Back

Poster Session D - Tuesday Morning
Category: GI Bleeding
D0324 - Massive Hematemesis: A Case of Esophageal-Subclavian Fistula
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio
- NC
Nicole Cornet, MD
New York-Presbyterian Hospital/Weill Cornell Medicine
New York, NY
Presenting Author(s)
Nicole Cornet, MD1, Preston Atteberry, MD1, Suzanne Elshafey, MD2, Carl Crawford, MD3
1New York-Presbyterian Hospital/Weill Cornell Medicine, New York, NY; 2New York Presbyterian-Weill Cornell Medical Center, Manhattan, NY; 3New York-Presbyterian Hospital/Weill Cornell Medical College, New York, NY
Introduction: Esophageal-subclavian fistulae are rare and are most commonly seen as a complication of congenital aortic arch anomalies. We report a case of an esophageal-subclavian fistula in a patient with a right aortic arch with an aberrant left subclavian artery (ALSA), an uncommon anatomical variant that occurs in approximately 1% of the general population.
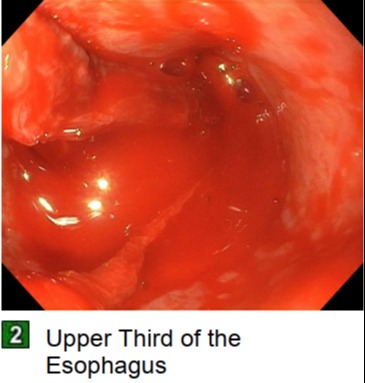
Case Description/Methods: A 76-year-old man with atrial fibrillation, prior pulmonary embolism, and hyperthyroidism with a multinodular goiter presented to an outside hospital (OSH) after being found down at home. He was intubated for acute hypoxic respiratory failure at the OSH, and transferred to our center for resection of the multinodular goiter causing airway compression. His postoperative course was complicated by multiple infections and prolonged intubation. CT imaging incidentally noted a four vessel aortic arch with retroesophageal ALSA. Two months into the hospitalization, he had large volume hematemesis and subsequent cardiac arrest requiring multiple rounds of resuscitation and Blakemore tube placement into the esophagus. Upon deflation of the Blakemore, he coded again and was started on massive transfusion protocol before successfully deflating the device. Emergent endoscopy was notable for clotted blood in the stomach and active, pulsatile bleeding of the proximal esophagus (25cm), concerning for arterio-esophageal fistula. Thoracic surgery, cardiac surgery, and vascular surgery were consulted; however, given overall poor prognosis and high risk with invasive surgery, no operative intervention was offered. He was ultimately transitioned to comfort care.
Discussion: While arterial-esophageal fistulae are rare, it is important to recognize these cases early as they can lead to fatal hemorrhage if not surgically intervened upon. In the case of ALSA, the vessel takes a retroesophageal course and often forms a dilated segment at the proximal end, called a diverticulum of Kommerell, which compresses the esophagus posteriorly. The vascular pressure on the esophagus can ultimately create a fistula. Prolonged use of indwelling devices, such as nasogastric tubes (NGT) and endotracheal tubes (ETT), may create pressure necrosis and erosion of the posterior esophageal wall, thus contributing to fistula formation. While there are currently no guidelines for screening for aortic arch abnormalities, it has been suggested that those with aortic arch abnormalities noted on CT imaging may benefit from avoidance of prolonged use of NGT or ETT.
Disclosures:
Nicole Cornet, MD1, Preston Atteberry, MD1, Suzanne Elshafey, MD2, Carl Crawford, MD3. D0324 - Massive Hematemesis: A Case of Esophageal-Subclavian Fistula, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1New York-Presbyterian Hospital/Weill Cornell Medicine, New York, NY; 2New York Presbyterian-Weill Cornell Medical Center, Manhattan, NY; 3New York-Presbyterian Hospital/Weill Cornell Medical College, New York, NY
Introduction: Esophageal-subclavian fistulae are rare and are most commonly seen as a complication of congenital aortic arch anomalies. We report a case of an esophageal-subclavian fistula in a patient with a right aortic arch with an aberrant left subclavian artery (ALSA), an uncommon anatomical variant that occurs in approximately 1% of the general population.
Case Description/Methods: A 76-year-old man with atrial fibrillation, prior pulmonary embolism, and hyperthyroidism with a multinodular goiter presented to an outside hospital (OSH) after being found down at home. He was intubated for acute hypoxic respiratory failure at the OSH, and transferred to our center for resection of the multinodular goiter causing airway compression. His postoperative course was complicated by multiple infections and prolonged intubation. CT imaging incidentally noted a four vessel aortic arch with retroesophageal ALSA. Two months into the hospitalization, he had large volume hematemesis and subsequent cardiac arrest requiring multiple rounds of resuscitation and Blakemore tube placement into the esophagus. Upon deflation of the Blakemore, he coded again and was started on massive transfusion protocol before successfully deflating the device. Emergent endoscopy was notable for clotted blood in the stomach and active, pulsatile bleeding of the proximal esophagus (25cm), concerning for arterio-esophageal fistula. Thoracic surgery, cardiac surgery, and vascular surgery were consulted; however, given overall poor prognosis and high risk with invasive surgery, no operative intervention was offered. He was ultimately transitioned to comfort care.
Discussion: While arterial-esophageal fistulae are rare, it is important to recognize these cases early as they can lead to fatal hemorrhage if not surgically intervened upon. In the case of ALSA, the vessel takes a retroesophageal course and often forms a dilated segment at the proximal end, called a diverticulum of Kommerell, which compresses the esophagus posteriorly. The vascular pressure on the esophagus can ultimately create a fistula. Prolonged use of indwelling devices, such as nasogastric tubes (NGT) and endotracheal tubes (ETT), may create pressure necrosis and erosion of the posterior esophageal wall, thus contributing to fistula formation. While there are currently no guidelines for screening for aortic arch abnormalities, it has been suggested that those with aortic arch abnormalities noted on CT imaging may benefit from avoidance of prolonged use of NGT or ETT.
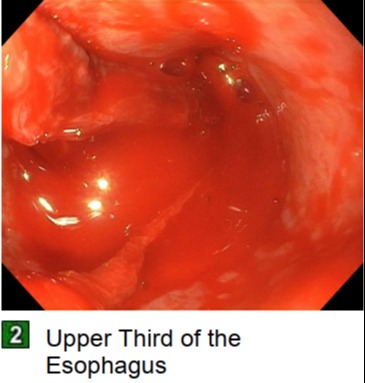
Figure: Endoscopy image showing upper third of the esophagus with profuse, active bleeding.
Disclosures:
Nicole Cornet indicated no relevant financial relationships.
Preston Atteberry indicated no relevant financial relationships.
Suzanne Elshafey indicated no relevant financial relationships.
Carl Crawford indicated no relevant financial relationships.
Nicole Cornet, MD1, Preston Atteberry, MD1, Suzanne Elshafey, MD2, Carl Crawford, MD3. D0324 - Massive Hematemesis: A Case of Esophageal-Subclavian Fistula, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
