Back

Poster Session B - Monday Morning
Category: Biliary/Pancreas
B0079 - Intraductal Papillary Neoplasm of the Bile Duct Diagnosed Post Liver Transplant in Patient With Recurrent Hepatocellular Carcinoma
Monday, October 24, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Leanna Rucker, MD
MedStar Georgetown University Hospital
Washington, DC
Presenting Author(s)
Leanna Rucker, MD1, Ahmad Al-Dwairy, MD2, Dalal Alhaqqan, MD1, Amol S. Rangnekar, MD1
1MedStar Georgetown University Hospital, Washington, DC; 2MedStar Health/Georgetown-Washington Hospital Center, Washington, DC
Introduction: This case describes a patient diagnosed with metastatic intraductal papillary neoplasm of the bile duct (IPNB) during his post liver transplant course. IPNB is a rare biliary tumor characterized by papillary proliferation in the bile duct lumen. IPNBs have been mainly described in countries such as Japan, China, Korea, and Taiwan, with only 11% of cases coming from the United States. Though more favorable in prognosis than infiltrating bile duct cancer, this case demonstrates the challenge in diagnosing IPNB and its metastatic potential.
Case Description/Methods: A 67-year-old Middle Eastern male with recurrent hepatocellular carcinoma (HCC) and decompensated hepatitis C cirrhosis was referred for liver transplant evaluation. Prior HCC treatments included hepatic resection and transarterial chemoembolization and radioembolization (TACE, TARE) which were complicated by the development of biliary strictures requiring percutaneous drainage. His course was further complicated by multiple episodes of cholangitis with drug-resistant organisms. At that time, endoscopic retrograde cholangiopancreatography revealed biliary strictures that were negative for dysplasia or malignancy.
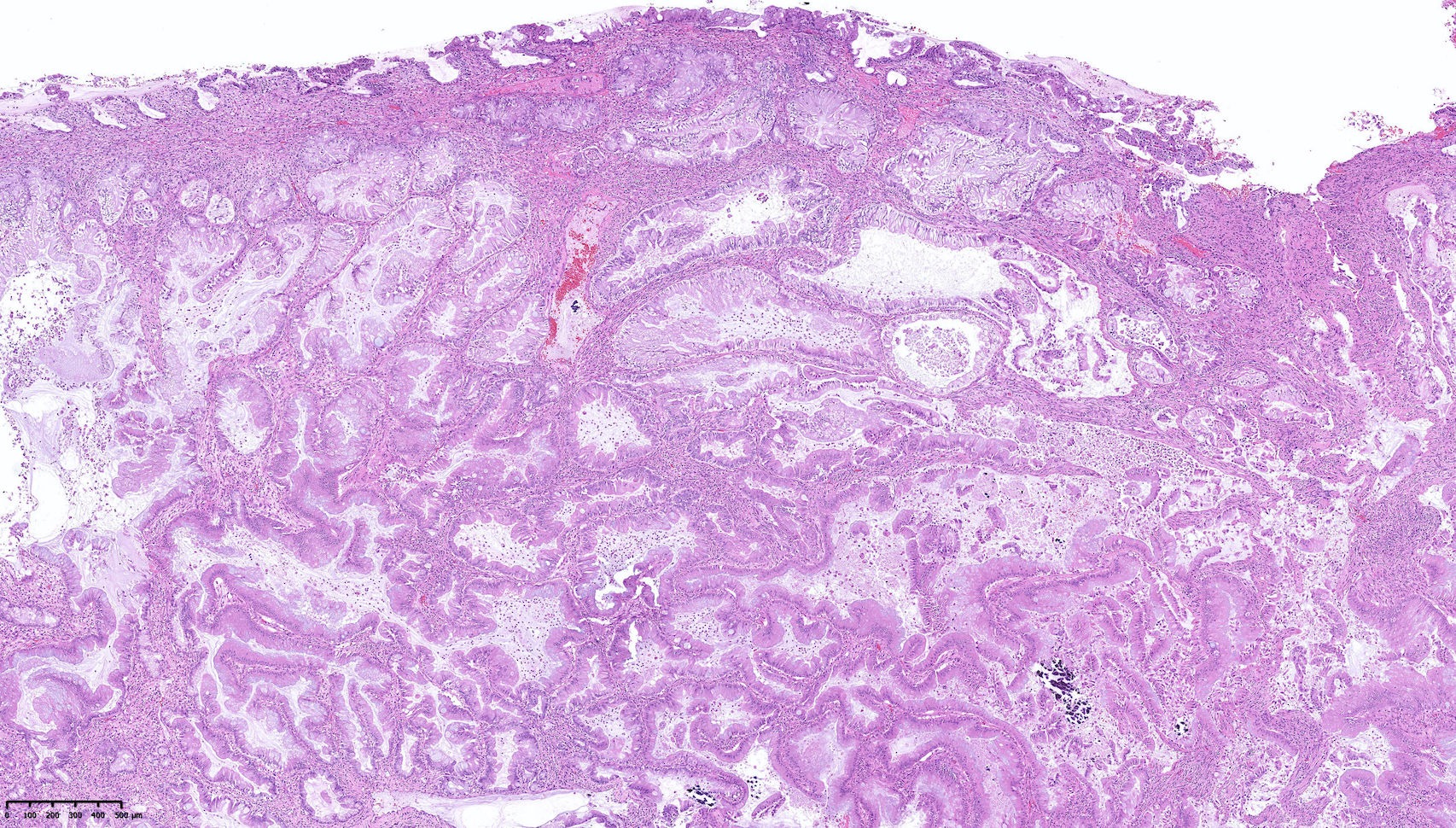
The patient ultimately underwent orthotropic liver transplant with Roux-en-Y biliary reconstruction, with intraoperative findings notable for chronic inflammation and intra-abdominal abscesses. Pathology from his native bile duct and liver revealed IPNB with mucin production, not detected on prior specimens from cholangiography. Three months later, he underwent Whipple procedure which revealed widely metastatic IPNB. Chemotherapy with gemcitabine and cisplatin was initiated.
Discussion: Though rare, IPNB has been increasingly reported in medical literature and is now recognized as its own entity with four histological subtypes. Excessive mucin production and friability of the tumor are thought to cause intermittent biliary obstruction and are responsible for its symptoms, including jaundice, abdominal pain, and cholangitis.
In our case, locally invasive IPNB was found only after bile duct explant requiring the patient to undergo a Whipple procedure following liver transplant. It is questionable whether his recurrent HCC or prior TACE and TARE procedures are linked to such tumor development. This further highlights the need to have a high index of suspicion and awareness for the elusive presentation of IPNB. It should also be considered as a potential diagnosis in patients presenting with recurrent cholangitis.
Disclosures:
Leanna Rucker, MD1, Ahmad Al-Dwairy, MD2, Dalal Alhaqqan, MD1, Amol S. Rangnekar, MD1. B0079 - Intraductal Papillary Neoplasm of the Bile Duct Diagnosed Post Liver Transplant in Patient With Recurrent Hepatocellular Carcinoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1MedStar Georgetown University Hospital, Washington, DC; 2MedStar Health/Georgetown-Washington Hospital Center, Washington, DC
Introduction: This case describes a patient diagnosed with metastatic intraductal papillary neoplasm of the bile duct (IPNB) during his post liver transplant course. IPNB is a rare biliary tumor characterized by papillary proliferation in the bile duct lumen. IPNBs have been mainly described in countries such as Japan, China, Korea, and Taiwan, with only 11% of cases coming from the United States. Though more favorable in prognosis than infiltrating bile duct cancer, this case demonstrates the challenge in diagnosing IPNB and its metastatic potential.
Case Description/Methods: A 67-year-old Middle Eastern male with recurrent hepatocellular carcinoma (HCC) and decompensated hepatitis C cirrhosis was referred for liver transplant evaluation. Prior HCC treatments included hepatic resection and transarterial chemoembolization and radioembolization (TACE, TARE) which were complicated by the development of biliary strictures requiring percutaneous drainage. His course was further complicated by multiple episodes of cholangitis with drug-resistant organisms. At that time, endoscopic retrograde cholangiopancreatography revealed biliary strictures that were negative for dysplasia or malignancy.
The patient ultimately underwent orthotropic liver transplant with Roux-en-Y biliary reconstruction, with intraoperative findings notable for chronic inflammation and intra-abdominal abscesses. Pathology from his native bile duct and liver revealed IPNB with mucin production, not detected on prior specimens from cholangiography. Three months later, he underwent Whipple procedure which revealed widely metastatic IPNB. Chemotherapy with gemcitabine and cisplatin was initiated.
Discussion: Though rare, IPNB has been increasingly reported in medical literature and is now recognized as its own entity with four histological subtypes. Excessive mucin production and friability of the tumor are thought to cause intermittent biliary obstruction and are responsible for its symptoms, including jaundice, abdominal pain, and cholangitis.
In our case, locally invasive IPNB was found only after bile duct explant requiring the patient to undergo a Whipple procedure following liver transplant. It is questionable whether his recurrent HCC or prior TACE and TARE procedures are linked to such tumor development. This further highlights the need to have a high index of suspicion and awareness for the elusive presentation of IPNB. It should also be considered as a potential diagnosis in patients presenting with recurrent cholangitis.
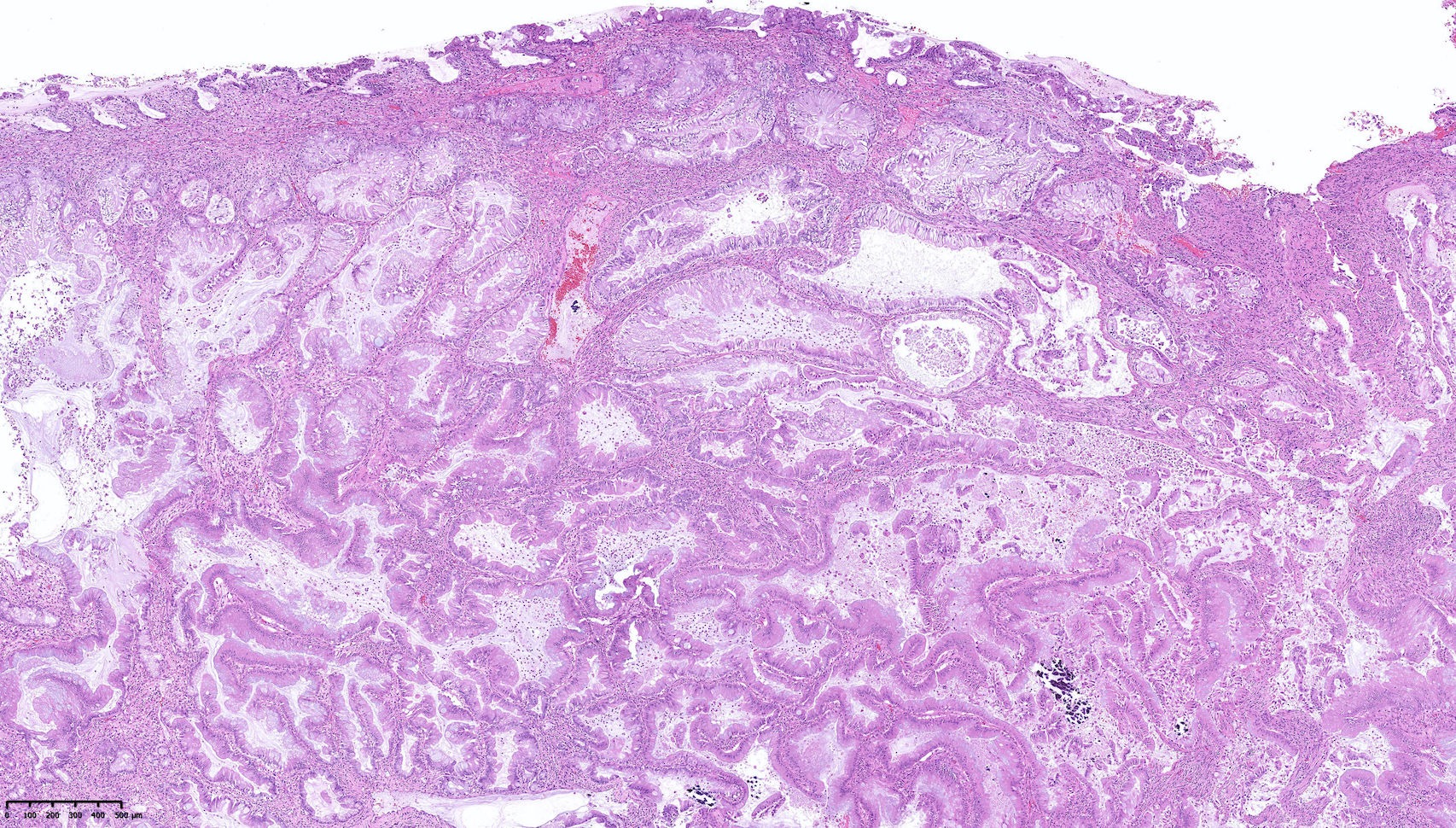
Figure: Native bile duct collection demonstrating multiple fragments of intraductal papillary neoplasm of the bile duct (IPNB) with mucin production and high-grade dysplasia (hematoxylin and eosin stain, low-power field).
Disclosures:
Leanna Rucker indicated no relevant financial relationships.
Ahmad Al-Dwairy indicated no relevant financial relationships.
Dalal Alhaqqan indicated no relevant financial relationships.
Amol Rangnekar indicated no relevant financial relationships.
Leanna Rucker, MD1, Ahmad Al-Dwairy, MD2, Dalal Alhaqqan, MD1, Amol S. Rangnekar, MD1. B0079 - Intraductal Papillary Neoplasm of the Bile Duct Diagnosed Post Liver Transplant in Patient With Recurrent Hepatocellular Carcinoma, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
