable. He reported a history of Colon Cancer in his sister and denied a history of smoking or alcohol use. An EGD was performed which showed grade 1 esophagitis, a focal linear 2 cm segment of granular, whitish mucosa in distal esophagus, a non-obstructing schatzki ring near GE junction and mild gastritis. The pathology showed H. Pylori positive chronic gastritis and the esophageal lesion was characterized as epidermoid metaplasia on pathology. Patient was treated with H Pylori eradication therapy and PPI. Repeat Endoscopy was performed with APC of the epidermoid metaplasia. Patient reported improvement in symptoms, and he was scheduled for repeat surveillance endoscopy for the metaplasia owing to the risk of transformation to SCC and assessing adequacy of ablation with APC. Repeat endoscopy and biopsy of the area few weeks after APC showed no endoscopic or histopathologic evidence of residual metaplasia.
Discussion: EEM/Esophageal leukoplakia is a rare entity which is often missed or discovered incidentally on endoscopy. Smoking and Alcohol consumption are main risk factors which were not present in our patient. While HIV is one of the risk factors for Oral Leukoplakia, but this patient had been optimally treated for years with undetectable viral load and normal CD4 count as per HIV clinic records. There is no consensus on frequency of surveillance endoscopy and some experts suggest annual surveillance with 4-quadrant biopsies every 1–2 cm in 6 months to yearly if no dysplasia or disease progression is seen. The treatment modalities include ablation with RFA, cryotherapy, APC and EMR depending upon size of lesion and degree of dysplasia.

Disclosures:
Yasir Rajwana, MD1, Ahmed M. Ahmed, DO2, Kosisochukwu J. Ezeh, MD1, Shima Ghavimi, MD3, Etan Spira, MD1. D0234 - Esophageal Epidermoid Metaplasia: A Case of a Rare Premalignant Condition, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Jersey City Medical Center, Jersey City, NJ; 2Rutgers New Jersey Medical School, Newark, NJ; 3Marshall University, Ona, WV
Introduction: Esophageal epidermoid metaplasia (EEM) also known as esophageal leukoplakia is a rare condition with potential for malignant transformation to in-situ and invasive squamous esophageal carcinoma. It can present with symptoms of dysphagia and gastroesophageal reflux or can be found incidentally on endoscopy. Due to the relative rarity of the condition the consensus on interval for screening and modality of choice for treatment remains elusive.
Case Description/Methods: A 63-year-old Hispanic male with history of HIV on HAART therapy was referred from HIV clinic for a few weeks history of dysphagia predominantly for solids and GERD symptoms. He denied any hematemesis, melena, weight loss, oral thrush, fevers, or systemic symptoms. Physical exam was unremarkable. He reported a history of Colon Cancer in his sister and denied a history of smoking or alcohol use. An EGD was performed which showed grade 1 esophagitis, a focal linear 2 cm segment of granular, whitish mucosa in distal esophagus, a non-obstructing schatzki ring near GE junction and mild gastritis. The pathology showed H. Pylori positive chronic gastritis and the esophageal lesion was characterized as epidermoid metaplasia on pathology. Patient was treated with H Pylori eradication therapy and PPI. Repeat Endoscopy was performed with APC of the epidermoid metaplasia. Patient reported improvement in symptoms, and he was scheduled for repeat surveillance endoscopy for the metaplasia owing to the risk of transformation to SCC and assessing adequacy of ablation with APC. Repeat endoscopy and biopsy of the area few weeks after APC showed no endoscopic or histopathologic evidence of residual metaplasia.
Discussion: EEM/Esophageal leukoplakia is a rare entity which is often missed or discovered incidentally on endoscopy. Smoking and Alcohol consumption are main risk factors which were not present in our patient. While HIV is one of the risk factors for Oral Leukoplakia, but this patient had been optimally treated for years with undetectable viral load and normal CD4 count as per HIV clinic records. There is no consensus on frequency of surveillance endoscopy and some experts suggest annual surveillance with 4-quadrant biopsies every 1–2 cm in 6 months to yearly if no dysplasia or disease progression is seen. The treatment modalities include ablation with RFA, cryotherapy, APC and EMR depending upon size of lesion and degree of dysplasia.

Figure: Figure 1: Esophageal Lesion (top) Pre and (bottom) Post APC Ablation
Disclosures:
Yasir Rajwana indicated no relevant financial relationships.
Ahmed Ahmed indicated no relevant financial relationships.
Kosisochukwu Ezeh indicated no relevant financial relationships.
Shima Ghavimi indicated no relevant financial relationships.
Etan Spira indicated no relevant financial relationships.
Yasir Rajwana, MD1, Ahmed M. Ahmed, DO2, Kosisochukwu J. Ezeh, MD1, Shima Ghavimi, MD3, Etan Spira, MD1. D0234 - Esophageal Epidermoid Metaplasia: A Case of a Rare Premalignant Condition, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
