Back

Poster Session D - Tuesday Morning
Category: GI Bleeding
D0334 - Sometimes You Have to “Dig a Little Deeper:” A Case of a Dieulafoy Lesion Leading to a Life-Threatening Gastrointestinal Bleed in a 30-Year-Old Male
Tuesday, October 25, 2022
10:00 AM – 12:00 PM ET
Location: Crown Ballroom
Has Audio

Andy Sam, DO
Palmetto General Hospital
Hialeah, FL
Presenting Author(s)
Andy Sam, DO1, Melissa Matheus, MD1, Emmanuel McDonald, DO2, Karthik Mohan, DO1
1Palmetto General Hospital, Hialeah, FL; 2Larkin Community Hospital, Hialeah, FL
Introduction: Dieulafoy's lesion is a relatively rare, but potentially life-threatening condition accounting for 1-2% of acute GI bleeds. Scrupulous operator techniques during upper endoscopy are critical for the detection of Dieulafoy's lesions and may decrease the mortality from 80% to 8.6%.
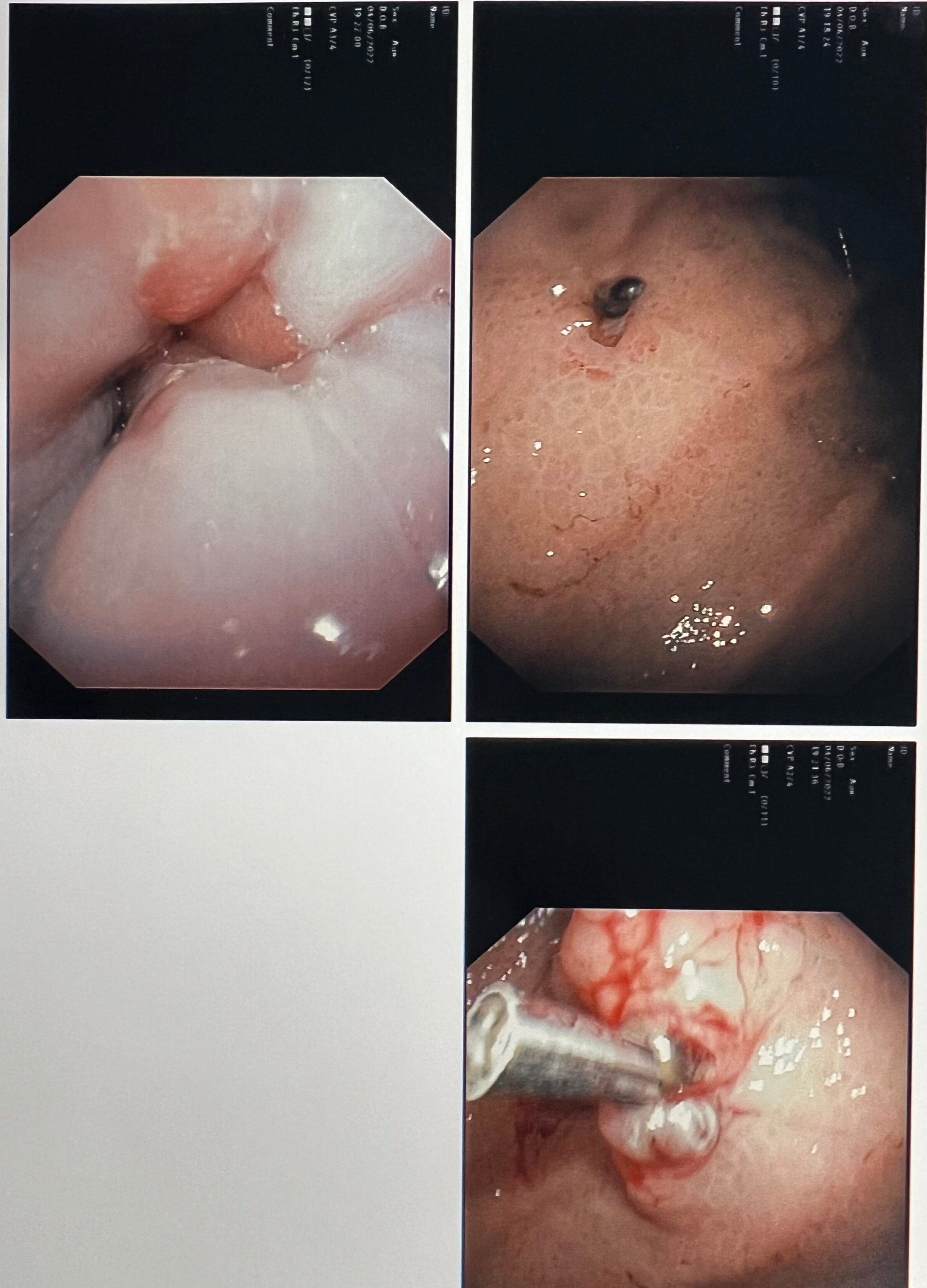
Case Description/Methods: A 30-year-old Hispanic male with a past medical history of ischemic cardiomyopathy, chronic anemia and uncontrolled hypertension which led to ESRD presents to our hospital due to melena and new onset hematemesis. He reports that a week prior he had presented to a facility with epigastric abdominal pain and symptomatic anemia requiring one unit of blood. An initial upper endoscopy at that time revealed gastritis and duodenitis with no sequelae of bleeding. Upon presentation, hemoglobin was 3.7mg/dl for which the patient was emergently transfused. CTA of abdomen revealed what appeared to be active arterial extravasation involving the region of the body of the stomach. An emergent upper endoscopy was performed which after proper insufflation showed a Dieulafoy lesion in the lesser curvature of the stomach. Lesion was subsequently injected with epinephrine and one hemoclip was placed. Patient later remained hemodynamically stable throughout the rest of his hospitalization.
Discussion: Dieulafoy's lesion is a large caliber aberrant submucosal vessel that erodes through overlying epithelium. It is a rare but well known cause of potential life threatening gastrointestinal hemorrhage. Enhanced blood flow through the enlarged artery may cause hypoperfusion, ischemia, and erosion of overlying mucosa. It is more prevalent in males with cardiopulmonary and/or renal failure comorbidities such as our patient's case. It is also considered one of the most under-recognized conditions due to its difficulty in diagnosis. Upper endoscopy is effective in diagnosing up to 70% of cases, however in some cases it may be overlooked. Factors that may lead to a missed diagnosis are excessive blood, small size of the lesion, poor insufflation during endoscopy, intermittent activity or unusual location such as the jejunum or ileum. When EGD and colonoscopy are non-specific, a push enteroscopy or wireless capsule may have a higher yield. If a gastrointestinal approach is not successful, we can also consider alternative treatments such as angiography and/or surgery. When encountering an obscure cause of life threatening gastrointestinal bleed, a Dieulafoy’s lesion must remain in our differential.
Disclosures:
Andy Sam, DO1, Melissa Matheus, MD1, Emmanuel McDonald, DO2, Karthik Mohan, DO1. D0334 - Sometimes You Have to “Dig a Little Deeper:” A Case of a Dieulafoy Lesion Leading to a Life-Threatening Gastrointestinal Bleed in a 30-Year-Old Male, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
1Palmetto General Hospital, Hialeah, FL; 2Larkin Community Hospital, Hialeah, FL
Introduction: Dieulafoy's lesion is a relatively rare, but potentially life-threatening condition accounting for 1-2% of acute GI bleeds. Scrupulous operator techniques during upper endoscopy are critical for the detection of Dieulafoy's lesions and may decrease the mortality from 80% to 8.6%.
Case Description/Methods: A 30-year-old Hispanic male with a past medical history of ischemic cardiomyopathy, chronic anemia and uncontrolled hypertension which led to ESRD presents to our hospital due to melena and new onset hematemesis. He reports that a week prior he had presented to a facility with epigastric abdominal pain and symptomatic anemia requiring one unit of blood. An initial upper endoscopy at that time revealed gastritis and duodenitis with no sequelae of bleeding. Upon presentation, hemoglobin was 3.7mg/dl for which the patient was emergently transfused. CTA of abdomen revealed what appeared to be active arterial extravasation involving the region of the body of the stomach. An emergent upper endoscopy was performed which after proper insufflation showed a Dieulafoy lesion in the lesser curvature of the stomach. Lesion was subsequently injected with epinephrine and one hemoclip was placed. Patient later remained hemodynamically stable throughout the rest of his hospitalization.
Discussion: Dieulafoy's lesion is a large caliber aberrant submucosal vessel that erodes through overlying epithelium. It is a rare but well known cause of potential life threatening gastrointestinal hemorrhage. Enhanced blood flow through the enlarged artery may cause hypoperfusion, ischemia, and erosion of overlying mucosa. It is more prevalent in males with cardiopulmonary and/or renal failure comorbidities such as our patient's case. It is also considered one of the most under-recognized conditions due to its difficulty in diagnosis. Upper endoscopy is effective in diagnosing up to 70% of cases, however in some cases it may be overlooked. Factors that may lead to a missed diagnosis are excessive blood, small size of the lesion, poor insufflation during endoscopy, intermittent activity or unusual location such as the jejunum or ileum. When EGD and colonoscopy are non-specific, a push enteroscopy or wireless capsule may have a higher yield. If a gastrointestinal approach is not successful, we can also consider alternative treatments such as angiography and/or surgery. When encountering an obscure cause of life threatening gastrointestinal bleed, a Dieulafoy’s lesion must remain in our differential.
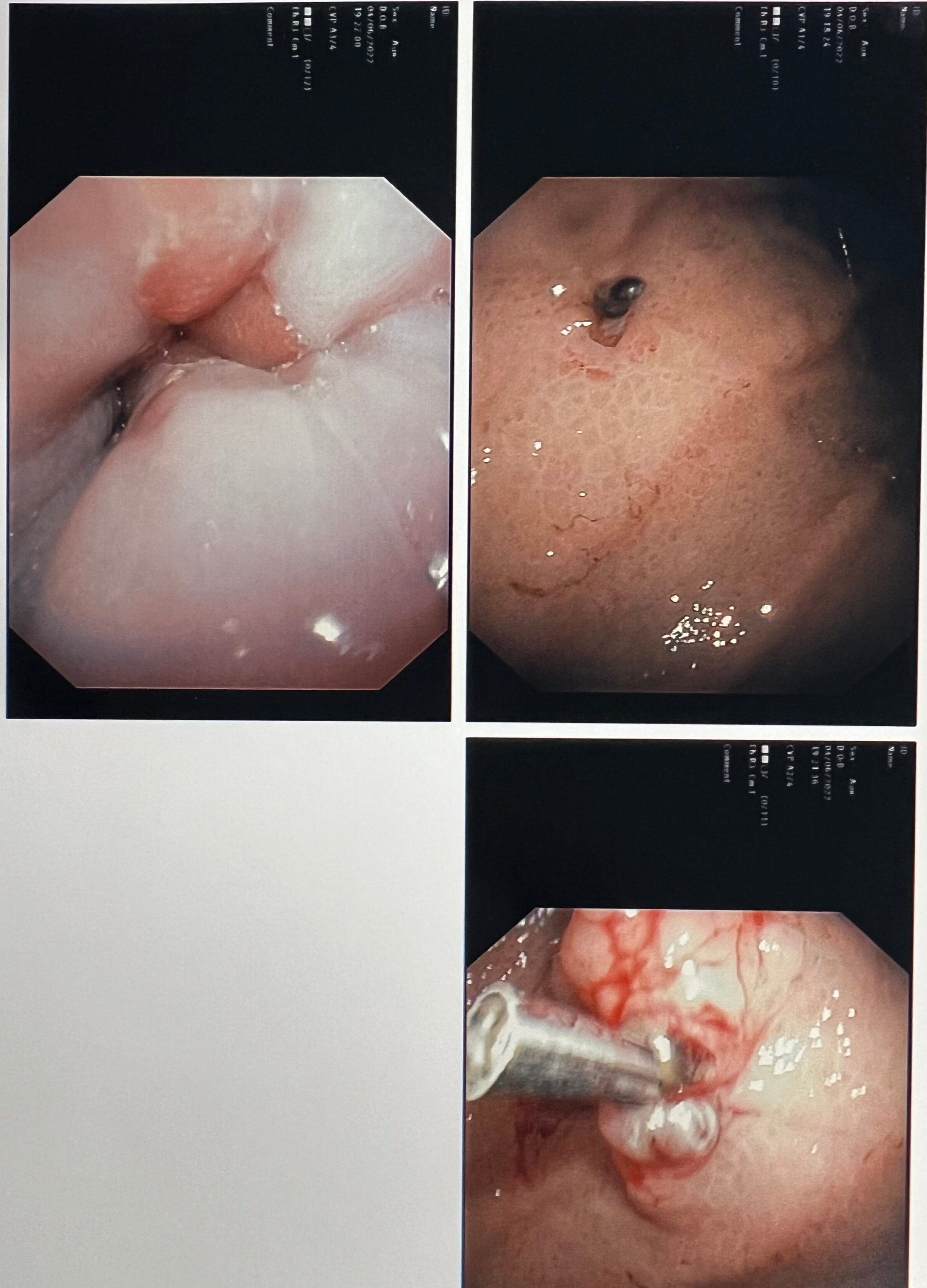
Figure: Figure 1. (Upper right image) Large caliber (Dieulafoy Lesion) protruding through the mucosal wall in the lesser curvature of the stomach. (Right lower image) Dieulafoy lesion after epinephrine and hemoclip hemostatic treatment.
Disclosures:
Andy Sam indicated no relevant financial relationships.
Melissa Matheus indicated no relevant financial relationships.
Emmanuel McDonald indicated no relevant financial relationships.
Karthik Mohan indicated no relevant financial relationships.
Andy Sam, DO1, Melissa Matheus, MD1, Emmanuel McDonald, DO2, Karthik Mohan, DO1. D0334 - Sometimes You Have to “Dig a Little Deeper:” A Case of a Dieulafoy Lesion Leading to a Life-Threatening Gastrointestinal Bleed in a 30-Year-Old Male, ACG 2022 Annual Scientific Meeting Abstracts. Charlotte, NC: American College of Gastroenterology.
