Back

Poster Session D - Tuesday Morning
Category: GI Bleeding
D0316 - Isolated Renal Cell Carcinoma Metastasis Presenting as a Crated Gastric Ulcer
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Arsh Momin, MD
Penn State Health Milton S. Hershey Medical Center
Hummelstown, PA
Presenting Author(s)
Arsh Momin, MD1, John Erikson L. Yap, MD2, Matthew R. Powell, MD3, Zain A. Sobani, MD4, Kenneth J. Vega, MD, FACG2, Viveksandeep Chandrasekar, MBBS2
1Penn State Health Milton S. Hershey Medical Center, Hummelstown, PA; 2Augusta University Medical College of Georiga, Augusta, GA; 3Medical College of Georgia, Augusta, GA; 4Augusta University/Medical College of Georgia, Augusta, GA
Introduction: Metastatic lesions in the stomach are rare, with autopsy studies showing < 1% rate of involvement. We report a case of recurrent renal cell carcinoma (RCC) in a patient, in remission for 8 years, presenting as an oozing gastric ulcer and celiac lymphadenopathy.
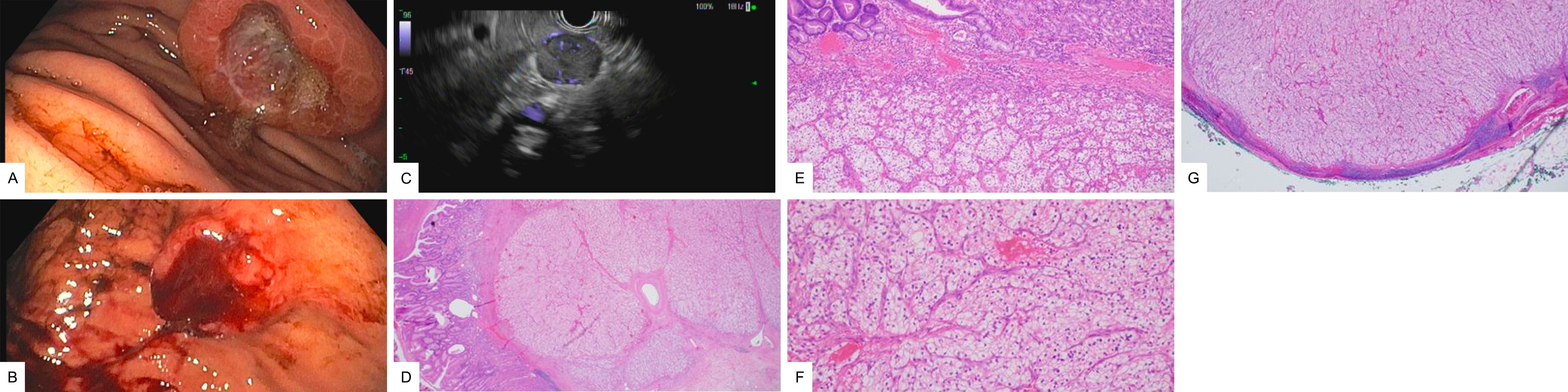
Case Description/Methods: A 66-year-old male with past medical history of RCC post laparoscopic left nephrectomy 8 years ago and hypertension presented to the outpatient clinic with iron deficiency anemia (IDA). Patient’s last colonoscopy, 7 months ago, was normal aside from adenomatous polyps. A computed tomography (CT) scan for RCC surveillance from 6 months ago showed a 20x18 mm lymph node around the celiac axis. Interventional radiology (IR) guided biopsy of it was inconclusive. A PET-CT showed a 24x22 mm lymph node adjacent to the celiac axis with hypermetabolic activity, concerning for nodal metastasis. An EGD with endoscopic ultrasound guided (EUS) lymph node biopsy was performed showing a 20x20 mm cratered ulcerated, friable mass in the mid-gastric body along the greater curvature with oozing post biopsy requiring Hemospray (Cook Medical, Bloomington, IN) for hemostasis (Figures A,B). EUS showed an 19x17 mm ill-defined, hypoechoic, heterogenous gastric body mass involving all layers to the muscularis propria. There was a 25x20 mm well defined hypoechoic lymph node in the celiac region with vascularity within it (Figure C). Fine needle biopsy (FNB) was performed but inconclusive. However, ulcer biopsy revealed metastatic RCC.
Patient underwent partial gastrectomy with retroperitoneal lymph node excision. Pathology from the excised gastric mass showed a clear cell neoplasm interfacing with gastric mucosa and high power images revealed a nested neoplasm with clear cytoplasm, a delicate capillary network and atypical nuclei consistent with metastatic RCC (Figures D,E,F). The same neoplasm was also identified in the excised celiac lymph node (Figure G). Patient is currently undergoing outpatient chemotherapy and doing well without evidence of residual disease.
Discussion: Gastric metastasis from RCC is very rare and seen in 0.2% of cases. The median time from RCC diagnosis to gastric metastasis in the literature is 7.6 years and can present with GI bleeding/IDA. It is associated with metastasis to other organs with poor prognosis but fortunately our patient did not have other organs involved. Surgical resection of symptomatic solitary metastasis is recommended.
Disclosures:
Arsh Momin, MD1, John Erikson L. Yap, MD2, Matthew R. Powell, MD3, Zain A. Sobani, MD4, Kenneth J. Vega, MD, FACG2, Viveksandeep Chandrasekar, MBBS2. D0316 - Isolated Renal Cell Carcinoma Metastasis Presenting as a Crated Gastric Ulcer, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Penn State Health Milton S. Hershey Medical Center, Hummelstown, PA; 2Augusta University Medical College of Georiga, Augusta, GA; 3Medical College of Georgia, Augusta, GA; 4Augusta University/Medical College of Georgia, Augusta, GA
Introduction: Metastatic lesions in the stomach are rare, with autopsy studies showing < 1% rate of involvement. We report a case of recurrent renal cell carcinoma (RCC) in a patient, in remission for 8 years, presenting as an oozing gastric ulcer and celiac lymphadenopathy.
Case Description/Methods: A 66-year-old male with past medical history of RCC post laparoscopic left nephrectomy 8 years ago and hypertension presented to the outpatient clinic with iron deficiency anemia (IDA). Patient’s last colonoscopy, 7 months ago, was normal aside from adenomatous polyps. A computed tomography (CT) scan for RCC surveillance from 6 months ago showed a 20x18 mm lymph node around the celiac axis. Interventional radiology (IR) guided biopsy of it was inconclusive. A PET-CT showed a 24x22 mm lymph node adjacent to the celiac axis with hypermetabolic activity, concerning for nodal metastasis. An EGD with endoscopic ultrasound guided (EUS) lymph node biopsy was performed showing a 20x20 mm cratered ulcerated, friable mass in the mid-gastric body along the greater curvature with oozing post biopsy requiring Hemospray (Cook Medical, Bloomington, IN) for hemostasis (Figures A,B). EUS showed an 19x17 mm ill-defined, hypoechoic, heterogenous gastric body mass involving all layers to the muscularis propria. There was a 25x20 mm well defined hypoechoic lymph node in the celiac region with vascularity within it (Figure C). Fine needle biopsy (FNB) was performed but inconclusive. However, ulcer biopsy revealed metastatic RCC.
Patient underwent partial gastrectomy with retroperitoneal lymph node excision. Pathology from the excised gastric mass showed a clear cell neoplasm interfacing with gastric mucosa and high power images revealed a nested neoplasm with clear cytoplasm, a delicate capillary network and atypical nuclei consistent with metastatic RCC (Figures D,E,F). The same neoplasm was also identified in the excised celiac lymph node (Figure G). Patient is currently undergoing outpatient chemotherapy and doing well without evidence of residual disease.
Discussion: Gastric metastasis from RCC is very rare and seen in 0.2% of cases. The median time from RCC diagnosis to gastric metastasis in the literature is 7.6 years and can present with GI bleeding/IDA. It is associated with metastasis to other organs with poor prognosis but fortunately our patient did not have other organs involved. Surgical resection of symptomatic solitary metastasis is recommended.
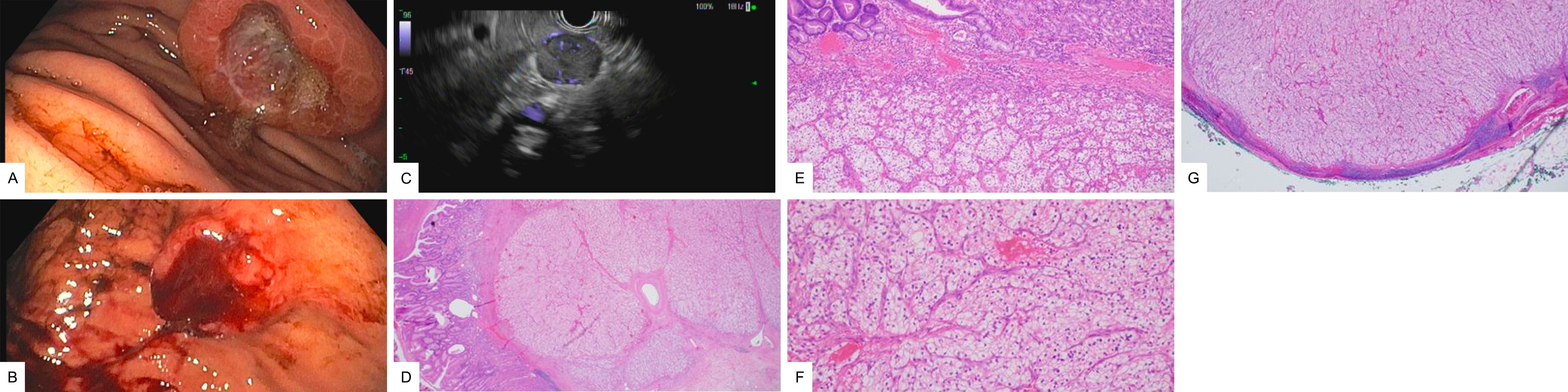
Figure: A - Esophagogastroduodenoscopy (EGD) showing a well-defined crated ulcerated mass along the greater curvature
B - Ulcer oozing after biopsies
C - Endoscopic ultrasound (EUS) demonstrating a 25 x 20 mm well-defined, hypoechoic lymph node in the celiac region
D & E - Pathology of the stomach showing clear cell neoplasm with gastric mucosa
F - High power showing neoplasm with clear cytoplasm, a delicate capillary network, and atypical nuclei
G - Pathology consistent with clear cell renal cell carcinoma
B - Ulcer oozing after biopsies
C - Endoscopic ultrasound (EUS) demonstrating a 25 x 20 mm well-defined, hypoechoic lymph node in the celiac region
D & E - Pathology of the stomach showing clear cell neoplasm with gastric mucosa
F - High power showing neoplasm with clear cytoplasm, a delicate capillary network, and atypical nuclei
G - Pathology consistent with clear cell renal cell carcinoma
Disclosures:
Arsh Momin indicated no relevant financial relationships.
John Erikson Yap indicated no relevant financial relationships.
Matthew Powell indicated no relevant financial relationships.
Zain Sobani indicated no relevant financial relationships.
Kenneth Vega indicated no relevant financial relationships.
Viveksandeep Chandrasekar indicated no relevant financial relationships.
Arsh Momin, MD1, John Erikson L. Yap, MD2, Matthew R. Powell, MD3, Zain A. Sobani, MD4, Kenneth J. Vega, MD, FACG2, Viveksandeep Chandrasekar, MBBS2. D0316 - Isolated Renal Cell Carcinoma Metastasis Presenting as a Crated Gastric Ulcer, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
