Back

Poster Session D - Tuesday Morning
Category: GI Bleeding
D0331 - An Unusual Case of Upper GI Bleeding in the Setting of Injection Drug Use
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Mohammed Rifat Shaik, MBBS
University of Maryland Medical Center Midtown Campus
Baltimore, MD
Presenting Author(s)
Mohammed Rifat Shaik, MBBS1, Nishat Anjum Shaik, MBBS2, Elvina Yunasan, MD1, Erika Wheeler, MD3, Yuting Huang, MD, PhD1, Robert T. Chow, MD, MBA1
1University of Maryland Medical Center Midtown Campus, Baltimore, MD; 2Guntur Medical College, Guntur, Andhra Pradesh, India; 3University of Maryland Medical Center, Baltimore, MD
Introduction: Autoimmune and chronic inflammatory or infectious disorders increase the risk of developing systemic AA amyloidosis. Renal and cardiac involvement is most common, followed by the nervous system, soft tissues, lungs, and liver. Gastrointestinal (GI) involvement is uncommon and often asymptomatic, leading to a delayed diagnosis. Here we present a patient with history of injection drug use who presented with hemoglobin (Hgb) decline from ongoing occult GI bleed. This prompted endoscopy, leading to a diagnosis of GI amyloidosis.
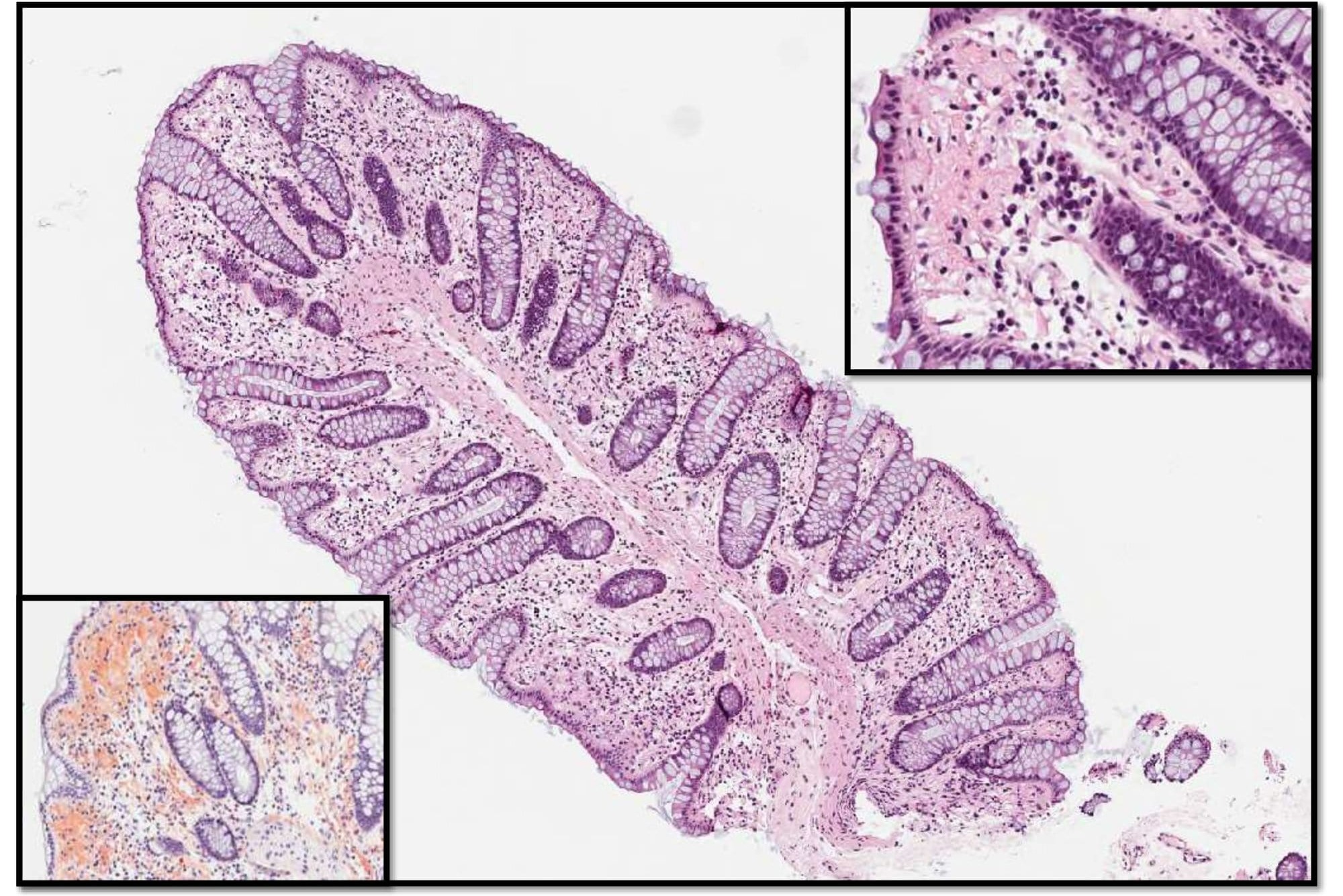
Case Description/Methods: A 37-year-old woman with a longstanding history of injection drug use was admitted with sepsis secondary to infection of chronic, non-healing forearm wounds. Her hospital course was complicated by a Hgb decline to 6.1 from 9 g/dL mandating transfusion support with 6 PRBCs to maintain her Hgb > 7 g/dL. She denied hematemesis, melena, or hematochezia. CT angiography indicated no obvious source of bleeding in the abdomen or pelvis. Upper GI endoscopy revealed erythematous, friable gastric mucosa, and duodenal mucosal atrophy. Colonoscopy revealed grossly normal but friable mucosa. Gastric, duodenal, and colonic biopsies showed extensive amyloid deposition in the lamina propria confirmed with Congo red stain (see figure). Mass spectrometry was positive for amyloid A. She was discharged on Pantoprazole, and responded well.
Discussion: GI amyloidosis is defined as the presence of GI symptoms with direct biopsy verification. Its incidence is 3%. ALλ was the most amyloid type (53%) whereas AA was least common (10%). AL usually deposits in the muscularis mucosae, submucosa and muscularis propria as massive deposits causing polypoid protrusions and thickened folds while the AA deposits in the lamina propria as granular deposits leading to mucosal friability. As a result, malabsorption and fecal occult blood are common in AA amyloidosis (like in our patient), whereas AL amyloidosis presents with mechanical obstruction and chronic intestinal pseudo obstruction. Since amyloidosis has a poor prognosis, early diagnosis is crucial. Endoscopic biopsy confirms the diagnosis with duodenal specimens having the highest diagnostic yield. Endoscopy is ineffectual in the management of bleeding, hence there are currently no guidelines for endoscopic treatment. Symptomatic relief is the focus. Definitive management entails treating the underlying cause (drug rehabilitation in this case).
Disclosures:
Mohammed Rifat Shaik, MBBS1, Nishat Anjum Shaik, MBBS2, Elvina Yunasan, MD1, Erika Wheeler, MD3, Yuting Huang, MD, PhD1, Robert T. Chow, MD, MBA1. D0331 - An Unusual Case of Upper GI Bleeding in the Setting of Injection Drug Use, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1University of Maryland Medical Center Midtown Campus, Baltimore, MD; 2Guntur Medical College, Guntur, Andhra Pradesh, India; 3University of Maryland Medical Center, Baltimore, MD
Introduction: Autoimmune and chronic inflammatory or infectious disorders increase the risk of developing systemic AA amyloidosis. Renal and cardiac involvement is most common, followed by the nervous system, soft tissues, lungs, and liver. Gastrointestinal (GI) involvement is uncommon and often asymptomatic, leading to a delayed diagnosis. Here we present a patient with history of injection drug use who presented with hemoglobin (Hgb) decline from ongoing occult GI bleed. This prompted endoscopy, leading to a diagnosis of GI amyloidosis.
Case Description/Methods: A 37-year-old woman with a longstanding history of injection drug use was admitted with sepsis secondary to infection of chronic, non-healing forearm wounds. Her hospital course was complicated by a Hgb decline to 6.1 from 9 g/dL mandating transfusion support with 6 PRBCs to maintain her Hgb > 7 g/dL. She denied hematemesis, melena, or hematochezia. CT angiography indicated no obvious source of bleeding in the abdomen or pelvis. Upper GI endoscopy revealed erythematous, friable gastric mucosa, and duodenal mucosal atrophy. Colonoscopy revealed grossly normal but friable mucosa. Gastric, duodenal, and colonic biopsies showed extensive amyloid deposition in the lamina propria confirmed with Congo red stain (see figure). Mass spectrometry was positive for amyloid A. She was discharged on Pantoprazole, and responded well.
Discussion: GI amyloidosis is defined as the presence of GI symptoms with direct biopsy verification. Its incidence is 3%. ALλ was the most amyloid type (53%) whereas AA was least common (10%). AL usually deposits in the muscularis mucosae, submucosa and muscularis propria as massive deposits causing polypoid protrusions and thickened folds while the AA deposits in the lamina propria as granular deposits leading to mucosal friability. As a result, malabsorption and fecal occult blood are common in AA amyloidosis (like in our patient), whereas AL amyloidosis presents with mechanical obstruction and chronic intestinal pseudo obstruction. Since amyloidosis has a poor prognosis, early diagnosis is crucial. Endoscopic biopsy confirms the diagnosis with duodenal specimens having the highest diagnostic yield. Endoscopy is ineffectual in the management of bleeding, hence there are currently no guidelines for endoscopic treatment. Symptomatic relief is the focus. Definitive management entails treating the underlying cause (drug rehabilitation in this case).
Figure: This low power image of a colon biopsy shows increased deposition of an amorphous pink material within the lamina propria, which can be more easily seen at higher magnification (see inset, upper right, 20x). A Congo red special stain confirms the amorphous material is comprised of amyloid protein (see inset, orange coloring, bottom left).
Disclosures:
Mohammed Rifat Shaik indicated no relevant financial relationships.
Nishat Anjum Shaik indicated no relevant financial relationships.
Elvina Yunasan indicated no relevant financial relationships.
Erika Wheeler indicated no relevant financial relationships.
Yuting Huang indicated no relevant financial relationships.
Robert Chow indicated no relevant financial relationships.
Mohammed Rifat Shaik, MBBS1, Nishat Anjum Shaik, MBBS2, Elvina Yunasan, MD1, Erika Wheeler, MD3, Yuting Huang, MD, PhD1, Robert T. Chow, MD, MBA1. D0331 - An Unusual Case of Upper GI Bleeding in the Setting of Injection Drug Use, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
