Back

Poster Session D - Tuesday Morning
Category: GI Bleeding
D0317 - Rectal Dieulafoy's Lesion Presenting as Massive Hematochezia With a Characteristic Endoscopic Appearance
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Elise Le Cam, MD, MS
University of Arizona
Tucson, AZ
Presenting Author(s)
Elise Le Cam, MD, MS, Amar Vedamurthy, MD, MSCI, MRCP, Avin Aggarwal, MD
University of Arizona, Tucson, AZ
Introduction: Dieulafoy's lesions (DLs) are a rare cause of gastrointestinal (GI) bleeding, accounting for an estimated 2% of all acute GI bleeding cases. Furthermore, DLs are often found in the stomach and the esophagus, with rectal DLs being uncommon. We present the case of an older male patient, with history of previous cardiac arrest and acute kidney injury, who experienced massive hematochezia from a rectal Dieulafoy’s lesion.
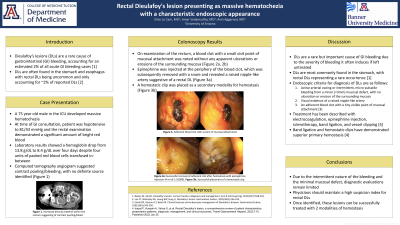
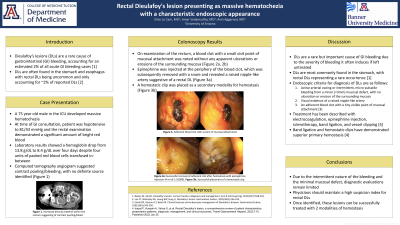
Case Description/Methods: A 75-year-old male in the medical intensive care unit (ICU) developed painless massive hematochezia. The patient was initially admitted after being found down and had a complicated hospital course. At the time of consultation, large clots per rectum were reported, which subsequently converted to bright red bleeding. The day before GI evaluation, the patient’s blood pressures were hypertensive to 155/66 mmHg, but subsequently dropped significantly to 81/43 mmHg. The rectal examination demonstrated a significant amount of bright red blood. Laboratory results showed a hemoglobin drop from 13.8 g/dL to 8.4 g/dL over four days despite four units of packed red blood cells transfused in-between. Computed tomography angiogram suggested contrast pooling/bleeding, with no definite source identified (Figure 1).
The colonoscopy demonstrated extensive diverticulosis without any signs of active bleeding. On examination of the rectum, a blood clot with a small visible point of mucosal attachment was noted without any apparent ulcerations or erosions of the surrounding mucosa (Figure 2a,2b). Epinephrine was injected at the periphery of the blood clot, which was subsequently removed with a snare, and revealed a raised nipple-like artery suggestive of a rectal Dieulafoy's lesion (Figure 3a). A hemostatic clip was placed as a secondary modality for hemostasis (Figure 3b). The patient was observed in the ICU and remained hemodynamically stable. He had no further episodes of hematochezia and no re-bleeding.
Discussion: Dieulafoy's lesions are a rare but important cause of GI bleeding due to the severity of bleeding it often induces if left untreated. They are most commonly found in the stomach and the esophagus but can rarely present in the rectum. Due to the intermittent nature of the bleeding and the minimal mucosal defect, diagnostic evaluations remain limited. Our case demonstrates a classic endoscopic appearance of rectal DLs, which requires careful inspection during withdrawal. Once identified, these lesions can be successfully treated with two modalities of hemostasis.

Disclosures:
Elise Le Cam, MD, MS, Amar Vedamurthy, MD, MSCI, MRCP, Avin Aggarwal, MD. D0317 - Rectal Dieulafoy's Lesion Presenting as Massive Hematochezia With a Characteristic Endoscopic Appearance, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
University of Arizona, Tucson, AZ
Introduction: Dieulafoy's lesions (DLs) are a rare cause of gastrointestinal (GI) bleeding, accounting for an estimated 2% of all acute GI bleeding cases. Furthermore, DLs are often found in the stomach and the esophagus, with rectal DLs being uncommon. We present the case of an older male patient, with history of previous cardiac arrest and acute kidney injury, who experienced massive hematochezia from a rectal Dieulafoy’s lesion.
Case Description/Methods: A 75-year-old male in the medical intensive care unit (ICU) developed painless massive hematochezia. The patient was initially admitted after being found down and had a complicated hospital course. At the time of consultation, large clots per rectum were reported, which subsequently converted to bright red bleeding. The day before GI evaluation, the patient’s blood pressures were hypertensive to 155/66 mmHg, but subsequently dropped significantly to 81/43 mmHg. The rectal examination demonstrated a significant amount of bright red blood. Laboratory results showed a hemoglobin drop from 13.8 g/dL to 8.4 g/dL over four days despite four units of packed red blood cells transfused in-between. Computed tomography angiogram suggested contrast pooling/bleeding, with no definite source identified (Figure 1).
The colonoscopy demonstrated extensive diverticulosis without any signs of active bleeding. On examination of the rectum, a blood clot with a small visible point of mucosal attachment was noted without any apparent ulcerations or erosions of the surrounding mucosa (Figure 2a,2b). Epinephrine was injected at the periphery of the blood clot, which was subsequently removed with a snare, and revealed a raised nipple-like artery suggestive of a rectal Dieulafoy's lesion (Figure 3a). A hemostatic clip was placed as a secondary modality for hemostasis (Figure 3b). The patient was observed in the ICU and remained hemodynamically stable. He had no further episodes of hematochezia and no re-bleeding.
Discussion: Dieulafoy's lesions are a rare but important cause of GI bleeding due to the severity of bleeding it often induces if left untreated. They are most commonly found in the stomach and the esophagus but can rarely present in the rectum. Due to the intermittent nature of the bleeding and the minimal mucosal defect, diagnostic evaluations remain limited. Our case demonstrates a classic endoscopic appearance of rectal DLs, which requires careful inspection during withdrawal. Once identified, these lesions can be successfully treated with two modalities of hemostasis.

Figure: Figure 1: Arterial phase imaging demonstrating increased density material within the rectum (demarcated by green arrow), suggestive of contrast pooling/bleed. No definite source was identified. Figure 2a, 2b: Adherent blood clot with a point of mucosal attachment. Figure 3a: Successful removal of adherent clot after hemostasis with epinephrine injection (4 ml of 1:10000). Figure 3b: Successful placement of a hemostatic clip.
Disclosures:
Elise Le Cam indicated no relevant financial relationships.
Amar Vedamurthy indicated no relevant financial relationships.
Avin Aggarwal indicated no relevant financial relationships.
Elise Le Cam, MD, MS, Amar Vedamurthy, MD, MSCI, MRCP, Avin Aggarwal, MD. D0317 - Rectal Dieulafoy's Lesion Presenting as Massive Hematochezia With a Characteristic Endoscopic Appearance, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
