Back

Poster Session D - Tuesday Morning
Category: GI Bleeding
D0314 - A Rare Case of Ischemic Proctitis in the Setting of COVID-19
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Niloufar Alimohammadi, MD
New York University
New York, NY
Presenting Author(s)
Niloufar Alimohammadi, MD1, Mohamad I. Itani, MD2, Jessica Hélène Wells, DO3, Fazel Dinary, MD3
1New York University, New York, NY; 2Wayne State University / Detroit Medical Center, Detroit, MI; 3University Hospitals / St. John Medical Center, Westlake, OH
Introduction: The association between COVID-19 and GI symptoms has been well-established. Due to the incompletely understood pathophysiology, new GI complications are continuously reported. Ischemic proctitis (IP) is a rare complication as the rectum has excellent collateral blood supply from the rectal arteries. We present a case of an elderly patient with IP in the setting of COVID-19.
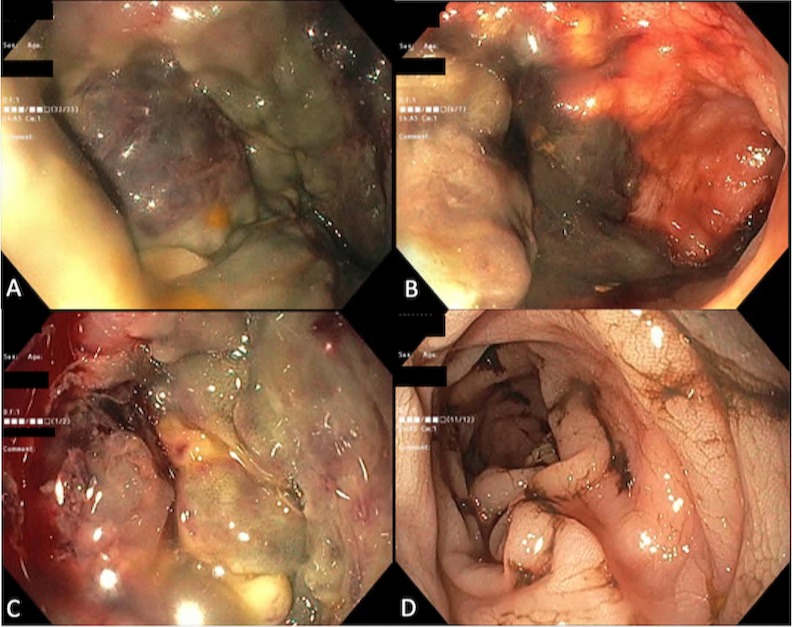
Case Description/Methods: A 66-year-old female with type 2 DM, hypertension, and GERD presented to the ED with severe shortness of breath and cough and was diagnosed with a COVID-19 infection. She was started on dexamethasone, remdesivir, therapeutic-dose enoxaparin and ceftriaxone. Her oxygen requirements increased, and she was transferred to the ICU for intubation and vasopressor support on day 4. Given a persistent decrease in hemoglobin requiring RBC and platelet transfusions on day 6, occult GI bleeding was suspected and she underwent emergent flexible sigmoidoscopy. Sigmoidoscopy showed necrotic circumferential mucosa with a large amount of blood clots starting 5cm from the anal verge and extending to 10cm in the rectum. The clots were removed, and after injection with epinephrine, no active bleeding was noted. Biopsies were taken from edges of the mucosal necrosis. The endoscope was advanced 50cm into descending colon and no active bleeding or abnormal mucosa were noted. Pathology showed marked mucosal necrosis and fibroinflammatory exudate. The patient further decompensated with superposed bacterial pneumonia, shock, AKI requiring hemodialysis, and expired one month after admission.
Discussion: COVID-19 causes a variety of respiratory symptoms in different stages of illness. Additionally, GI symptoms such as vomiting and diarrhea were linked to the virus. GI complications, such as mesenteric ischemia or ischemic colitis have also been associated with the virus due to shock and hypercoagulability. Although superficial ischemic events causing shallow mucosal ulcers are common, IP is extremely rare in the clinical setting. The protective mechanism against IP includes rectal blood supply by the inferior mesenteric, internal iliac and internal pudendal arteries. The main underlying causes of IP include severe vascular disease, acute vascular occlusion, previous vascular intervention, aorto-iliac surgery, and vasculitis. The treatment of ischemic proctitis is largely supportive but may be challenging when managing transmural rectal ischemia or gangrene, often requiring surgery and proctectomy as the definitive treatment.
Disclosures:
Niloufar Alimohammadi, MD1, Mohamad I. Itani, MD2, Jessica Hélène Wells, DO3, Fazel Dinary, MD3. D0314 - A Rare Case of Ischemic Proctitis in the Setting of COVID-19, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1New York University, New York, NY; 2Wayne State University / Detroit Medical Center, Detroit, MI; 3University Hospitals / St. John Medical Center, Westlake, OH
Introduction: The association between COVID-19 and GI symptoms has been well-established. Due to the incompletely understood pathophysiology, new GI complications are continuously reported. Ischemic proctitis (IP) is a rare complication as the rectum has excellent collateral blood supply from the rectal arteries. We present a case of an elderly patient with IP in the setting of COVID-19.
Case Description/Methods: A 66-year-old female with type 2 DM, hypertension, and GERD presented to the ED with severe shortness of breath and cough and was diagnosed with a COVID-19 infection. She was started on dexamethasone, remdesivir, therapeutic-dose enoxaparin and ceftriaxone. Her oxygen requirements increased, and she was transferred to the ICU for intubation and vasopressor support on day 4. Given a persistent decrease in hemoglobin requiring RBC and platelet transfusions on day 6, occult GI bleeding was suspected and she underwent emergent flexible sigmoidoscopy. Sigmoidoscopy showed necrotic circumferential mucosa with a large amount of blood clots starting 5cm from the anal verge and extending to 10cm in the rectum. The clots were removed, and after injection with epinephrine, no active bleeding was noted. Biopsies were taken from edges of the mucosal necrosis. The endoscope was advanced 50cm into descending colon and no active bleeding or abnormal mucosa were noted. Pathology showed marked mucosal necrosis and fibroinflammatory exudate. The patient further decompensated with superposed bacterial pneumonia, shock, AKI requiring hemodialysis, and expired one month after admission.
Discussion: COVID-19 causes a variety of respiratory symptoms in different stages of illness. Additionally, GI symptoms such as vomiting and diarrhea were linked to the virus. GI complications, such as mesenteric ischemia or ischemic colitis have also been associated with the virus due to shock and hypercoagulability. Although superficial ischemic events causing shallow mucosal ulcers are common, IP is extremely rare in the clinical setting. The protective mechanism against IP includes rectal blood supply by the inferior mesenteric, internal iliac and internal pudendal arteries. The main underlying causes of IP include severe vascular disease, acute vascular occlusion, previous vascular intervention, aorto-iliac surgery, and vasculitis. The treatment of ischemic proctitis is largely supportive but may be challenging when managing transmural rectal ischemia or gangrene, often requiring surgery and proctectomy as the definitive treatment.
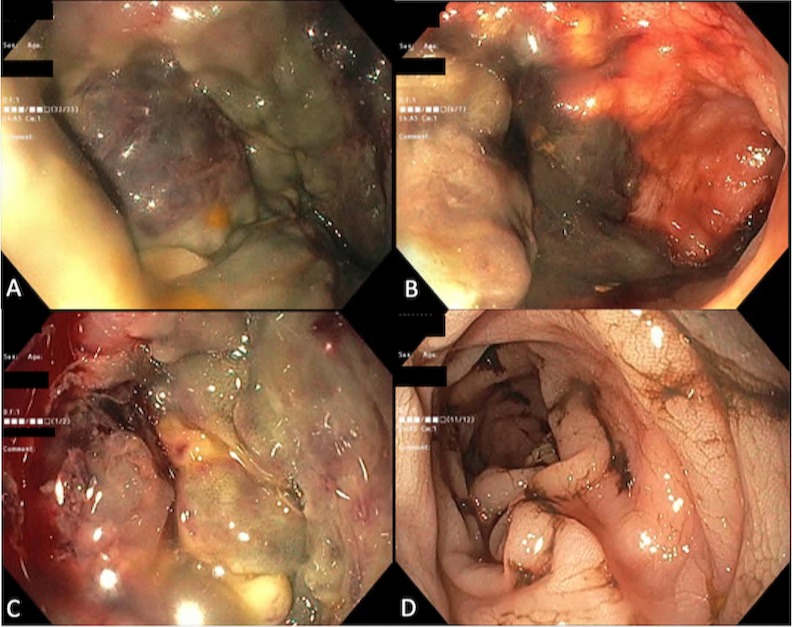
Figure: Endoscopic imaging showing mucosal necrosis of the rectum (A) with visible blood clots (B); mucosal necrosis extending to the rectosigmoid junction (C) without apparent necrosis of the sigmoid (D).
Disclosures:
Niloufar Alimohammadi indicated no relevant financial relationships.
Mohamad I. Itani indicated no relevant financial relationships.
Jessica Hélène Wells indicated no relevant financial relationships.
Fazel Dinary indicated no relevant financial relationships.
Niloufar Alimohammadi, MD1, Mohamad I. Itani, MD2, Jessica Hélène Wells, DO3, Fazel Dinary, MD3. D0314 - A Rare Case of Ischemic Proctitis in the Setting of COVID-19, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
